CLINICAL CASE
REVISTA DE LA FACULTAD DE MEDICINA HUMANA 2024 - Universidad Ricardo Palma10.25176/RFMH.v24i1.5973
MILIARY TUBERCULOSIS IN AN IMMUNOCOMPETENT PATIENT: CASE REPORT
TUBERCULOSIS MILIAR EN PACIENTE INMUNOCOMPETENTE: REPORTE DE CASO
Renzo Steffano Valle Farfan
 1,a
1,a
Alejandro Manuel Peña Villalobos
 1,a
1,a
Walter Jesus Espinoza Hernandez
 1,a
1,a
Steffano Alessandro Valle Farfan
 2,b
2,b
1 Clínica San Pablo. Surco. Lima-Peru.
2 Faculty of Human Medicine. Universidad Científica del Sur. Lima-Peru.
a Pulmonologist
b Human Medicine student
ABSTRACT
Miliary Tuberculosis (TB) is a potentially fatal condition if not diagnosed and treated promptly,
although it requires certain circumstances to develop. This article studies the case of a 48-year-old
man with no significant pathological history, who developed the disease over a period of six months,
initially presenting with diffuse gastrointestinal symptoms. One month prior to admission, he developed
progressive respiratory symptoms and was admitted to the emergency department where bilateral diffuse
miliary involvement was evident on the chest computed tomography. He was administered oxygen and support
measures and passed an HIV test, which was negative. Nevertheless, his sputum smear microscopy showed
positive results. His clinical evolution remained stationary until the administration of
antituberculosis therapy, observing slight clinical improvement. Low doses of corticosteroids were also
administered, leading to a favorable evolution, and he was subsequently discharged.
Keywords: Tuberculosis, miliary, respiratory insufficiency, corticosteroids (Source: MeSH).
RESUMEN
La tuberculosis (TB) miliar es una presentación con un desenlace fatal de no ser diagnosticada ni
tratada a tiempo; para desarrollar esta presentación se requieren de ciertas condicionantes. En este
artículo, se estudia el caso de un varón de 48 años sin antecedentes patológicos, quien inició la
enfermedad por un periodo de seis meses, con un cuadro gastrointestinal difuso inicial; un mes antes del
ingreso presentó un cuadro respiratorio progresivo, por lo que fue ingresado a Emergencias, en donde se
evidenció, en la tomografía computarizada de tórax, compromiso miliar difuso bilateral; se le administró
oxígeno y medidas de soporte, se obtuvo prueba VIH, cuyo resultado fue negativo. Se obtuvieron
resultados positivos en la baciloscopia de esputo. Su evolución fue estacionaria hasta la administración
de la terapia antituberculosa y se observó leve mejoría clínica; así mismo, se le administraron dosis
bajas de corticoide, luego de los cuales se evidenció una evolución favorable, por lo que se le dio de
alta.
Palabras clave: Tuberculosis miliar, insuficiencia respiratoria, corticoesteroides (Fuente:
DeCS).
INTRODUCTION
Tuberculosis (TB) continues to be a significant global health concern, with the COVID-19 pandemic having
a detrimental effect on access to diagnosis, treatment, and disease burden. In 2021, an estimated of
10.6 million people fell ill with TB, which represented a 4.5% increase from 2020. In the same year, 1.4
million deaths were reported among HIV-seronegative individuals (1). In
Peru, the Directorate of Tuberculosis Prevention and Control (DPCTB, by its Spanish acronym) reported an
incidence rate of 60.1 per 100,000 inhabitants in 2022 (2). Miliary TB is a
lethal form of disseminated TB, resulting from massive lymphohematogenous dissemination of a
Mycobacterium tuberculosis-laden focus (3), occurring either during primary
mycobacterial infection or upon reactivation of a latent infection (5). The
dissemination usually results from erosion into a blood vessel and the release of caseating material
from any bodily focus. In an individual with low immunity, this leads to the seeding of small, often
caseating granulomas resembling millet grains, that is why they are called miliary (4). Various predisposing or associated conditions have been documented in
miliary TB patients, including childhood infections, malnutrition, HIV/AIDS, alcoholism, chronic renal
disease, dialysis, post-gastrectomy state, organ transplantation, use of immunosuppressive drugs,
connective tissue disorders, pregnancy, postpartum period, underlying malignant tumors, and silicosis
(6).
CASE REPORT
The patient, a 48-year-old male mechanic in the mining industry with no significant medical history,
presented six months before admission with diffuse abdominal pain, progressive abdominal distension, and
weight loss of approximately 10 kilograms. Therefore, he initially visited an outpatient
Gastroenterology clinic, where he was diagnosed with ascites and was scheduled for a procedure, which he
did not attend due to personal reasons. Two months later, he was re-evaluated by a specialist who
informed him that the ascites had resolved. It is important to note that one month prior to hospital
admission, the patient experienced sporadic dry cough associated with progressive dyspnea, and one week
before admission, the dyspnea worsened even with mild efforts. Additionally, he presented with febrile
episodes and headache, which led him to consult a company doctor. There, an oxygen saturation of 70% was
identified, prompting his transfer to the emergency clinic.
Upon physical examination at admission, the patient had an oxygen saturation of 95% at FiO2 of 21%,
generalized pallor, tachypnea, use of accessory muscles for breathing, and a slightly distended but
non-painful abdomen; the rest of the physical examination was within normal ranges. Laboratory tests
showed hemoglobin: 13.5 gr/dL, hematocrit: 43%, total leukocytes: 9.64, total proteins: 5.75 g/dL,
alkaline phosphatase: 75, total bilirubin: 0.45, indirect bilirubin: 0.26, direct bilirubin: 0.19, with
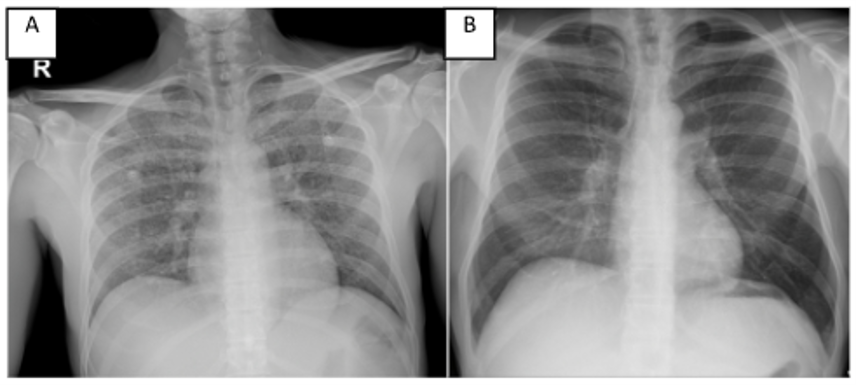
tumor markers: CA 21-1 and carcinoembryonic antigen negative and HIV negative. Imaging studies revealed
a bilateral diffuse micronodular pattern in the chest X-ray upon admission (Figure 1); the same pattern
was observed in the chest computed tomography at admission, with no evidence of pleural effusion or
lymphadenopathy (Figure 2).
During his hospitalization, the patient showed poor clinical evolution and increased respiratory effort,
leading to his transfer to the Intensive Care Unit, where he received oxygen support through a binasal
cannula. After positive sputum smear microscopy results for Mycobacterium tuberculosis, specific
treatment was initiated. Two weeks into the treatment, a slight improvement was noted compared to his
condition upon admission, but there was a worsening in the control tomography (Figure 2), along with
persistent tachypnea and oxygen supplementation. Consequently, corticosteroid therapy was initiated,
leading to significant improvement in the respiratory pattern within a week, and he was transferred to a
non-critical patient hospitalization ward.
Following the progressive weaning from mechanical ventilation and gradual reduction of corticosteroids,
as well as tolerance to the antituberculosis treatment, the patient was discharged 21 days after
hospitalization. Three months into the treatment, during a follow-up, he was in phase 2, showing
evidence of improvement in the control tomography image.
DISCUSSION
Miliary TB is a deadly form of TB resulting from massive lymphohematogenous dissemination of a
Mycobacterium tuberculosis-laden focus. Radiologically, the miliary pattern has been defined as "a
collection of tiny, discrete pulmonary opacities that are generally uniform in size and broadly
distributed”; each one measures 2 mm or less in diameter (6). This pattern
involves the simultaneous compromise of multiple organs and is more common in extreme ages of life, in
both infants, young children, and elderly individuals with debilitating conditions (4). Organs with high blood flow, such as the spleen, liver, lungs, bone
marrow, kidneys, and adrenal glands, are frequently affected. On macroscopic examination, the lesions
are rounded, grey to reddish-brown, small, punctate, and more or less uniform in size. They can be
observed in the lungs and several other organs. The "tubercle" is the histopathological hallmark of
miliary tuberculosis. When miliary tuberculosis results from an acute massive hematogenous spread,
lesions in all viscera appear similar: "soft" or "exudative" tubercles; a clear caseous focus invading
blood vessels is usually demonstrable, and the lesions often reveal acid-fast bacillus (AFB). This can
develop at the time of primary infection or later, during the reactivation of a latent focus (3). In the vast majority, the host's immune responses are capable of
containing the primary infection, leading either to complete healing or persistence as a latent
infection. However, in 10% of patients, the immune response is insufficient to contain the primary
infection, resulting in dissemination (5). Miliary tuberculosis is believed
to result from inadequate effector T-cell (Teff) responses to contain the tuberculous bacillus; evidence
suggests that selective chemokine-directed Th2 cell responses may play a critical role in the
development of miliary TB. In a susceptible host, immune responses lean towards a protective inhibitory
Th2 response, such as granuloma formation, and this inability to limit local disease activity favors
dissemination. Miliary TB likely results from a Th2-biased response that occurs as a predetermined
pathway (6).
The predominant constitutional symptoms include anorexia, weight loss, and fever, the latter being the
most common symptom. About 75-80% of patients experience an early morning peak in fever. Gradual onset
of malaise and weight loss occurs in 60-65% of individuals; cough and difficulty breathing are seen in
50% of cases. Abdominal pain is the main symptom in about 7-14% of patients with miliary TB. Headache,
observed in 10-15% of cases, suggests meningeal involvement (5); night
sweats are common, leaving a silhouette-like sweat mark on the bed, similar to a wet shadow (wet shadow
sign) (6). Some authors have discussed the concept of cryptic miliary TB
(6, 8), defined as a form of disseminated TB with a
non-miliary pattern or normal chest radiography, plus one of the following conditions: positive culture
for M. tuberculosis from bone marrow, liver biopsy sample, or in two or more non-contiguous organs; and
positive culture for M. tuberculosis from one organ and histopathological demonstration of caseating
granulomas from another non-contiguous organ (7). Regarding pulmonary
involvement evidenced in radiology, the predominant finding in miliary TB are diffuse nodules between
1-3 mm with random distribution (8); Kim et al. showed that the number of
small nodules and micronodules in HIV-positive patients was greater than in HIV-negative patients, and
ground-glass attenuation was identified in 14 (93%) of 15 HIV-positive patients and nine (64%) of 14
HIV-negative patients. In our patient, diffuse micronodular lesions predominantly bibasal without
secondary TB lesions were found. In the presence of clinical suspicion compatible with miliary TB,
bacteriological confirmation should be performed, as there is a high incidence of this disease in our
environment. Detection of mycobacterial isolates from a clinical sample provides a definitive diagnosis
of disseminated tuberculosis. Examples of tissue samples include sputum, body fluids, tissue, and biopsy
samples (16); in our patient, a positive sputum smear confirmed the
diagnosis.
Similar case reports exist in other countries: Cueto et al. reported a case of a 38-year-old
immunocompetent male patient with miliary TB and acute respiratory failure with a fatal outcome, who
also required support with invasive mechanical ventilation (10). Likewise,
Agu et al. reported a case of a 67-year-old immunocompetent African American male with comorbidities
such as hypertension, atrial fibrillation, and prostate cancer, who, after treatment, achieved complete
remission of miliary TB (11); Echeverri-Fernandez et al. reported the case
of a 24-year-old woman without comorbidities, who, after six months of gastrointestinal and
constitutional symptoms, was diagnosed with peritoneal TB, received treatment, and was discharged after
15 days of hospitalization (12). Regarding the treatment of miliary TB, it
is uniformly fatal if untreated. Standard antituberculosis treatment is the cornerstone of management.
There is no consensus on the optimal duration of treatment in patients with miliary TB. In many parts of
the world, patients with miliary TB are treated under the National Tuberculosis Control Program with
observed short-duration chemotherapy (3).
In general, corticosteroids lead to a clinically significant reduction in mortality, regardless of the
affected organ group. The overall mortality reduction from steroid use is 17% (14); the benefit of using corticosteroids has been demonstrated, as
corticosteroids like dexamethasone inhibit the death of necrotic cells infected with Mycobacterium
tuberculosis (Mtb) and facilitate mitogen-activated protein kinase phosphatase 1 (MKP-1) dependent
dephosphorylation of p38 MAPK (13); evidence has been published supporting
the use of pulse corticosteroids in patients affected by miliary tuberculosis associated with
respiratory distress syndrome, with favorable results for this therapy (15).
CONCLUSIONS
Miliary tuberculosis is a lethal presentation if not identified and treated in time, and diagnostic
suspicion is the main tool: clinical follow-up and imaging support are important for its final
diagnosis. While it occurs more frequently in extreme ages of life and in people with predisposing
factors, it can also present in those outside these age ranges and without any risk factors. Prompt
initiation of antituberculosis treatment and support measures are the cornerstone of managing this
unique pathological presentation; the use of corticosteroids in this presentation is debatable, but in
our case, faced with poor clinical evolution, the response resulted in notable improvement, and the
patient was successfully weaned off mechanical ventilation, leading to discharge.
Authorship contributions:
Renzo Steffano Valle Farfán participated in the conception and design of the article,
collection of results, analysis and interpretation of data, writing of the article, critical
review of the article, approval of the final version, provision of patients or study
material, and obtaining funding; likewise, Alejandro Manuel Peña Villalobos, Steffano
Alessandro Valle Farfán, and Walter Jesus Espinoza Hernandez conducted the critical review
of the article and approval of the final version.
Financing:
Self-financed
Declaration of conflict of interest:
The authors declare no conflict of interest.
Recevied:
October 3, 2023
Approved:
March 14, 2024
Correspondence author:
Renzo Steffano Valle Farfan.
Address:
Calle Antonio Canova 132, San Borja, Lima-Peru.
Phone:
(+51) 970012187
E-mail:
renzo90vf@hotmail.com
Article published by the Journal of the faculty of Human Medicine of the Ricardo Palma University. It is an open access article, distributed under the terms of the Creatvie Commons license: Creative Commons Attribution 4.0 International, CC BY 4.0 (https://creativecommons.org/licenses/by/1.0/), that allows non-commercial use, distribution and reproduction in any medium, provided that the original work is duly cited. For commercial use, please contact revista.medicina@urp.edu.pe.