ORIGINAL ARTICLE
REVISTA DE LA FACULTAD DE MEDICINA HUMANA 2024 - Universidad Ricardo Palma10.25176/RFMH.v24i1.6012
CORRELATION OF HISTOPATHOLOGICAL RESULTS AND TOMOGRAPHIC FINDINGS IN PATIENTS WITH LIVER LESIONS SUSPICIOUS FOR MALIGNANCY
CORRELACIÓN DEL RESULTADO HISTOPATOLÓGICO Y HALLAZGOS TOMOGRÁFICOS EN PACIENTES CON LESIONES HEPÁTICAS SOSPECHOSAS DE MALIGNIDAD
Luis Pablo Valencia Montiel
 1,3,a
1,3,a
Jorge Roberto Hernández Santos
 2,b
2,b
Arturo García-Galicia
 1,c
1,c
Álvaro José Montiel-Jarquín
 1,d
1,d
Diana López García
 1,a
1,a
Maricarmen Tapia Venancio
 1,a
1,a
Nancy Rosalía Bertado-Ramírez
 1,f
1,f
1 Directorate of Education and Research in Health, High Specialty Medical Unit, Hospital de
Especialidades de Puebla, Centro Médico Nacional "Gral. de Div. Manuel Ávila Camacho", Instituto Mexicano
del Seguro Social, Puebla de Zaragoza, Mexico.
2 Division of Radiology, High Specialty Medical Unit, Hospital de Especialidades de Puebla,
Centro Médico Nacional "Gral. de Div. Manuel Ávila Camacho", Instituto Mexicano del Seguro Social, Puebla de
Zaragoza, Mexico.
3 Faculty of Human Medicine, Universidad Popular Autonóma del Estado de Puebla, Puebla de
Zaragoza, Mexico.
a General Physician
b Specialist in Radiology
c Specialist in Pediatrics. Master of Medical Sciences and Research
d Specialist in General Surgery. Master of Medical Sciences and Research
f Specialist in Neurology
ABSTRACT
Introduction: Liver cancer is the seventh most common neoplasm worldwide and the second cause of
mortality directly associated with cancer. In Mexico it has an incidence of 3.9% in the entire
population. Although computed tomography (CT) is the imaging study of choice, the final diagnosis is
established with the anatomopathological study of the lesion.
Objective: Correlate the tomographic findings with the histopathological result in patients with
liver lesions with suspicion of malignancy, who underwent USG-guided biopsy.
Methods: Descriptive, correlation, retrolective, homodemographic and single-center study. The
study period was from September 2021 to February 2022. Patients older than 18 years with liver lesions
suspicious of malignancy were selected and underwent Computed Axial Tomography and ultrasound-guided
biopsy. Shapiro Wilk tests (for normality) were used and chi-square was used for an analysis of
association of categorical variables.
Results: Twenty-four patients were included, who underwent Tomography and lesion biopsy, finding
an average size of lesions of 2.39cm. The results of the correlation between the tomographic diagnosis
and the definitive histopathological diagnosis did not have statistical significance p=0.069.
Conclusions: No significant correlation was found between the histopathological study and
tomographic findings in liver lesions suggestive of malignancy.
Keywords: Hepatic neoplasms; Biopsy; X-ray computed tomography. (source: MeSH-NLM)
RESUMEN
Introducción: El cáncer hepático es la séptima neoplasia más frecuente a nivel mundial y la
segunda causa de mortalidad asociada directamente a cáncer. En México presenta una incidencia del 3.9%
en toda la población. A pesar de que la tomografía axial computada es el estudio diagnóstico inicial de
elección, el diagnóstico final se establece con el estudio anatomopatológico de la lesión.
Objetivo: Correlacionar los hallazgos tomográficos con el resultado histopatológico en pacientes
con lesiones hepáticas con sospecha de malignidad, a los que se les tomó biopsia dirigida por USG.
Material y métodos: Estudio descriptivo, de correlación, retrolectivo, homodémico y unicéntrico.
El tiempo de estudio fue de septiembre 2021 a febrero 2022. Se seleccionó a pacientes mayores de 18 años
con lesiones hepáticas sospechosas de malignidad, a los que se les realizó tomografía y biopsia guiada
por ultrasonido. Se utilizó pruebas de Shapiro-Wilk (de normalidad) y se utilizó ꭕ2 para un análisis de
asociación de variables categóricas.
Resultados: Se incluyeron a 24 pacientes, a los cuales se les realizó tomografía y biopsia de
lesión, encontrando un tamaño promedio de las lesiones de 2.39cm. Los resultados de la correlación entre
el diagnóstico tomográfico y el diagnóstico histopatológico definitivo no tuvieron significancia
estadística p=0.069.
Conclusiones: No se encontró correlación significativa entre el estudio histopatológico y los
hallazgos tomográficos en lesiones hepáticas sugerentes de malignidad.
Palabras clave: Neoplasias hepáticas; Biopsia; Tomografía computarizada por rayos X. (fuente:
DeCS-BIREME)
INTRODUCTION
Liver cancer is the seventh most common neoplasm worldwide. In 2020, the World Health Organization
reported an incidence of 4.7% and it's the second leading cause of mortality (1, 2). In Latin America
and the Caribbean, the incidence is 2.7%. Mexico reports it at 3.9% in the entire population, with a
predominance in males at 4.1% (3).
The main risk factors include hepatitis B virus infection, hepatitis C virus infection, alcoholism,
non-alcoholic fatty liver disease, type 2 diabetes, obesity, and age over 60 years (6, 7). Other factors
such as systemic arterial hypertension, pancreatitis, sleep apnea, osteoarthritis, liver
transplantation, and autoimmune hepatitis are also associated with the development of liver cancer (8, 9).
The disease is initially asymptomatic. In the case of hepatocellular carcinoma, early symptoms are
associated with liver cirrhosis in over 60% of cases (10). Symptoms in advanced stages include abdominal
pain, weight loss, early satiety, palpable mass in the epigastrium, and sometimes paraneoplastic
syndromes presenting with hypoglycemia, erythrocytosis, hypercalcemia, diarrhea, and skin conditions
(10). On the other hand, cholangiocarcinoma obstructing the biliary drainage may present with abdominal
pain (50%), weight loss (40%), fever (20%), jaundice, pruritus, acholia, and stools with a reddish-brown
color. The presence of jaundice indicates advanced disease. This is the most aggressive variant of liver
cancer (11, 12).
Patients at risk for liver cancer are recommended to undergo periodic imaging studies to detect
cancerous lesions early. The American, European, and Asian Pacific associations recommend ultrasound,
serum tumor markers, and tomography in patients with cirrhosis, hepatitis B, those awaiting liver
transplantation, men over 40 years old, and women over 50 (13).
Suspicion of malignancy in a liver lesion indicates the performance of magnetic resonance imaging, which
provides clear images of the tumor and allows classification into intrahepatic or extrahepatic, and the
latter into hilar or perihilar (20).
Ultrasound (USG) has variable sensitivity and specificity, so in case of doubt or abnormal findings,
computed tomography (CT) is performed. Magnetic resonance cholangiopancreatography is performed to
define the tumor's location, extent, and other details useful for treatment (21, 22, 23).
Once the diagnosis of liver cancer is established, it is staged to plan medical and surgical treatment.
The classification proposed by the American Joint Committee on Cancer (AJCC) stages liver cancer, and
its definitions established in the 8th edition of 2017 are still in use. The AJCC is a TNM
classification where T represents the tumor size, N the presence of nodules, and M the existence of
metastasis (24, 25). The use of CT has been validated by eight associations as the first-choice
diagnostic study in suspected liver cancer, as it helps define guidelines for monitoring and medical and
surgical treatment (26, 27). However, few guidelines condition a sensitivity and specificity between CT
findings and histopathological study. Apart from this characteristic, there are no studies exploring the
correlation between tomographic findings and histopathological results in patients with liver lesions
suspicious of malignancy (28).
Materials and Methods:
An analytical, correlational study was conducted from 2021 to 2022. It was carried out on patients with
liver lesions suspected of malignancy by CT who underwent ultrasound-guided percutaneous biopsy, treated
at a tertiary hospital in Puebla, Mexico.
Patients over 18 years old with liver lesions suspected of malignancy, who also underwent biopsy of
these lesions, were included. Patients who had already received oncological treatment were excluded, and
those who requested to leave the study or died during its conduct were eliminated.
A data collection form was used to gather patient information, including variables such as sex, age,
risk factors, diagnosis by CT and histopathology, contrast enhancement phase in CT, tumor location by
CT, tumor segment affected, tumor size, and the number of days between the imaging study and biopsy.
Once patients meeting the inclusion criteria were gathered, it was obtained a convenience sample of 24
patients.
For statistical analysis, frequencies and percentages were calculated, and measures of central tendency
including mean, median, and mode, as well as measures of dispersion consisting of minimum, maximum, and
standard deviation, were used.
Shapiro-Wilk tests were used for normality, obtaining a normal distribution (p=>0.5). ꭕ2 tests were used
for an analysis of association of categorical variables, obtaining p=>0.05. A database was created in
the IBM SPSS Statistics pack version 25 statistical processor, and all variables and their results were
entered in numerical language.
The protocol was approved by the Local Health Research Committee. Patient anonymity was preserved at all
times, and the data were used solely for scientific purposes.
Results:
Out of a total population of 24 patients, it was found that 10 (41.70%) were men and 14 (58.3%) were
women, with a mean age of 57.54 years.
The mean number of days between the performance of both studies was 23.50 days with a standard deviation
of 12.56 days. The elapsed time ranged from 2 to a maximum of 50 days.
The average lesion size was 2.39cm as determined by both tomography and biopsy.
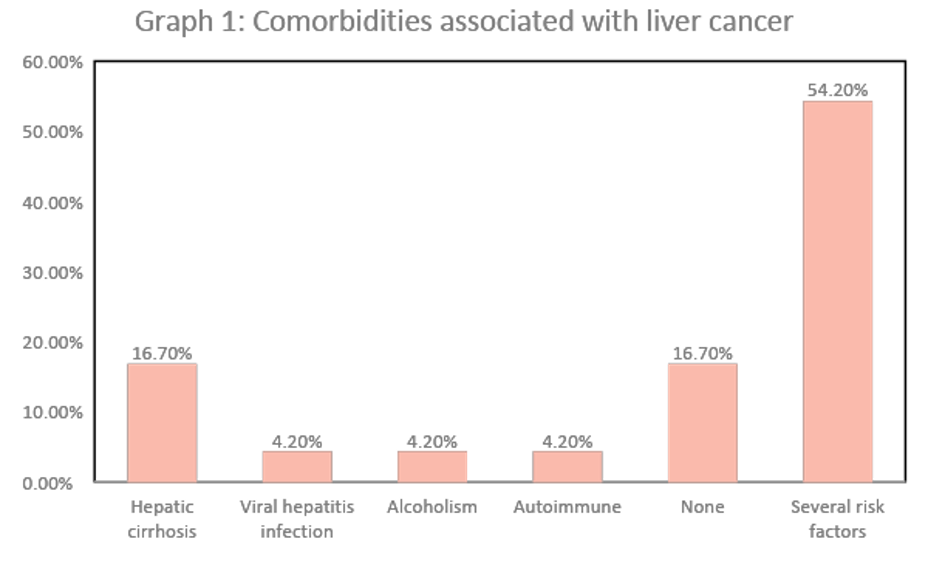
The presence of comorbidities in the sample population included hepatic cirrhosis, with a prevalence of
16.70%. However, the majority of patients had one or more comorbidities, resulting in a prevalence of
54.20%.
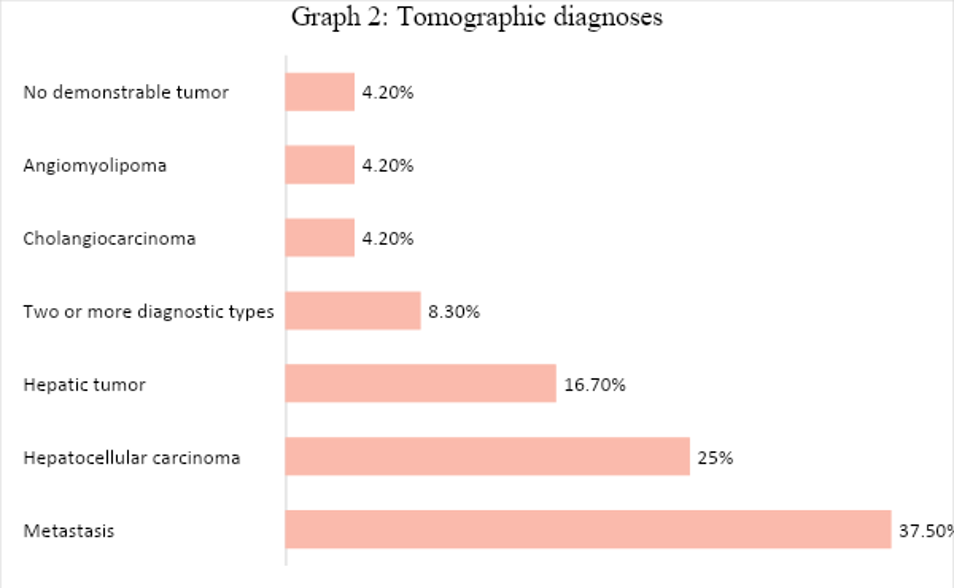
The most frequent tomographic diagnosis was metastasis, with n=9 (37.50%), followed by hepatocellular carcinoma with 6 (25%), and in third place, hepatic tumor with 4 (16.70%). The rest of the diagnoses are shown in Figure 2.
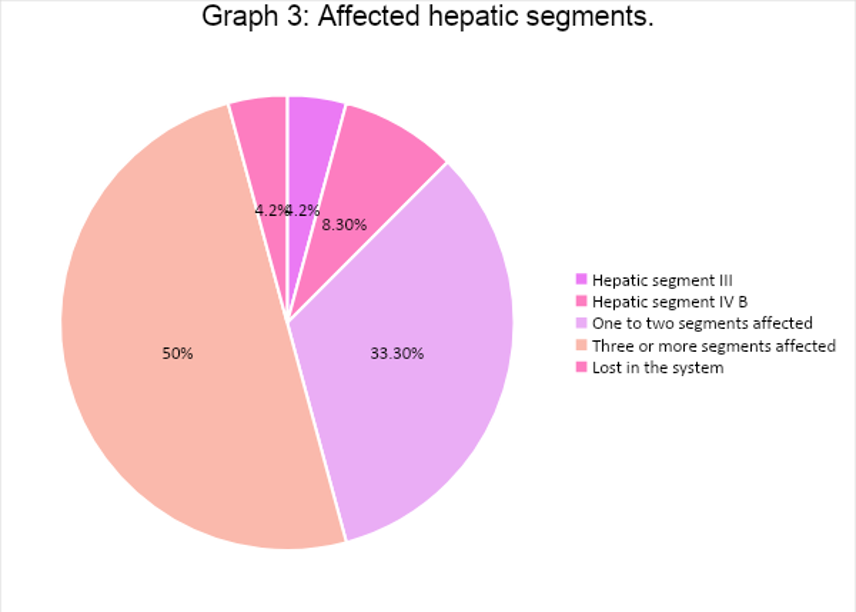
Regarding the hepatic segments, most patients had three or more liver segments affected by the tumor, 12 (50%). Only one patient had no affected segments because the presence of the tumor could not be demonstrated by CT scan, and the phase with the most enhancement due to the tumor was the arterial phase, 17 (70.80%) (See Figures 3 and 4).
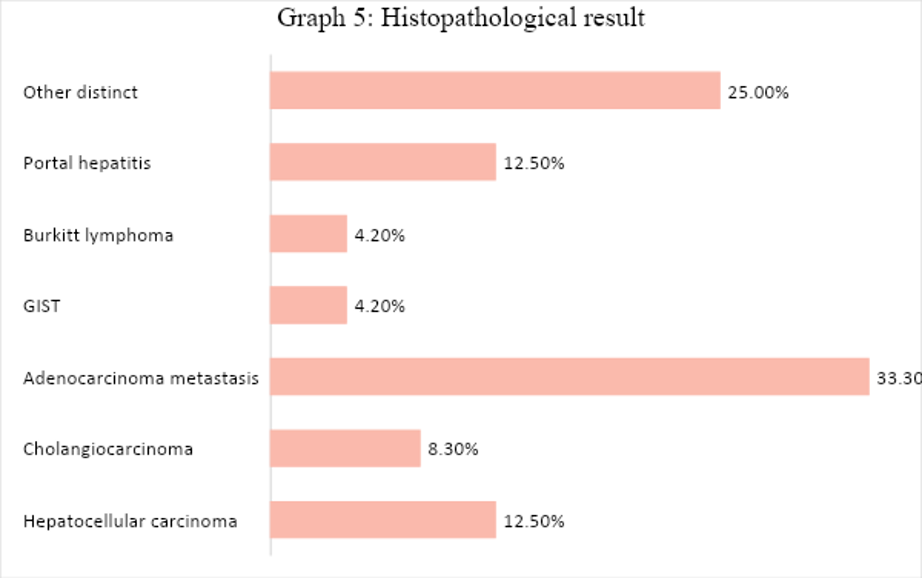
Out of the 24 patients with liver lesions, 15 (62.50%) tested positive for malignancy, while 9 (37.50%) had a negative result for malignancy. The primary histopathological diagnosis was adenocarcinoma metastasis, accounting for 8 (33.30%) cases. The remaining diagnoses are shown below.
The results of the correlation between the tomographic diagnosis and the definitive histopathological
diagnosis did not show statistical significance (p=0.10), and the correlation coefficient was 0.61,
indicating a weak correlation.
Discussion
Despite CT scanning being ideal for diagnosing liver cancer, it is necessary to distinguish the
characteristics of a primary tumor and a metastasis site regardless of the patient's clinical
presentation. Various studies have been conducted to distinguish between them, concluding that a primary
tumor is more frequently established in liver segment 8, while metastases are expressed in segment 5
(29, 30).
For lesions larger than 2 cm, CT is considered the gold standard for detecting malignant liver neoplasms
with diagnostic accuracy of almost 100%. However, its sensitivity decreases to approximately 60% when
the lesion is smaller (31).
A total of 24 patients with suspected malignant liver lesions were analyzed over a six-month period,
with a mean age of 57.54 years, mostly female. This is in line with international guidelines for liver
and biliary tract cancer, which show increased predisposition in women after 50 years of age, although
it differs from other descriptive studies where nearly 60% of the population are men (22, 32, 33).
On the other hand, the majority of the included population had a variety of comorbidities; however, when
analyzed in isolation, the presence of liver cirrhosis was the most predominant characteristic, with an
estimated 80% of patients worldwide with a history of or current hepatocellular carcinoma having this
antecedent (34).
Another comorbidity reported as a fundamental cause of liver cancer is prior infection with Hepatitis B
and C viruses, which for a long time was considered the main triggering factor for this neoplasm;
however, in this population, the percentages reached 4.20% of the total sample included (35, 36).
Regarding imaging studies, the primary imaging method used is ultrasound due to its low cost; however,
the sensitivity and specificity it offers are lower than other imaging techniques such as CT scan.
Nonetheless, due to its clear difficulty in lesions <1cm, it is suggested that a biopsy of the lesion
be performed to confirm the findings, as was done in this study (37).
Similarly, concerning the characteristics obtained by imaging, hepatocellular carcinoma can be
diagnosed, for example, if the main finding on the CT scan is enhancement in the hepatic arterial phase
combined with washout in the portal phase, confirming the presence of a neoplastic lesion. However, in
this study, only 12.5% of the population had this characteristic, while more than 60% did not show
enhancement, so it was necessary to perform a liver biopsy in all patients for confirmation (37).
Regarding liver segments, most patients had more than one segment affected by the lesion, this being due
to the average lesion size of 2.39 centimeters, while the maximum tumor size found in patients in this
study was 3 centimeters.
On the other hand, concerning histopathological study, the main types of neoplastic lesions diagnosed
are cholangiocarcinoma and hepatocellular carcinoma, with the latter being the most common of the two
(38).
When correlating the findings obtained by computed tomography and by histopathology in suspicious liver
lesions, it was found that the main diagnosis given by these two tools was hepatocellular carcinoma
(25%); on the other hand, regarding cholangiocarcinoma visualized by CT scan, it was only demonstrated
in 4.2% of the population, which differs considerably from the biopsy, which was demonstrated in 8.3%.
Placing the results in the contingency table for diagnostic test evaluation, computed tomography was
taken into consideration at the top of the table, and the anatomopathological study obtained by
ultrasound-guided biopsy, in which each column represented cases positive for malignancy obtained in
both studies, and each row represented the suspicion of malignancy.
Additionally, the diagnostic possibilities of both auxiliary techniques in the diagnosis of neoplastic
pathologies were not the same, and there was no significant difference between the diagnostic suspicion
provided by the imaging study, in this case, the CT scan, and the confirmation study, which is the
biopsy for subsequent pathological anatomy study.
Among the limitations of the study is that the sample size is smaller compared to previous studies;
however, this limitation did not prevent the study objectives from being met.
CONCLUSION
There was no significant correlation between histopathological study and tomographic findings in
suspected malignant liver lesions.
Authorship contributions:
The authors participated in the genesis of the idea, project design, data collection and
interpretation, results analysis, and manuscript preparation of the present research work.
Financing:
The authors received no assistance or funding for the present work.
Declaration of conflict of interest:
The authors declare no conflict of interest.
Recevied:
October 24, 2023
Approved:
April 8, 2024
Correspondence author:
Álvaro José Montiel-Jarquín.
Address:
Calle 2 norte # 2004. Colonia Centro. CP 72000. Puebla, Pue.
Phone:
+52 (222) 2424520 extensión 61315. Teléfono móvil: +521 2222384907
E-mail:
dralmoja@hotmail.com
Article published by the Journal of the faculty of Human Medicine of the Ricardo Palma University. It is an open access article, distributed under the terms of the Creatvie Commons license: Creative Commons Attribution 4.0 International, CC BY 4.0 (https://creativecommons.org/licenses/by/1.0/), that allows non-commercial use, distribution and reproduction in any medium, provided that the original work is duly cited. For commercial use, please contact revista.medicina@urp.edu.pe.
BIBLIOGRAPHIC REFERENCES