ORIGINAL ARTICLE
REVISTA DE LA FACULTAD DE MEDICINA HUMANA 2024 - Universidad Ricardo Palma10.25176/RFMH.v24i2.6068
CLINICAL AND EPIDEMIOLOGICAL CHARACTERISTICS OF ACUTE PANCREATITIS IN HIGH ALTITUDE RESIDENTS
CARACTERÍSTICAS CLÍNICAS Y EPIDEMIOLÓGICAS DE LA PANCREATITIS AGUDA DE LOS RESIDENTES DE ALTITUD
Geraldine Espinoza-Mayhua
 1,a
1,a
Amilcar Tinoco-Solórzano
 2,b
2,b
1 Faculty of Human Medicine, Universidad Peruana Los Andes, Huancayo, Peru
2 Department of Intensive and Intermediate Care, Hospital Nacional Ramiro Prialé Prialé, Social
Health Insurance of Peru (EsSalud), Huancayo, Peru.
a MD, Surgeon
b MD, Specialist in Human Medicine
ABSTRACT
Introduction: Acute pancreatitis (AP) may have particular characteristics at high altitude that
can affect its severity.
Objetive: To describe the clinical and epidemiological characteristics of AP in residents at high
altitude.
Methods: Observational and descriptive study conducted in a hospital at 3,250 meters above sea
level (masl) in Huancayo, Peru. A total of 129 patients with AP between 2017 and 2021 were included.
Clinical, demographic, and management characteristics were analyzed. Data were collected at admission
and followed until hospital discharge. Statistical analysis was performed using SPSS version 32,
describing qualitative variables with frequencies/percentages and quantitative variables with
mean/standard deviation or median/interquartile ranges according to the distribution.
Results: The mean age was 45.8 years; 61.2% were women. The mean BMI was 26.1 kg/m², and the
hospital stay was 11.1 days. The main cause of AP was biliary (78.3%). The mean SaO2 was 91.6%; PaO2,
68.7 mmHg; PaCO2, 29.4 mmHg; HCO3, 18.8 mEq/L; hemoglobin, 15.5 g; hematocrit, 46.3%; AST, 286.4 U/L;
and ALT, 313.9 U/L. The incidence of AP was 38.4 cases per 10,000 admissions. 13.2% were admitted to the
ICU, with a mortality rate of 52.9%. The most frequent complications were peri-pancreatic collections
(14.7%) and pancreatic necrosis (9.3%). The overall mortality was 13.9%.
Conclusion: AP at high altitude shows many similar characteristics to sea level; however,
differences in SaO2, PaO2, PaCO2, HCO3, and mortality may suggest an influence of hypobaric hypoxia that
should be corroborated in further studies.
Keywords: Pancreatitis; Epidemiology; Altitude; Retrospective Studies (source: MeSH NLM)
RESUMEN
Introducción: La pancreatitis aguda (PA) podría tener características particulares en altitud que
pueden afectar su severidad.
Objetivo: Describir características clínicas y epidemiológicas de la PA en residentes de altitud.
Métodos: Estudio observacional y descriptivo realizado en un hospital a 3 250 metros sobre el
nivel del mar (msnm) en Huancayo, Perú. Se incluyeron 129 pacientes con PA entre 2017 y 2021. Se
analizaron características clínicas, demográficas y de manejo. Los datos se recolectaron al ingreso y se
siguieron hasta el alta hospitalaria. El análisis estadístico se realizó usando SPSS versión 32,
describiendo variables cualitativas con frecuencias/porcentajes y cuantitativas con media/desviación
estándar o mediana/rangos intercuartílicos según la distribución.
Resultados: La edad media fue 45,8 años; el 61,2% fueron mujeres. El IMC medio fue de 26,1 kg/m²
y la estancia hospitalaria de 11,1 días. La causa principal de PA fue biliar (78,3%). La media de SaO2
fue 91,6%; de PaO2, 68,7 mmHg; de PaCO2, 29,4 mmHg; de HCO3, 18,8 mEq/L; de hemoglobina, 15,5g; de
hematocrito, 46,3%; de TGO, 286,4 U/L y de TGP, 313,9 U/L. La incidencia de PA fue 38,4 casos por cada
10000 ingresos. El 13,2% ingresó a UCI, con una mortalidad del 52,9%. Las complicaciones más frecuentes
fueron colecciones peri-pancreáticas (14,7%) y necrosis pancreática (9,3%). La mortalidad global fue
13,9%.
Conclusión: La PA en altitud muestra muchas características similares al nivel del mar; empero,
las diferencias en SaO2, PaO2, PaCO2, HCO3 y la mortalidad, podría sugerir una influencia de la hipoxia
hipobárica que deberá ser corroborada en otros estudios.
Palabras clave: Pancreatitis; Epidemiología; Altitud; Estudios Retrospectivos (fuente: DeCS-
BIREME)
INTRODUCTION
Acute pancreatitis (AP) is an inflammation of the pancreas that can become systemic. The diagnosis of AP
is established using at least two of the following criteria: upper abdominal pain radiating to the back,
amylase and/or lipase levels three times higher than normal, and typical findings on imaging (1). The mortality rate of AP varies between one and four percent, with the
main causes being biliary (64%) and alcoholic (9%) (1 - 4).
Over the last twenty years, the incidence of AP has increased by three percent annually, ranging from
0.3 per ten thousand inhabitants in Asia to 13.6 in North America. The average age of the patients is
40.14 years, and the disease affects more females. The most common clinical presentation is abdominal
pain, and the length of hospital stay varies between four and six days (4, 5).
The geographic environment can influence the presentation of AP. A population is considered at altitude
when it is above 1,500 meters above sea level (masl), and a permanent resident is someone who has lived
at altitude for at least one year (6). At altitudes below 3,000 masl, the
clinical and epidemiological characteristics of AP are similar to those observed in other parts of the
world (7). However, at altitudes above 3,000 masl, mortality is higher, and
AP presents unique challenges due to the overestimation of severity caused by the reduction in arterial
oxygen partial pressure (PaO2). This affects the classification of severity in various systems,
negatively impacting clinical management (8, 9). Moreover,
these studies have limitations in describing demographic, laboratory, imaging, and complications data,
and may differ from the sociocultural and epidemiological environment of this study, which could
influence the presentation and severity of AP (3, 10, 11).
Our study seeks to fill the knowledge gap identified by previous studies, addressing the limitations in
describing demographic, laboratory, imaging, and complications data. Furthermore, we aim to demonstrate
that physiological adaptations caused by life at altitude influence the characteristics of AP, affecting
both its presentation and severity in this particular environment (6). The
general objective of this study is to describe the clinical and epidemiological characteristics of AP in
residents at altitude. The specific objectives include determining the incidence, mortality, admission
to intensive care units (ICU), and local complications of AP. Our results will allow for improved
assessment in the initial diagnosis of AP at altitude.
METHODS
Design and study area
This is an epidemiological, observational, descriptive, longitudinal, and retrospective study. The
STROBE checklist for observational studies was used. The study was conducted at a level III-1 hospital
located at 3,250 masl, with a barometric pressure of 535 mmHg in Huancayo, Peru. Data were collected at
patient admission to the hospital and followed until hospital discharge to determine admission to the
operating room, ICU, and mortality.
Population and sample
The population consisted of 129 hospitalized patients from January 2017 to December 2021 at Hospital
Regional Daniel Alcides Carrión. No sampling was performed as the entire available population was used.
Adult patients who were permanent residents at altitude with AP were included. Patients with incomplete
medical records, those referred to other institutions, and those who requested voluntary discharge were
excluded.
Variables and instruments
The variables studied included clinical and demographic characteristics. Clinical characteristics
comprised vital functions, complete blood count, biochemical tests, arterial gases, abdominal
ultrasound, chest X-ray, and abdominal tomography. Demographic variables included age, sex, weight,
height, body mass index (BMI), residence at altitude, marital status, education level, occupation,
length of hospitalization, signs and symptoms, etiology, and type of management. These were collected
using a data collection form, and the technique was the documentation of medical records.
Procedures
Data were collected at patient admission to the hospital and followed until hospital discharge to record
events such as admission to the operating room, ICU, and mortality. Patients were clinically evaluated,
and corresponding laboratory and imaging tests were performed.
Statistical analysis
For statistical processing, SPSS software version 32 was used. In the univariate analysis, the normality
of the variables was verified using the Shapiro-Wilk test (p>0.05 normal; p<0.05 not normal).
Qualitative variables were described with frequencies and percentages, quantitative variables with
normal distribution with mean and standard deviation, and quantitative variables without normal
distribution with median and interquartile ranges.
Ethical considerations
This study obtained its data by reviewing the medical records of adult patients, so it was not necessary
to request informed consent. However, the confidentiality of the names of the participants was
maintained by recording these data in coded form. Permission was obtained from the hospital to access
the data. The study complies with current bioethical research standards and was approved by the Ethics
Committee of the Faculty of Human Medicine of the Universidad Peruana Los Andes, Huancayo, Peru.
RESULTS
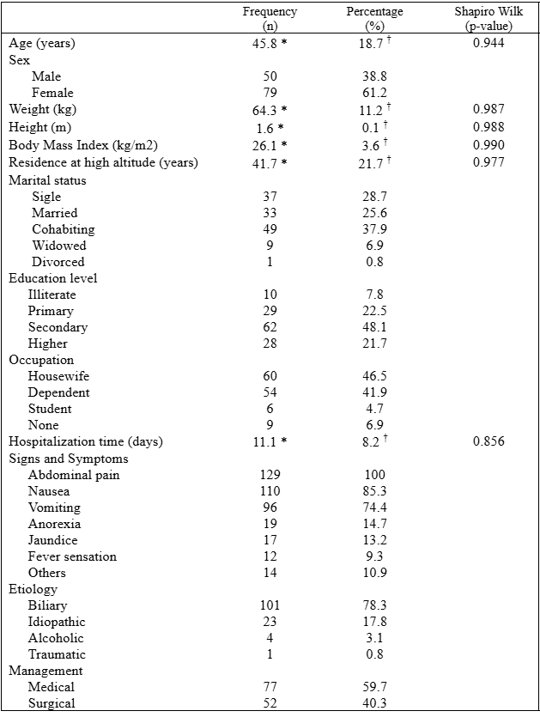
Data from 129 patients with acute pancreatitis (AP) were analyzed, who were admitted and followed until
their hospital discharge. The mean age was 45.8 years, with a predominance of female patients (61.2%).
The average BMI was 26.1 kg/m², and the mean hospital stay was 11.1 days. The most frequent symptoms
were abdominal pain, nausea, and vomiting. The main cause of AP was biliary, and medical management
predominated (Table 1).
Table 1: Epidemiological characteristics of acute pancreatitis in residents of high altitudes.
n = 129. * mean. † standard deviation
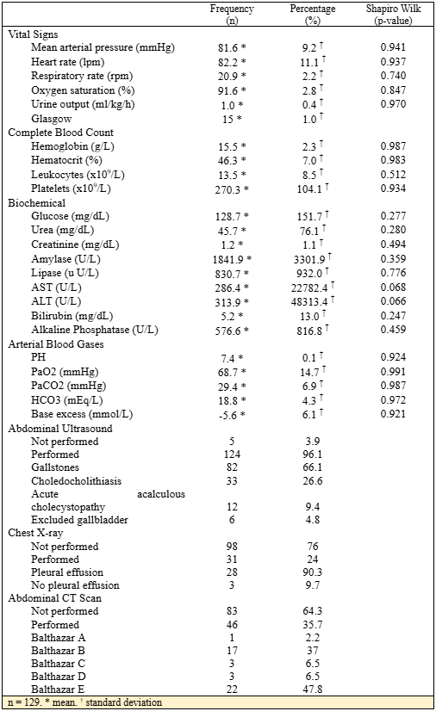
The values found for clinical parameters were: mean arterial pressure (MAP) of 81.6 mmHg, oxygen
saturation (SaO2) of 91.6%, PaO2 of 68.7 mmHg, PaCO2 of 29.4 mmHg, bicarbonate (HCO3) of 18.82 mEq/L,
hematocrit of 46.3%, aspartate aminotransferase (AST) of 286.4 U/L, and alanine aminotransferase (ALT)
of 313.9 U/L. Chest X-rays were performed on 31 patients (24%), finding pleural effusion in 90.3% of
them. Abdominal ultrasound was performed on 124 patients (96.1%), finding gallstones in 66.1%. Abdominal
CT scans were performed on 46 patients (35.7%), with 47.8% classified as Balthazar E (Table 2).
Table 2: Clinical characteristics of acute pancreatitis in residents of high altitudes
n = 129. * mean. † standard deviation
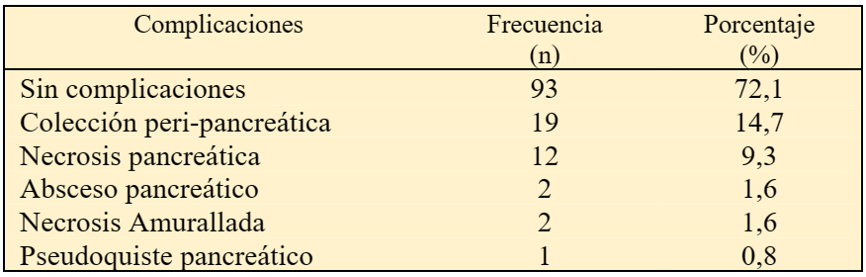
27.9% of patients presented local complications, with the most frequent being peripancreatic collections
(14.7%) and pancreatic necrosis (9.3%) (Table 3).
Table 3. Local complications of acute pancreatitis in residents of high altitudes
n = 129
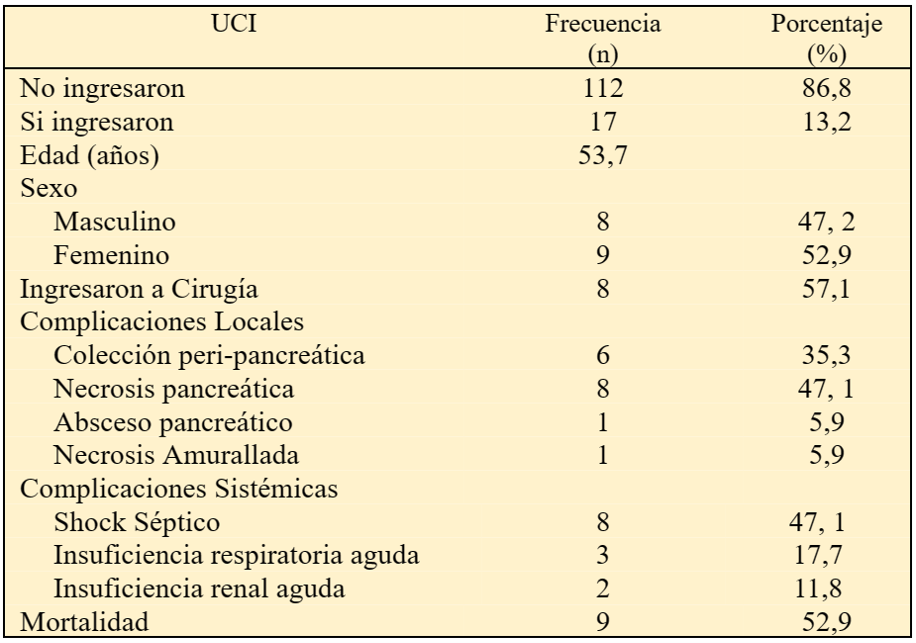
13.2% of patients with acute pancreatitis (AP) were admitted to the ICU. Of these, 47.1% presented
pancreatic necrosis, 57.1% were admitted after undergoing surgery, and 47.1% developed septic shock. The
mortality rate for patients with AP in the ICU at high altitude was 52.9% (Table 4).
Table 4. Characteristics of acute pancreatitis in residents of high altitudes who were admitted to the Intensive Care Unit (ICU)
n = 129. ICU: Intensive Care Unit
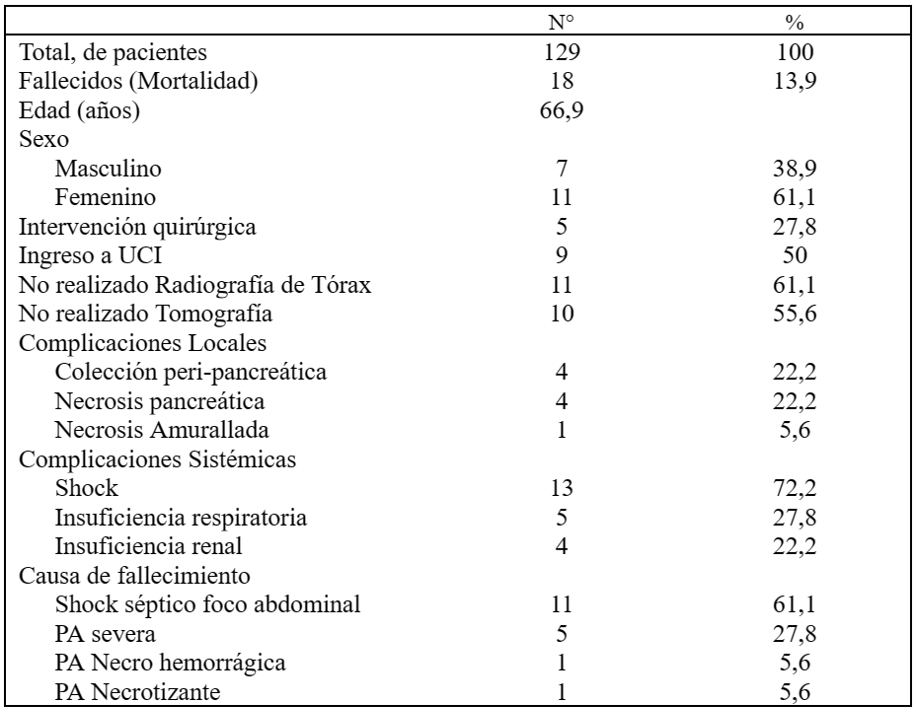
The overall mortality of the 129 patients with acute pancreatitis was 18 patients, representing 13.9%.
Of these, 50% had been admitted to the ICU and 27.8% had undergone surgery. The cause of death in 61.1%
of cases was septic shock. Abdominal CT scans had not been performed on 55.6% of these patients (Table
5).
Table 5. Characteristics of mortality from acute pancreatitis in residents of high altitudes
n = 129. ICU: Intensive Care Unit. AP: Acute Pancreatitis
DISCUSSION
Globalization has standardized dietary styles, physical activity, weight control, and toxic substance
use, leading the high-altitude population to adopt lifestyles similar to those of sea-level residents.
In the present study, the predominant age group was adults (36 to 64 years), with a mean age of 45.84
years. The majority of patients were women (61.2%), and 85% were overweight with a BMI over 25 kg/m².
The average hospital stay was 11.14 days. The most common symptoms were abdominal pain, nausea, and
vomiting, with a predominantly biliary etiology, and medical treatment was as frequent as observed at
sea level (12, 13).
A mean arterial pressure (MAP) of 81.6 mmHg was reported, comparable to patients with AP at sea level.
However, it is important to note that healthy residents at altitude have a higher MAP, between 79 and 83
mmHg (14 - 16), likely due to hypobaric hypoxia,
suggesting that this elevation is not a consequence of AP but of altitude conditions.
At sea level, AP patients exhibit elevated hemoglobin and hematocrit levels (17). A hematocrit over 44% increases the risk of developing severe acute
pancreatitis and is an independent predictor of mortality. We observed a hematocrit of 46.31%, similar
to values reported by Landeo et al. (18). However, this elevation is common
in healthy altitude residents due to the decrease in partial oxygen pressure, which causes tissue
hypoxia and an increase in erythropoietin production, raising the red blood cell count (15, 19). Thus, the hematocrit elevation may be more
related to altitude than to AP. It remains to be determined whether these values in healthy altitude
residents increase the risk of developing severe pancreatitis (3).
The behavior of transaminases in healthy altitude residents is similar to that of sea-level residents,
as no alteration in liver cell integrity is observed (20). In patients with
AP at sea level, elevated levels of AST and ALT are reported (11, 21). In the present study, elevated levels of AST (286.4 U/L) and ALT
(313.9 U/L) were reported, similar to previous studies conducted at altitude (18).
Abdominal ultrasound was performed in 96.1% of our sample, finding gallstones in 66.1%, results similar
to those reported at sea level (21). CT scans performed at 72 hours from
the onset of symptoms are used to determine the severity of AP in patients with unfavorable progression.
In the studied population, it was performed in 35.7% of cases, with 47.8% classified as Balthazar E and
37% as Balthazar B, results similar to those observed at sea level (2, 18). However, these results should be analyzed with caution, as CT scans
were not performed on the entire sample.
The most frequent complications in patients with AP at altitude were acute peri-pancreatic fluid
collections and pancreatic necrosis, which usually resolve spontaneously, results similar to those
previously reported (22, 23). 13.2% of patients with AP
were admitted to the ICU, a proportion similar to that recorded at sea level (12). 57.1% were admitted after undergoing surgery for pancreatic necrosis,
with septic shock being the most frequent reason for admission. The mortality rate in these patients
reached 52.9%. Surgical intervention in sterile necrosis is associated with an increase in mortality,
whereas infected necrosis should be surgically treated as soon as possible, according to the clinical
situation, even before antibiotic therapy (23). Cholecystectomy is
recommended to be performed six weeks after the acute episode (24).
Surgical treatment of sterile AP is associated with mortality (12, 13), so evolutionary control through radio-guided abdominal puncture is
necessary upon any suspicion of deterioration (25).
Thus, altitude seems not to influence characteristics of AP such as age, sex, BMI, hospital stay,
clinical presentation, etiology, MAP, hemoglobin, hematocrit, transaminases, ICU admission,
complications, abdominal ultrasound results, and type of management, being similar to those reported at
sea level. However, patients with AP at altitude exhibit lower values of SaO2, PaO2, PaCO2, and HCO3,
and a higher incidence and mortality than those reported at sea level.
There are evolutionary differences between patients with AP at sea level and those at altitude. However,
when comparing patients with AP to the healthy altitude population, no significant differences are
observed, which could be explained by the response to chronic hypobaric hypoxia. We reported an SaO2 of
91.6% compared to 96% at sea level in patients with AP (14). Healthy
residents at altitude have an SaO2 between 88% and 97% (15), directly
related to the altitude level (16). Regarding arterial blood gases, the
results of this study at altitude show lower values of PaO2, PaCO2, and HCO3 compared to parameters at
sea level (26, 27). However, studies in healthy residents
at altitude also report decreased values of these parameters, with pH and lactate within normal values
(15, 28). Presenting low levels of PaO2, PaCO2, and HCO3
in altitude residents should be considered normal; therefore, in this population, it is better to assess
the decrease in pH, the increase in lactate, or the elevation of CRP, which could better predict an
evolution to organ dysfunction.
Pleural effusion is an alarming sign indicating an unfavorable progression and allows for the diagnosis
of potentially severe AP (22, 29). Its early detection is
essential via chest X-ray. It was found that 90.3% of the patients presented pleural effusion, a
percentage that doubles other studies (30). However, only 24% of the sample
in this study underwent chest X-ray, so these results must be validated with subsequent studies.
The global incidence of AP varies from 0.3 to 13.9 per 10,000 inhabitants (31). The results of this study show a higher incidence, with 38.44 cases
per 10,000 hospital admissions. The global mortality of AP is three to six percent. We observed a
mortality rate of 13.9%, much higher than the values at sea level (25). The
higher mortality could be explained by hypobaric hypoxia, which increases the hematocrit (8), although factors related to the surgical management of pancreatic
necrosis and evolution to septic shock may also influence. These hypotheses need to be tested. This
study aims to be the first step in a new line of research on "Acute Pancreatitis at Altitude," which
will continue with subsequent studies.
Among the limitations of our study, we must assume those related to a descriptive study, in which, not
having a sea-level control group, we can only propose hypotheses. Another significant bias was the lack
of uniformity in imaging studies, which were not performed on the entire sample, potentially leading to
information bias. However, despite these limitations, it is one of the few studies analyzing AP at
altitude, specifically in a unique environment like the Peruvian highlands, providing valuable data.
CONCLUSION
The study on AP at altitude showed a mean age of 45.8 years, predominantly women (61.2%), with an
average BMI of 26.1 kg/m². The average hospital stay was 11.1 days, with common symptoms of abdominal
pain, nausea, and vomiting. The main cause was biliary, predominating medical management. The incidence
of AP was 38.44 cases per 10,000 hospital admissions, and the mortality rate was 13.9%. 13.2% of
patients were admitted to the ICU, with a mortality rate of 52.9%. The most frequent complications were
peri-pancreatic collections and pancreatic necrosis. Although, when comparing these results with other
studies, altitude does not appear to influence certain clinical and demographic characteristics of AP,
lower values of SaO2, PaO2, PaCO2, and HCO3 were observed compared to those reported at sea level,
suggesting an impact of hypobaric hypoxia on AP at altitude. We recommend conducting analytical studies
comparing altitude populations with sea-level populations to verify if altitude has a direct
relationship with the increase in incidence and mortality of AP.
Authorship contributions:
GEM and ATS participated in the conceptualization, data curation, formal analysis, research,
visualization, and writing and review of the original draft. In addition, they approved the
final version for publication.
Financing:
This article was funded by the authors
Declaration of conflict of interest:
The authors declare no conflicts of interest.
Recevied:
November 25, 2023
Approved:
April 29, 2024
Correspondence author:
Amilcar Tinoco-Solórzano
Address:
Independencia 266, Huancayo 12006, Perú
Phone:
064 481120
E-mail:
amilcartinoco@gmail.com
Article published by the Journal of the faculty of Human Medicine of the Ricardo Palma University. It is an open access article, distributed under the terms of the Creatvie Commons license: Creative Commons Attribution 4.0 International, CC BY 4.0 (https://creativecommons.org/licenses/by/4.0/), that allows non-commercial use, distribution and reproduction in any medium, provided that the original work is duly cited. For commercial use, please contact revista.medicina@urp.edu.pe.
BIBLIOGRAPHIC REFERENCES