CLINICAL CASE
REVISTA DE LA FACULTAD DE MEDICINA HUMANA 2024 - Universidad Ricardo Palma10.25176/RFMH.v24i1.6076
SUCCESSFUL INTRABDOMINAL PRETERM PREGNANCY: A CASE REPORT
EMBARAZO PRETÉRMINO INTRABDOMINAL EXITOSO: REPORTE DE CASO
Saida Anyul Abud-Flores
 1,a
1,a
Marco Andrés González Martínez
 1,b
1,b
Carlos Alberto López-Bernal
 1,c
1,c
Arturo García-Galicia
 1,d
1,d
Álvaro José Montiel-Jarquín
 1,e
1,e
Gisela Alonso Torres
 1,b
1,b
Nancy Rosalía Bertado Ramírez
 1,f
1,f
Laura Andrea Reyes-Luna
 1,a
1,a
1 Unidad Médica de Alta Especialidad Hospital de Especialidades de Puebla, Centro Médico Nacional
“Gral. de Div. Manuel Ávila Camacho”, Instituto Mexicano del Seguro Social, Puebla de Zaragoza, México.
a Medical resident in General Surgery
b Medical intern in Social Service
c Medical specialist in General Surgery, subspecialist in Colon and Rectal Surgery
d Medical specialist in Pediatrics. Master of Medical Sciences and Research
e Medical specialist in General Surgery. Master of Medical Sciences and Research
f Medical specialist in Neurology
ABSTRACT
Introduction: Ectopic pregnancy is any gestation in which the implantation site of the fertilized
egg is located outside the endometrial cavity. Abdominal ectopic pregnancy represents 1.4% of these.
Case report: 28-year-old patient with two previous cesarean sections; bilateral tubal obstruction
during the last operation. The patient was admitted to the hospital with blood pressure of 180/130 mm Hg
that did not respond to medical treatment and not progression to labor so it was decided to interrupt
the pregnancy by cesarean section. During surgery, a small uterus with extrauterine pregnancy was
observed adhered to the serosa of the cecum, ascending colon, and appendix. A live preterm female
product was obtained; the mother had a favorable evolution and no postoperative complications.
Conclusion: Ectopic pregnancies are rera. An adequate prenatal control by well trained personnel
is essential for an accurate diagnosis. The mother and the newborn did not present any complication. It
is very important to have and accurate an opportune diagnosis so trained personnel can offer an adequate
management.
Keywords: Ectopic pregnancy, abdominal pregnancy, caesarean section, placenta (Source: MeSH).
RESUMEN
Introducción: El embarazo ectópico es toda gestación, en la que el sitio de implantación del
óvulo fecundado se localiza fuera de la cavidad endometria y representa el 1.4 % de estos.
Caso clínico: Paciente de 28 años con dos cesáreas previas, sometida a salpingoclasia durante la
última intervención. La paciente ingresó al hospital con presión arterial de 180/130 mm Hg, no respondió
a tratamiento médico y presentó falla en la progresión de trabajo de parto, por lo que se decidió
interrupción por operación cesárea. Durante la cirugía, se observó un pequeño útero con embarazo
extrauterino adherido a la serosa del ciego, el colon ascendente y el apéndice. Se obtuvo un producto
femenino pretérmino vivo; la madre cursó con evolución favorable y sin complicaciones posoperatorias.
Conclusión: La presentación del embarazo abdominal ectópico es rara, por lo que un control
prenatal adecuado por personal capacitado puede orientar a la sospecha diagnóstica. La madre y la recién
nacida no presentaron ninguna complicación, a pesar de ser un embarazo abdominal avanzado y la inserción
multifocal de la placenta. Se resalta la importancia del manejo oportuno y multidisciplinario cuando se
enfrentan embarazos con curso anormal para la mejor evolución de la madre y del producto.
Palabras clave: Embarazo ectópico, embarazo abdominal, cesárea, placenta (Fuente:
DeCS).
INTRODUCTION
Ectopic pregnancy is defined as any pregnancy in which the implantation site of the fertilized ovum is
located outside the endometrial cavity. This type of pregnancy represents 1.5% to 2% of all pregnancies
(1).
The most common implantation site for ectopic pregnancies is the fallopian tube (2). Approximately 10%
implant in non-tubal locations such as the cervix, ovary, interstitial portion of the fallopian tube,
broad ligament, uterine horn, cesarean scar, and abdominal cavity (3). The
latter represents only 1.4%
of ectopic pregnancies, with an incidence of 1 in 10,000 births (4). The
most significant risk factors
for ectopic pregnancy include previous tubal pregnancy, prior tubal surgery and ligation, unintended
pregnancy as a complication, tubal pathology, and intrauterine device (IUD) use (5).
Abdominal pregnancy occurs when the fertilized ovum implants in the peritoneal cavity. Common
implantation sites include the uterine serosa, diaphragm, pelvic vessels, liver, spleen, intestine,
omentum, pelvic wall, and broad ligament (4). A history of assisted
fertilization is noteworthy (6).
Clinical presentation ranges from asymptomatic to acute abdominal pain depending on the corresponding
gestational age. Diagnosis is intraoperative in 50% to 90% of cases (7).
Ultrasound is the diagnostic
test of choice, with a specificity of 94% and sensitivity of 87% (8).
Maternal mortality is primarily
caused by uncontrollable hemorrhage, with a high rate of up to 5 per 1000 cases (7).
The diagnostic challenges and therapeutic approach in these patients are illustrated in the following
case.
Case Presentation
A 28-year-old patient at 37 weeks of pregnancy presented for a third-trimester ultrasound with
inadequate prenatal care and a history of two previous cesarean deliveries, followed by tubal ligation.
She was admitted to a rural hospital with a diagnosis of moderate hypertensive disorder of pregnancy,
with a blood pressure of 180/130 mmHg and a hemoglobin level of 11.8 mg/dl. Pharmacological management
for hypertension was initiated but failed to achieve adequate control, and there was no progression in
labor, leading to a decision for abdominal delivery. During the surgical intervention, a small uterus
with an amniotic sac in the peritoneal cavity was found. The abdominal cavity was closed, and the
patient was referred with a diagnosis of abdominal ectopic pregnancy to a secondary-level hospital as
the initial hospital lacked the necessary infrastructure.
At the secondary-level hospital, amniorrhexis was performed as a second intervention, resulting in the
delivery of a live female neonate without facial or limb anomalies, estimated at 34.4 weeks of gestation
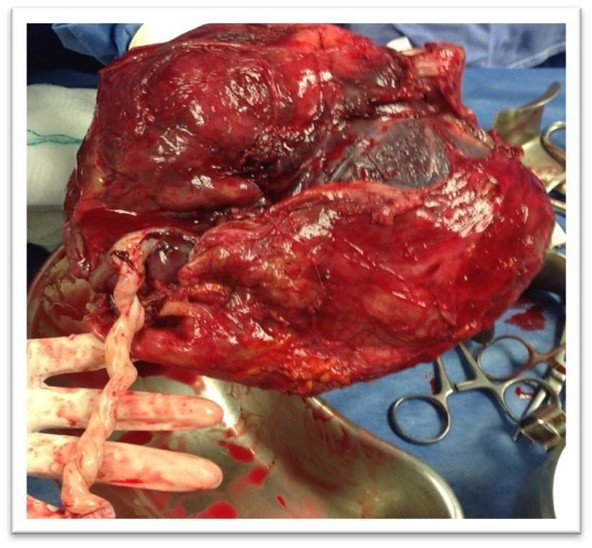
by Capurro scale (Figure 1). Subsequently, meticulous dissection of the placenta was performed, which
was adhered to the omentum, appendix, cecum, and ascending colon serosa (Figure 2). The decision to
remove the placenta was made to prevent potential complications, since it was loosely adhered to the
serosa and, being very close to the ileocecal valve, it could cause obstruction during its involution
and reabsorption; therefore, it did not require leaving it in situ. The maternal side of the placenta
was found without cotyledon formation (Figure 3). Fetal surface of the placenta without malformations
(Figure 4). The mother did not present intestinal perforation or additional complications.
She was transferred to the Intensive Care Unit (ICU) for monitoring and was discharged from the hospital
48 hours post-surgery with her baby without complications. Follow-up visits at 15- and 30-days
post-surgery reported normal progress.
Discussion
Abdominal pregnancy is a rare condition associated with high maternal mortality. Diagnosis is often
delayed due to inadequate prenatal care, as seen in this case. Abdominal pregnancies can remain
undetected until late gestational ages, depending on the site of implantation and involved organic
structures (9).
During gestation, the patient did not exhibit symptoms suggestive of abdominal ectopic pregnancy. The
reason for hospital admission was uncontrolled hypertensive disorder of pregnancy. In cases like this,
nonspecific or asymptomatic clinical presentation poses a challenge for timely diagnosis (6).
In this reported case, the patient underwent surgical intervention in two stages: initially, the
decision was made to discontinue the procedure due to the complexity of the case and was referred to a
hospital with better infrastructure.
The neonate in this case did not experience structural complications. The incidence of malformations in
live births from abdominal pregnancies is 23% (9), and up to 43.84% result
in stillbirths or early
neonatal deaths (10).
The implantation at multiple sites (omentum, cecum, ascending colon, and cecal appendix) in this case
was also an uncommon presentation, as only 5.79% of ectopic abdominal pregnancies involve three or more
placental implantation sites (10).
In this case, meticulous placental resection was achieved with complete surgical removal despite its
multifocal presentation, and no complications were observed during follow-up. Placental manipulation
often poses challenges due to difficulty in isolating blood supply. Frequently, leaving the placenta in
situ with administration of methotrexate or a second surgical intervention for removal is preferred.
Complications can include uncontrollable bleeding, disseminated intravascular coagulation, intestinal
obstruction, and gastrointestinal or genitourinary fistulas (11, 12). Regardless, careful monitoring must
be maintained.
The placenta may be removable without causing massive bleeding, as in cases of adherence to the omentum.
The preferred management is leaving the placenta in the cavity. Accumulation of necrotic tissue in
larger quantities would favor intra-abdominal infection.
Currently, the use of methotrexate is not recommended as it rapidly degrades placental tissue, leading
to abundant necrotic tissue and increased infection risk. The surgical decision regarding placental
management is highly controversial; some authors recommend placental extraction, associated with a lower
complication rate but also a higher maternal mortality rate. The decision to extract it or not depends
on the site of implantation (14).
Also noteworthy is the favorable outcome of the neonate, without complications typical of premature
infants, possibly due to the action of gestational hypertensive disorder. Cases that progress beyond 20
weeks, as in this case, are very rare. Both the mother and the newborn did not experience any
complications typical of advanced abdominal pregnancy and multifocal placental insertion.
Conclusion
The case presentation of ectopic abdominal pregnancy is rare, underscoring the importance of adequate
prenatal care provided by trained personnel to guide diagnostic suspicion. Despite being an advanced
abdominal pregnancy with multifocal placental insertion, neither the mother nor the newborn experienced
complications. This case highlights the significance of timely and multidisciplinary management when
faced with pregnancies deviating from the norm, ensuring optimal outcomes for both mother and child.
Authorship contributions:
All authors participated in the conceptualization, research, methodology, and writing of the
manuscript.
Financing:
The authors did not receive any assistance or funding for the present work.
Declaration of conflict of interest:
The authors declare no conflicts of interest.
Recevied:
December 1, 2023
Approved:
March 31, 2023
Correspondence author:
Arturo García-Galicia
Address:
Calle 2 norte # 2004. Colonia Centro. CP 72000. Puebla, Pue.
Phone:
+52 (222) 2424520 extensión 61314. Teléfono móvil: +521 (222) 1945360
E-mail:
neurogarciagalicia@yahoo.com
Article published by the Journal of the faculty of Human Medicine of the Ricardo Palma University. It is an open access article, distributed under the terms of the Creatvie Commons license: Creative Commons Attribution 4.0 International, CC BY 4.0 (https://creativecommons.org/licenses/by/1.0/), that allows non-commercial use, distribution and reproduction in any medium, provided that the original work is duly cited. For commercial use, please contact revista.medicina@urp.edu.pe.