ORIGINAL ARTICLE
REVISTA DE LA FACULTAD DE MEDICINA HUMANA 2024 - Universidad Ricardo Palma10.25176/RFMH.v24i1.6086
SHORT AND PROLONGED FASTING PRIOR TO THE PERFORMANCE OF TRACHEOSTOMIES IN INTENSIVE THERAPY: A RETROSPECTIVE STUDY
AYUNO CORTO VS PROLONGADO PREVIO A LA REALIZACIÓN DE TRAQUEOSTOMÍAS EN PACIENTES DE TERAPIA INTENSIVA: UN ESTUDIO RETROSPECTIVO
DURAN, Lucas Gonzalo
 1,2
BEILMAN María Emilia
1,2
BEILMAN María Emilia
 1,2
QUIROGA, Araceli Natali
1,2
QUIROGA, Araceli Natali
 3
3
CRUZ Magdalena
 2
MILLAN Alejandra Vanesa
2
MILLAN Alejandra Vanesa
 2
OJEDA Micaela Johanna
2
OJEDA Micaela Johanna
 2
2
CICCIOLI Fabiana
 2
MONTENEGRO FERNANDEZ Micaela Giselle
2
MONTENEGRO FERNANDEZ Micaela Giselle
 2
2
MONRROY MIRO Wendy Estefany
 2
MALISIA Valentina Trinidad
2
MALISIA Valentina Trinidad
 2
GRASSI Nicolas Antonio
2
GRASSI Nicolas Antonio
 2
2
ZELAYA DE LEON, Nazareno Iñaki
 2
ESPINOZA Franco Ezequiel
2
ESPINOZA Franco Ezequiel
 2
OTAMENDI Marina
2
OTAMENDI Marina
 2
2
ZORZANO OSINALDE, Paula
 2
PETASNY, Marcos
2
PETASNY, Marcos
 2
2
1 DEPARTAMENTO DE CIENCIAS DE LA SALUD, UNIVERSIDAD NACIONAL DEL SUR, BAHIA BLANCA, BUENOS AIRES,
ARGENTINA.
2 SERVICIO DE TERAPIA INTENSIVA, HOSPITAL MUNICIPAL DE AGUDOS DR. LEONIDAS LUCERO, BAHIA BLANCA,
BUENOS AIRES, ARGENTINA
3 SERVICIO DE CIRUGIA, HOSPITAL MUNICIPAL DE AGUDOS DR. LEONIDAS LUCERO, BAHIA BLANCA, BUENOS
AIRES, ARGENTINA
ABSTRACT
Introduction: International guidelines on aid prior to invasive procedures usually generate
longer aid than in intensive care (IT) patients. This fact represents a high risk of malnutrition and,
consequently, a worse prognosis. The objective of the present investigation was to analyze the degree of
association between the fasting time prior to tracheostomy of patients under mechanical ventilatory
assistance (MVA) and the appearance of pneumonia.
Methods: Retrospective cohort study that included patients admitted to our IT from 10/01/2018 to
08/31/2022 and with a tracheostomy performed. Two cohorts were defined characterized by fasting ≤3 hours
vs. >3 hours. Fisher's exact test and Mann-Whitney test were used for bivariate analysis. A p value
<0.05 was shown to be significant.
Results: 141 patients were hospitalized with a tracheostomy, 9 were excluded, leaving 132
patients. The cohort with fasting ≤3 hours was made up of 15 patients and the one with fasting >3 hours
was made up of 117, the latter presented an average fast of 2.5 hours (IR 2-3), days of AVM prior to the
procedure of 13 days (IR 12-18), while the other cohort presented an average fast of 6 hours (IR 5-8),
days of AVM prior to the procedure of 12 days (IR 10-14.5). When analyzing the association between the
type of fasting and the appearance of pneumonia, an OR of 0.958 (95% CI: 0.32-2.87) was obtained, p
value of 0.743.
Conclusions: No significant differences were found regarding fasting time and the appearance of
pneumonia as referred to in the international literature.
Keywords: Fasting, Tracheostomy, Pneumonia. (source: MeSH-NLM)
RESUMEN
Introducción: Las pautas internacionales sobre la práctica del ayuno previo a procedimientos
invasivos generalmente ocasionan ayunos más prolongados que en los casos de pacientes internados en las
Unidades de Cuidados Intensivos (UCI). Este hecho representa un alto riesgo de desnutrición y,
consecuentemente, un pronóstico más negativo. El objetivo de la presente investigación fue analizar el
grado de asociación entre el tiempo de ayuno previo a la traqueostomía de pacientes bajo asistencia
ventilatoria mecánica (AVM) y la aparición subsecuente de neumonía.
Métodos: Fue un estudio de cohorte retrospectivo que incluyó a pacientes ingresados en nuestra
UCI desde el 01/10/2018 hasta el 31/08/2022, quienes habían sido sometidos a una traqueostomía. Se
definieron dos cohortes caracterizadas por ayuno inferior o igual a tres horas y superior a tres horas.
Se utilizó la prueba exacta de Fisher y la prueba U de Mann-Whitney para el análisis bivariado. Un valor
de p < 0.05 se consideró significativo.
Resultados: Se hospitalizaron 141 pacientes con traqueostomía, 9 fueron excluidos, quedando 132
pacientes. La cohorte con ayuno ≤ 3 horas estuvo compuesta por 15 pacientes y la de ayuno > 3 horas
estuvo compuesta por 117; esta última presentó un ayuno promedio de 2.5 horas (RIC 2-3) y 13 días de AVM
previos al procedimiento (RIC 12-18), mientras que la otra cohorte presentó un ayuno promedio de 6 horas
(RIC 5-8) y 12 días de AVM previos al procedimiento (RIC 10-14.5). Al analizar la asociación entre el
tipo de ayuno y la aparición de neumonía, se obtuvo un OR de 0.958 (IC del 95%: 0.32-2.87) y valor de p
de 0.743.
Conclusiones: No se encontraron diferencias significativas respecto al tiempo de ayuno y la
aparición de neumonía, tal como se refleja en la literatura internacional.
Palabras clave: Ayuno, Traqueostomía, Neumonía. (fuente: DeCS-BIREME)
INTRODUCTION
Tracheostomy is one of the most frequently performed procedures in the intensive care unit (ICU).
According to medical literature, it is performed in 9-10 % of all mechanically ventilated patients in
the United States and the United Kingdom, respectively (1, 2, 3, 4). However, other studies that evaluated its
international prevalence have reported higher values, arguing that 24 % of these patients were assisted
through a tracheostomy (5).
Generally, these patients, who are being evaluated to undergo a tracheostomy, are usually in an
extremely critical condition with multiple associated comorbidities. This is aggravated when the
procedures are delayed due to the lack of fasting time of more than eight hours, indicated by the
anaesthesiologists or surgeons, that causes patients to remain fasting for more than a day in many
cases, with a high metabolic demand and, therefore, a greater risk of malnutrition, a condition that
increases the risk of septic complications and insulin resistance syndrome (6, 7). This fact produces a
delay in transfers to less complex floors and prolongs stays in the ICU, which is associated to an
increase in care costs.
Contrary to what may be assumed, pulmonary aspiration during anesthesia is a very rare event with low
incidence (8, 9). Bronchoaspiration is an unusual adverse
circumstance, with an incidence of 2.9 to 4.7
cases per 10 000 general anesthesia in the overall population (10). Due to
the physiological changes
that occur during pregnancy, obstetric patients have a two to three times higher risk (11).
Bronchoaspiration can be classified into two categories: aspiration pneumonia, which refers to
undetected aspiration of gastrointestinal contents that triggers pneumonia, and aspiration pneumonitis,
which refers to aspiration of gastric contents, that is directly observed by the doctor during
anesthetic induction, the surgical procedure or immediately after it (12).
When aspiration occurs, it is
most likely related to a complication during induction of anesthesia, laryngoscopy, or extubation
(13).
For this reason, it is possible to consider shorter preoperative fasting times for patients, who are
already endotracheally intubated and have easy access to the stomach through nasogastric or orogastric
tubes. The aim of the present investigation is to analyze the degree of association between the fasting
time prior to tracheostomy of patients under mechanical ventilatory assistance (MVA) and the subsequent
appearance of pneumonia, mortality from all causes, length of hospital stays, duration of intensive care
stays and the decline of the PAFI.
METHODS
A retrospective cohort study was performed. The target population was made up of all patients
hospitalized in a period between October 1, 2018 and August 31, 2022 in ICU of the Hospital Municipal de
Agudos Dr. Leónidas Lucero (HMALL) de Bahía Blanca.
Unit of analysis or eligible population
- Inclusion criteria: Only patients, who during their hospitalization, had a tracheostomy performed with any technique during the period in the study were included.
- Exclusion criteria: Patients who required the emergency procedure were excluded.
- Elimination criteria: Patients who, due to insufficient data recorded in the electronic medical record, were unable to obtain at least 80 % of the required data were eliminated.
Data collection instrument
Data were collected through the HMALL computer system that provides access to the digital medical
history of each patient. Likewise, laboratory data were obtained through the use of the NextLab®
computer system with which the hospital has an agreement.
Operational definition of the variables
- Reason for hospitalization: in ICU and was confirmed in the epicrisis upon discharge. It was classified into: cardiological, neurological, respiratory, infectious and other clinical emergency, planned post-operative, non-neurological surgical emergency and post-surgical complications.
- Type of fast: fasts were classified as short if they were less or equal than three hours and prolonged when they exceeded that period.
- Associated pneumonia: defined by suggestive symptoms (fever, purulent mucus, crackles), decrease in PaFi <200, and chest x-ray with clear infiltrate. To capture all intervention-related pneumonias, the criteria were expanded to include any new consolidation within a 5-day period after the intervention.
- PAFI: estimated by the ratio between the arterial oxygen pressure and the inspired fraction of oxygen. They were classified as pafi with severe decrease at values <100, moderate between 100 and 200 and mild between 200 and 300.
- MVA time: established in days until weaning from the ventilator or death.
- Hospitalization time in ICU: established as the duration in days of the patients' hospitalization in the ICU.
- Hospital stay time: established as the duration in days of the patients' stay in the hospital.
- Reason for orotracheal intubation: This variable is defined as the reason why it was decided to protect the airway. This may be due to respiratory failure, ventilatory failure or cardiorespiratory arrest.
- Type of tracheostomy: tracheostomy was classified if it was performed before 10 days and late if it was performed after that period.
- Tracheostomy technique: they can be defined as open or percutaneous.
- Surgical team: It could be composed of a resident – resident team; staff – resident; staff – staff.
- Type of surgical wound: classified as clean wound, clean contaminated wound, contaminated wound and dirty wound.
- Duration of the procedure: quantified in minutes from the beginning of the patient's induction until the fixation of the tracheostomy tube with suture.
Statistic analysis
Patients were coded numerically consecutively in consistent order with their medical record number,
which guaranteed the anonymity and confidentiality of the information at the time of analysis. A
univariate analysis was performed to estimate the percentages and means of each variable. To compare the
means of the baseline characteristics, the Student T test was used, after verifying the assumptions for
the delta PaFi variables, the rest of the numerical variables that did not have a normal distribution
were analyzed with the Mann-Whitney U test. To estimate the degree of association between fasting time
and pneumonia, a bivariate analysis was performed with cross-classification tables using Fisher's exact
test and subsequently a logistic regression model was performed to analyze the factors associated with
the presence of post-fasting pneumonia tracheostomy. A p value <0.05 was considered significant and
the IBM SPSS 23® software in its version for Windows® was used.
Ethics statement
This research was approved by the Institutional Research Bioethics Committee of the HMALL (resolution
No. 6-263-2022), accredited by the Central Ethics Committee of the Ministry of Health of the provincia
de Buenos Aires, under No. 105/2013, with last reaccreditation on 09/09/2022. Strict confidentiality was
guaranteed in the handling of the data provided by the personal data protection law 25 326 and was
conducted in accordance with the guidelines established by the modified declaration of Helsinki.
RESULTS
During the time period covered by the study, a total of 1106 patients were admitted to the ICU, of which
12.75 % (141/1106) required a tracheostomy. Of these 141 patients, 9 were excluded an those are a total
of 132. Two cohorts were established based on fasting time (>3 hours or ≤3 hours). The cohort with
fasting ≤3 hours was made up of 15 patients, while the cohort with fasting >3 hours was made up of 117.
The cohort with fasting ≤3 hours had a median age of 53 years (IR 16), a proportion of male patients of
80 % (12/15), a median number of days of MVA until the procedure of 13 days (IR 6), a median fasting
time of 2.5 hours (IR 1) and a positive previous pneumonia diagnosis of 25 % (3/15). Regarding the
reason for hospitalization, it was identified that within this group 40% (6/15) presented a respiratory
emergency, 33.3 % (5/15) a neurological emergency, and 13.3 % (2/15) a non-neurological surgical
emergency, 6.7% (1/15) had a cardiological emergency and 6.7 % (1/15) had other clinical emergencies,
while the most frequent reason for intubation was respiratory failure with 60 % (9/15). followed by
ventilatory failure with 33.3 % (5/15) and cardio-respiratory arrest with 6.7 % (1/15).
On the other hand, the cohort with fasting >3 hours had a median age of 61 years (IR 27.5), a proportion
of male patients of 59.8 % (70/117), a median number of days of MVA until the procedure of 12 days (IR
5), a median fasting time of 6 hours (IR 4) and a previous positive pneumonia diagnosis of 35.89 %
(42/117). Regarding the reason for hospitalization, it was identified that within this group 26.5 %
(31/117) presented a respiratory emergency, 31.6 % (37/117) a neurological emergency, and 14.5 %
(17/117) a non-neurological surgical emergency, 7.7 % (9/117) had a cardiological emergency and 9.4 %
(11/117) had other clinical emergencies, while the most frequent reason for intubation was respiratory
failure with 52.1 % (61/117), followed by ventilatory failure with 42.7 % (50/117) and
cardio-respiratory arrest with 5.1 % (6/117). When comparing the baseline characteristics previously
described in each cohort, p values >0.05 were obtained for the statistical tests used in each of the
variables.
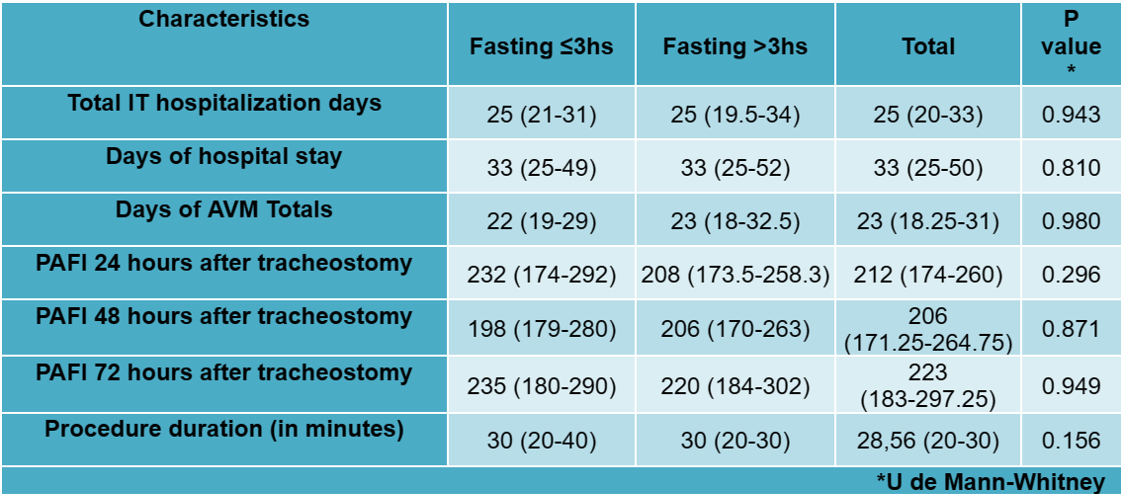
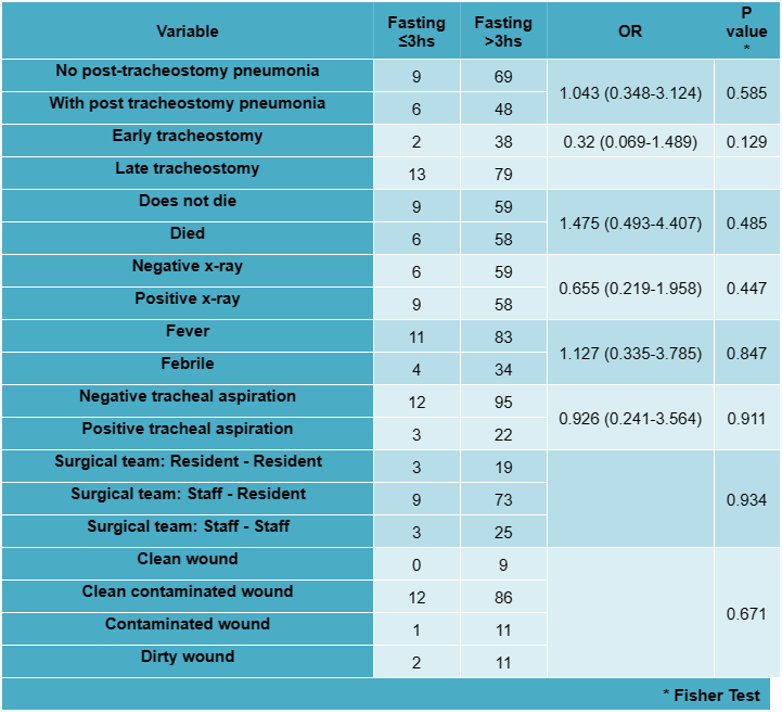
Regarding the bivariate analysis, when analyzing the association between the appearance of
post-tracheostomy pneumonia according to the fasting time, an OR of 1.043 (95% CI: 0.348-3.124) was
obtained with a P value for the chi-square test of 0.585. The analysis of the rest of the variables of
interest can be seen summarized in table 1 and table 2. Given the retrospective characteristic of the
established cohorts, a power of 12.6 % was calculated for the pooled sample. The multivariate analysis
multiple regressions showed the same trend and obtained an OR of 0.90 (95 % CI: 0.69; 1.17), 0.81 (95 %
CI: 0.40; 1.64) and 2.19 (95 % CI: 0.97; 4.96) for the reason for hospitalization, reason for intubation
and previous pneumonia.
DISCUSSION
This study represents a valuable approach when examining the impact of fasting in patients with
tracheostomies, given that there is little scientific evidence available on this topic. Although fasting
before tracheostomy is a common practice in daily clinical care, there is a lack of solid local evidence
that justifies the current fasting protocol, making it crucial to consider this aspect as a relevant
indicator when evaluating the quality of tracheostomy medical attention. The results of this study
highlight the high frequency of patients requiring tracheostomy in our service, coinciding with
international data where references are made to similar statistics describing a 10 to 14 % frequency of
this procedure (1,1).
The results of our study provide relevant evidence about the safety of performing the with a short fast
without increasing the risk of developing pneumonia an prolongs the ICU or hospital stay or worsening
mortality. These data are consistent with what was expressed in the experience published by Hartl T et
al., who implemented a protocol without fasting prior to performing the procedure and found results
clearly in favor of the alternative mentioned before (1). It should be noted
that currently there is no
clear indication of the most appropriate time to avoid complications and guarantee a good nutritional
intake in these patients, which is supported by evidence. In fact, in Gonik's study carried out in 2016
(1); statistically significant differences have not been found when
comparing the group that received a
40-minute fast compared to the control group that received a 6-hour fast.
On the other hand, a survey conducted in the critical care and anesthesia departments found significant
variability in internal protocols. Surgical ICU were noted to have shorter fasting periods for
procedures compared to ICU and anesthesia departments (4 vs. 6 hours). However, in all specialties, wide
fasting ranges were observed for tracheostomies (between 0-8 hours) (1).
Likewise, anesthesia guidelines
have few references to fasting times, especially in critically ill patients. Shime et al. found that 90
% of Japanese anesthesia departments used longer fasts than recommended (21). Others have noted that
fasts for solids actually ranged from 12 to 14 hours instead of 6 to 8 hours and can last up to 37 hours
(20, 21).
Pousman et al. described short fasts for patients receiving jejunal feedings (22). Using a 45-minute
fast before bedside procedures, they noted no change in ventilator-associated pneumonias compared to
controls and a trend toward increased caloric intake. In a review of aspiration, Warner et al identified
only 68 cases of aspiration in 215 000 general anesthesia procedures (13).
All aspirations occurred
before, after, or during airway manipulations and during induction or emergence of anesthesia. At such
times, the airway is more susceptible to aspiration of gastric contents, since the patient is lying down
with abolished protective reflexes and low esophageal tone. Even in high-risk emergency intubations, the
factor that predisposes patients to the highest risk of aspiration is multiple intubations attempts and
the need for mask ventilation that can inflate the stomach (23).
These promising results should be considered the first step towards a change of approach in the ICU. It
is essential to generate solid evidence before implementing any change in clinical practice, so it is
planned to continue this study with a prospective analysis, taking into account the limitations
identified in this work.
One of the limitations of our study lies in its retrospective design, so we recognize the need to
develop a protocol that allows prospective follow-up of patients, which will surely improve the quality
and reliability of the data in question, adding nutritional parameters that enrich the debate. This
prospective approach will allow us to collect more detailed and precise information on the effects of
fasting in patients with tracheostomies and improve the sample size necessary to increase the power of
the study given the low incidence of events.
CONCLUSIONS
No significant differences were found regarding the risk of pneumonia, days of hospital stay, PAFI
values or mortality with respect to fasting time prior to the tracheostomy procedure.
It is important to highlight the importance of nutrition in critically ill patients, so it is pertinent
to optimize fasting times. This is consistent with the limited results obtained in other countries,
which adapted to our context and allows us to avoid postponing the procedure.
Authorship contributions:
Conceptualization: DLG, BME, and QAN. Acquisition, analysis, or interpretation of the data:
DLG, BME, QAN. Statistical analysis: DLG and OMJ. Drafting of the manuscript and editing:
DLG, BME, QAN, CM, MAV, OMJ, CF, MVT, MFMG, MMWE, GNA, ZLNI, EFE, OM, ZOP, PM.
Financing:
This research did not receive any specific grant from funding agencies in the public,
commercial, or not-for-profit sectors.
Declaration of conflict of interest:
The authors declare that they have no known competing financial interests or personal
relationships that could have appeared to influence the work reported in this paper.
Recevied:
December 4, 2023
Approved:
February 28, 2024
Correspondence author:
DURAN, Lucas Gonzalo, Servicio de Terapia Intensiva, Hospital Municipal de Agudos Dr.
Leónidas Lucero
Address:
Estomba 968, Bahía Blanca (8000), Buenos Aires, Argentina
Phone:
-
E-mail:
lucas.duran@uns.edu.ar
Article published by the Journal of the faculty of Human Medicine of the Ricardo Palma University. It is an open access article, distributed under the terms of the Creatvie Commons license: Creative Commons Attribution 4.0 International, CC BY 4.0 (https://creativecommons.org/licenses/by/1.0/), that allows non-commercial use, distribution and reproduction in any medium, provided that the original work is duly cited. For commercial use, please contact revista.medicina@urp.edu.pe.
BIBLIOGRAPHIC REFERENCES