ORIGINAL ARTICLE
REVISTA DE LA FACULTAD DE MEDICINA HUMANA 2024 - Universidad Ricardo Palma10.25176/RFMH.v24i2.6178
FREQUENCY AND ASSOCIATED FACTORS OF MENTAL HEALTH PROBLEMS IN COVID-19 VACCINATED WORKERS AT A PERUVIAN PUBLIC HOSPITAL
FRECUENCIA Y FACTORES ASOCIADOS A PROBLEMAS DE SALUD MENTAL EN TRABAJADORES VACUNADOS CONTRA EL COVID-19 DE UN HOSPITAL PÚBLICO PERUANO
José Raúl Collantes-Schmidt
 1,a
1,a
Belén Virrueta-De La Sota
 1,a
1,a
Marlon Yovera-Aldana
 2,b
2,b
Marco Antonio Bautista-Macedo
 1,c
1,c
1 Universidad Científica del Sur. Lima, Perú
2 Grupo de Investigación Neurociencias, Efectividad Clínica y Salud Pública. Universidad
Científica del Sur, Lima, Perú.
a Graduate of the Master's Degree in Occupational and Environmental Medicine
b Master in Clinical Epidemiology
c Master in Risk Prevention and Occupational Health
ABSTRACT
Introduction: The pandemic increased stress and underdiagnosed mental health issues in the
workplace.
Objetive: To determine the frequency of mental health problems and their associated factors among
vaccinated workers at the Dos de Mayo National Hospital (HNDM).
Methods: A cross-sectional analytical study was conducted using secondary data from a mental
health survey carried out by the HNDM Mental Health Service in October 2021. The Self-Reporting
Questionnaire (SRQ) was administered to all HNDM workers who had received the full vaccination scheme.
Statistical analysis included chi-square tests and logistic regression to identify associated factors.
Results: Of 2109 workers, 2.7% presented mental health problems, with a higher prevalence in
women (3.4%) compared to men (1.5%), and more frequent in the age groups 18-29 years (4.8%) and 50-59
years (4%). Divorced/separated individuals (7%) had a higher prevalence compared to single (2.8%) or
married (2%) individuals. Multivariate analysis indicated a positive association with women (ORa: 2.30;
95% CI: 1.22-4.84) and divorced/separated individuals (ORa: 3.00; 95% CI: 1.12-7.25) compared to
married/cohabiting individuals. There was a negative association in the 30-39 years (ORa: 0.43, 95% CI:
0.19-0.96) and 40-49 years (ORa: 0.30, 95% CI: 0.11-0.81) age groups compared to 18-29 years. No
significant associations were found for other variables.
Conclusion: One in forty HNDM workers presented mental health problems, with higher risks
observed among women, younger and older age groups, and divorced/separated individuals. Improved
screening and support for early intervention are recommended.
Keywords: Mental Health; COVID-19; Vaccination; Health Personnel (source: MeSH NLM)
RESUMEN
Introducción: La pandemia aumentó el estrés y los problemas de salud mental subdiagnosticados en
el trabajo.
Objetivo: Determinar la frecuencia de problemas de salud mental y sus factores asociados en
trabajadores vacunados del Hospital Nacional Dos de Mayo (HNDM).
Métodos: Se realizó un estudio transversal-analítico utilizando datos secundarios de una encuesta
de salud mental llevada a cabo por el Servicio de Salud Mental del HNDM en octubre de 2021. Se
administró el Self-Reporting Questionnaire (SRQ) a todos los trabajadores del HNDM que habían recibido
el esquema completo de vacunación. El análisis estadístico incluyó pruebas de chi-cuadrado y regresión
logística para identificar factores asociados.
Resultados: De 2109, el 2,7% de los trabajadores presentaron problemas de salud mental. 3,4% en
mujeres y 1,5% en hombres y fue más frecuente en los grupos de edad de 18-29 años (4,8%) y 50-59 años
(4%); así como en las personas divorciadas/separadas (7%) que las solteras (2,8%) o casadas (2%). El
análisis multivariado indicó asociación positiva con mujeres (ORa: 2,30; IC 95%: 1,22-4,84) y personas
divorciadas/separadas (ORa: 3,00; IC 95%: 1,12-7,25) frente a casados/convivientes. Hubo una asociación
negativa en los grupos de 30-39 años (ORa: 0.43, IC 95%: 0.19-0.96) y 40-49 años (ORa: 0.30, IC 95%:
0.11-0.81) frente a 18-29 años. No se encontraron asociaciones significativas para otras variables.
Conclusión: Uno de cada cuarenta trabajadores del HNDM presentó problemas de salud mental, con
mayores riesgos observados entre mujeres, grupos etarios más jóvenes y mayores, y personas
divorciadas/separadas. Se recomienda mejorar tamizaje y apoyo para intervención temprana.
Palabras clave: Salud mental; COVID-19; Vacunación; Personal sanitario (fuente: DeCS- BIREME)
INTRODUCTION
Mental health problems are underdiagnosed conditions in the workplace. There are prejudices and feelings
of self-criticism among workers, making early diagnosis and subsequent management difficult (1, 2). When the COVID-19 pandemic began in 2020, it added a
new work-related stress situation, leading to an increase in mental health problems (3). This prompted the Ministry of Health to implement regulations to
diagnose and improve working conditions, provide psychological support, and establish mechanisms to
promote mental health and prevent mental disorders (4).
Locally, high prevalences of depression (45.9%), anxiety (40.2%), and stress (49.0%) have been reported
among healthcare workers during the early stages of the COVID-19 pandemic (5), similar to those found in other parts of Latin America (6). In the United Kingdom, a large percentage (58%) of staff reported
difficulty coping with these problems and communicating them to their superiors, leading to the use of
alcohol, cigarettes, and other substances, exacerbated by social restrictions (7). In a humanitarian aid group in Africa, a prevalence of depression and
anxiety of 39% was shown (8).
Similarly, there was an increase in the incidence of depressive symptoms in the general population
(9), indirectly reflecting a progression in all work areas, not just in
critical care areas (10). Global systematic reviews have compared the
frequency of mental health problems during the COVID-19 pandemic between healthcare workers and those in
other areas, showing similar levels of distress but differing in causes (11). In a Dublin hospital in 2020, health personnel showed 20.3% and 21%
moderate intensity depression and anxiety, respectively. However, a considerable portion of the total
respondents (22%) were administrative staff, and this group had the highest scores. Therefore, it is
essential to also consider this labor group (12).
Additionally, the factors associated with mental health problems among healthcare personnel are multiple
and complex (13). They are related to conditions such as long working hours
and chronic stress (14). However, information on the disease burden that
includes all personnel and not just clinical staff is limited (15).
Considering a context where more than 50% of healthcare personnel had received the second dose of the
COVID-19 vaccine and the effectiveness in reducing mortality and severe disease was evident (16), this study aimed to determine the frequency of mental health problems
and their associated factors among vaccinated workers against COVID-19 at the Hospital Nacional Dos de
Mayo (HNDM) in 2021.
METHODS
Design and Study Area
The research had a cross-sectional-analytical design based on secondary analysis of a database created
by the HNDM mental health service in relation to the Health Surveillance and Care Plan for workers in
the context of the COVID-19 pandemic, carried out in October 2021. The HNDM is a Peruvian public
hospital managed by the Ministry of Health of Peru. It is located in central Lima and, according to its
complexity level, is classified as a III-1 hospital. At the beginning of the COVID-19 pandemic, it was
designated by the government as one of five referral hospitals for the care of coronavirus-affected
patients (17).
Population and Sample
Our study included all records with complete responses from the Self-Reporting Questionnaire (SRQ). The
original survey included all healthcare or administrative workers of the hospital who had received the
complete vaccination scheme at the time of evaluation and agreed to answer the questionnaire; therefore,
no sampling was done. The original survey was sequentially applied to the entire population present
during the third COVID-19 vaccination dose. No initial sample size was calculated for frequency and
associated factors. However, the sample size power was calculated for both, detailed in the analysis
plan section.
For statistical power calculation, the STATA 18 program was used. To estimate power for prevalence
calculation, we used the command power oneproportion. We estimated obtaining a difference in proportion
between 0.025 to 0.80, considering a prevalence of mental health problems of 0.83 (18). We obtained similar powers of 99.9% for both limits. Regarding
associated factors, the power twoproportions or artbin formula was used, depending on whether they had
two or more than two categories, respectively. We found a power for the sex variable of 80.7% and for
the education level of 7%. For age group, marital status, position, and work area, a similar power of
56% was obtained.
Variables and Instruments
A person was considered a positive case of mental health problems if they had at least five positive
responses out of a total of thirteen on the SRQ. The WHO SRQ questionnaire, designed between 1978 and
1993, has a sensitivity of 62.9% to 90% and a specificity of 44% to 95.2%. The Technical Guide for
Mental Health Care for Health Personnel in the Context of COVID-19 by the Ministry of Health of Peru
(MINSA), developed in 2020, recommends it as an adapted and validated instrument for use in health
facilities in Metropolitan Lima, with Ministerial Resolution No. 186-2020-MINSA.
Regarding other variables, age was categorized as 18 to 29; 30 to 39; 40 to 49; 50 to 59; and 60 or
older years; sex (male or female); education level (complete or incomplete secondary, technical, and
higher); marital status (single, married, divorced or separated, cohabiting, and widowed); occupational
group (doctors, nurses, other health professionals, nursing technicians, other health
technicians/assistants, and administrative/general services) and work area (emergencies and critical
areas, hospitalization, outpatient consultation, diagnostic support, and administrative offices).
The "other health professionals" category included obstetricians, nutritionists, psychologists, physical
therapists, etc., excluding the already indicated nursing group. The "other health technicians and
assistants" group included laboratory technicians, radiology technicians, among others. The
administrative/general services group included workers not directly related to healthcare work: lawyers,
journalists, engineers, system programmers, auditors, maintenance, or other related personnel.
Regarding work areas, emergency and critical areas included all emergency areas (adult, pediatric, and
gynecology-obstetrics), regardless of whether they were differentiated as COVID-19 areas, as well as
intensive care units (adult ICU, pediatric ICU, and intermediate care unit). It also included the
pharmacy and emergency cash desk area. In the case of hospitalization areas, the hospitalization rooms,
chemotherapy environments, delivery rooms, and obstetric center adjacent to patient admission areas were
considered. For outpatient consultation, all outpatient consultation rooms used for ambulatory care were
considered. In some services, due to the lack of an exclusive office environment, the consultation room
was used as an office outside user care hours. In all other cases, administrative offices included the
offices of healthcare services as well as other purely administrative function offices such as
insurance, economy, personnel, logistics, planning, etc. Finally, diagnostic support areas included
pharmacy, laboratory, clinical pathology, blood bank, anatomical pathology, and imaging environments.
Procedures
Authorization was requested to conduct the research and access the data from the HNDM Mental Health
Service, which contained the results of the mental health screening surveys conducted as part of the
Health Surveillance and Care Plan, approved with Directoral Resolution 073-2020, based on MINSA
Directives specified in the Technical Guide for Mental Health Care for Health Personnel in the Context
of COVID-19, approved with Ministerial Resolution 180-2020-MINSA.
The initial survey was conducted by the HNDM Mental Health Service. It was carried out in the hospital's
outpatient area from October 18 to 30, 2021, during the third COVID-19 immunization for healthcare
personnel. Psychology staff handed a sheet with the abbreviated SRQ questionnaire to the worker,
providing the respective explanation for marking their responses and allowing 20 minutes for its
completion. The data were then recorded in a spreadsheet.
Statistical Analysis
We used Stata Version 15.1 (Stata Corp, College Station, TX, USA). The absolute and relative frequencies
of the workers' demographic and labor characteristics were reported. Prevalence was calculated by
dividing the number of positive results with more than five responses in relation to the total screened,
and it was also calculated according to baseline characteristic categories.
We assessed whether there was an association between the presence of mental health problems and baseline
characteristics using the Chi-Square test. If the assumption that expected frequencies were less than 5
in more than 20% of the cells was not met, Fisher's exact test was used.
Crude and adjusted odds ratios (OR) with their 95% confidence intervals were estimated using binary
logistic regression analysis. Adjustment was made with variables that had a p-value less than 0.2.
Collinearity and independence of factors were evaluated. For all hypothesis tests, an alpha value of 5%
was used.
Ethical Aspects
The research was approved by the Institutional Ethics Committee in Research of the Universidad
Científica del Sur with Certificate No. 355-CIEI-CIENTÍFICA-2022, and the HNDM Biomedical Research
Ethics Committee gave a favorable opinion on February 23, 2023, with evaluation No. 018-2023-CEIB-HNDM.
RESULTS
General characteristics
The total number of records in the database at the start was 2,378. Of these, 269 were incomplete and
did not meet the study's eligibility criteria. Therefore, the included records were 2,109.
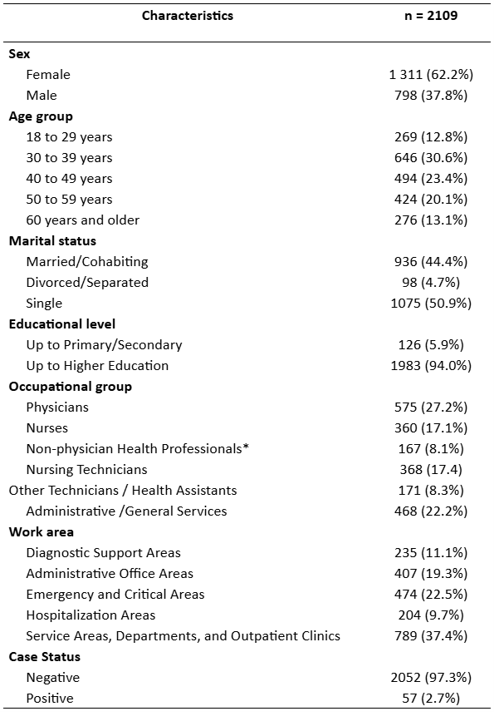
In the included population, females predominated at 62.2%, and the group under 40 years old represented
43.4%. Regarding marital status, 50.9% were single. Additionally, 94% had higher education, and nursing
staff represented 44% of the surveyed population. According to the work area, personnel in service areas
and outpatient clinics predominated, comprising 37.4% (Table 1).
Table 1. Descriptive characteristics of the study sample
* Psychologists (5), nutritionists (33), obstetricians (36), medical technologists (70), pharmacists (33), dentists (4).
Prevalence of mental health problems
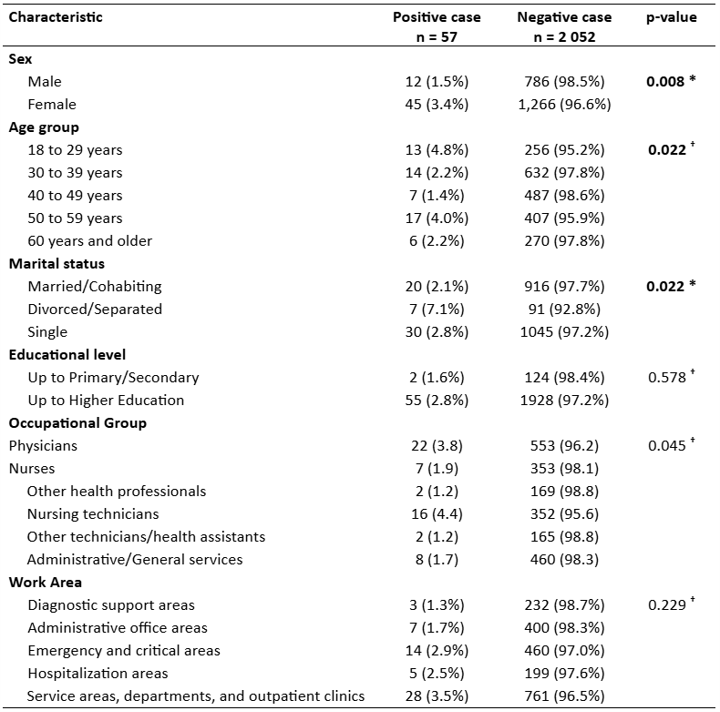
The prevalence of mental health problems was 2.7%. It was more frequent in women than in men (3.4% vs.
1.5%; p=0.008). The highest prevalence was found among those aged 18 to 29 years and 50 to 59 years,
showing a bimodal distribution (p=0.022). Regarding marital status, divorced/separated individuals
reached 7%, compared to single or married individuals who were at 2% (p=0.022). For different
educational levels, positions, or work areas, the prevalence of mental health problems was similar.
Regarding occupational groups, the highest percentage was observed in nursing technicians, followed by
physicians (p=0.045) (Table 2).
Table 2. Factors associated with having a positive case of mental health problems
*Chi-square test of independence. † Fisher’s exact test.
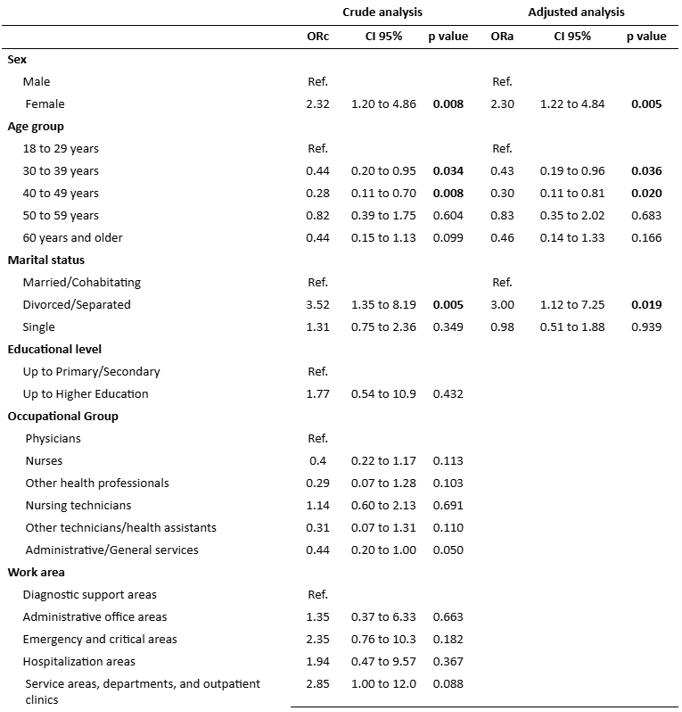
Multivariate Analysis
In the multivariate analysis, women had 1.3 times higher risk of having mental health problems (ORa:
2.30; CI 95%: 1.22 to 4.76; p=0.005). The age group of 30 to 39 years had a 57% lower risk of mental
health problems compared to the 18 to 29 years age group (ORa: 0.43; CI 95%: 0.19 to 0.96; p=0.036). A
similarly lower risk was observed in the 40 to 49 years age group, with a 70% reduction (ORa: 0.30; CI
95%: 0.11 to 0.81; p=0.010). Regarding marital status, divorced/separated individuals had twice the risk
of mental health problems (ORa: 3.00; CI 95%: 1.12 to 7.25; p=0.019). The rest of the variables did not
show any association (Table 3).
Table 3. Simple and adjusted multivariable regression analysis of factors associated with having a positive case of mental health problems
ORc: Crude Odds Ratio. ORa: Adjusted Odds Ratio. CI95%: Confidence Interval to 95%
DISCUSSION
Our study found a low frequency of mental health problems, with one in 40 workers experiencing some
mental health issue. Among the evaluated factors, female sex, the youngest or oldest age groups, and
divorced/separated individuals were associated with these problems.
The frequency of mental health problems among healthcare personnel during the COVID-19 context varied
depending on geographical area, vaccination status, professional group, and the type of instrument used,
ranging from 47% to 83% in national studies. At the Hospital Regional de Tumbes (18), during the 2020-2021 period, using the SRQ, a high percentage of
workers with some mental health problem (82.9%) was found. This study only considered ICU health
personnel in the COVID area with a sample of only 35 subjects. On the other hand, a study from the
Hospital Regional Docente Las Mercedes in Chiclayo during 2021 (19), with
212 workers, found that 47% of the population had anxious and depressive symptoms, with a higher
frequency in men (76%) and associated with alcohol consumption. This study was conducted among non-COVID
health personnel and used a different version of the SRQ (SRQ-18), so the frequencies might not be
comparable.
We did not find studies describing healthcare and administrative personnel during the pandemic that used
the abbreviated SRQ version suggested by MINSA, making it impossible to compare our results at the
national level. However, we have verified that the abbreviated SRQ version has been successfully used
for screening and treatment in the general population in Lima, where the questionnaire was applied
virtually to 2,027 people, finding 77.9% positive cases and providing psychological intervention in 63%
of cases, achieving a significant reduction in SRQ scores in at least 58% of participants (20). This demonstrates the effectiveness of the tool as a screening and
follow-up instrument. Additionally, there were no prior screenings at HNDM, so it was not possible to
evaluate the change or impact of the COVID-19 pandemic.
Regarding the variables related to a higher prevalence of mental health problems, the female gender is
the most represented in the health area and presents, as in other series, the highest frequency of
stress and depression (6). Regarding age, a meta-analysis conducted in Asia
did not find a relationship with depressive disorders. However, an observational study reported that in
the 31 to 40-year-old groups, fear of infecting their families prevailed, and in the 41 to 50-year-old
groups, concern for their health prevailed. In our case, we can assume a similar motivation, where young
adults (30 to 49 years old) expressed a lower frequency of mental health problems than younger (18 to 29
years old) or older adults. Finally, single/divorced marital status, compared to married individuals,
presented an increased risk. Loneliness and isolation would influence mental health problems such as
depression, as they lack concomitant family emotional support. Although not related, nursing technicians
had the highest prevalence of mental health problems, even higher than doctors. This coincides with
reports of adverse outcomes in personnel during the pandemic, where this occupational group presented
one of the highest frequencies (20).
Explanation of results
Healthcare personnel, regardless of the work area, have been affected by the COVID-19 pandemic in mental
health without distinction (16). However, we are struck by the low disease
burden in our study at this particular moment of the pandemic. We can theorize that, at the time of the
original survey, there was a complete vaccination scheme, and it was conducted while the third dose was
being applied, which may have created an environment of optimism and transitory resilience (21). At the same time, the effectiveness of the vaccine in reducing
mortality and severe cases was demonstrated globally and locally (22). The
non-probabilistic convenience selection of workers may have also influenced it since only those who
attended in person developed the survey, excluding those who worked virtually. Similarly, we must
consider the way the questionnaire was administered, conducted while waiting for their vaccination and
with limited supervision by surveyors.
Research recommendations
Given that the prevalence result of mental health problems differs widely from those reported in
national and international studies, we suggest establishing specific guidelines to apply the SRQ more
accurately or choosing another instrument with better sensitivity. We recommend continuing screening and
expanding information on associated factors to establish a profile of those who might be more
susceptible to these problems and thus be able to act on the environment, recognize warning signs, and
make an early diagnosis for timely intervention. It is essential to remember that mental health problems
affect the quality of patient care and the workers' quality of life.
Limitations and strengths
Among the limitations, we consider that the SRQ questionnaire only allows us to screen and establish the
possibility of a mental health problem without specifying the diagnosis, so it must be confirmed with a
specialized medical evaluation. The evaluated factors do not intend to estimate causality, nor are all
the associated factors that may intervene in the results available. There are factors related to mental
health problems that have not been analyzed in this study; characteristics such as working hours, sleep
hours, and economic status were not considered when applying the mental health screening instrument.
There was no baseline screening of mental health problems in HNDM personnel before the COVID-19 pandemic
to estimate changes in prevalence or factors. As it was conducted concurrently with the COVID-19
vaccination process, there is a possibility that participants did not pay attention to correctly filling
out the questionnaire, did not have enough time to respond, or did not have an adequate environment to
reflect on their answers. Likewise, the surveyed population was limited to those working in person and
did not include workers on sick leave or ill and those with virtual work; however, at the time of the
survey, 90% were under this modality. Also, the convenience capture of workers, i.e., through
non-probabilistic selection, could have led to potential selection bias. We also consider as strengths
that a validated and recommended questionnaire by the Ministry of Health was used to screen for mental
health problems in health sector workers, as well as the sample size of 2,100 subjects, which allows for
establishing the frequency of mental health problems with sufficient power.
CONCLUSION
One in 40 workers who worked in person at HNDM in 2021 had mental health disorders. Associated factors
were female sex, extreme age groups, and divorced/separated marital status. The post-vaccination context
and some methodological limitations express this particular moment and limit its use for future
recommendations. Regardless, the collaboration between mental health areas and Occupational Medicine
should be strengthened to promote optimal working conditions for health personnel, elevated with or
without a pandemic.
Acknowledgments: To the Mental Health Service staff of Hospital Nacional Dos de Mayo for their
collaboration.
Authorship contributions:
JRCS, BVD, and MABM participated in the conception, planning, organization, and execution of
the research. MYA also participated in the review of analysis and results. All authors
contributed to writing the final report and approving the manuscript for publication.
Financing:
Self-funded
Declaration of conflict of interest:
The authors declare no conflict of interest.
Recevied:
December 14, 2023
Approved:
April 29, 2024
Correspondence author:
Marlon Yovera-Aldana
Address:
Jirón San Martín 230 Dpto 502. Magdalena del Mar, Lima, Perú.
Phone:
+51 943990228
E-mail:
myovera@cientifica.edu.pe
Article published by the Journal of the faculty of Human Medicine of the Ricardo Palma University. It is an open access article, distributed under the terms of the Creatvie Commons license: Creative Commons Attribution 4.0 International, CC BY 4.0 (https://creativecommons.org/licenses/by/4.0/), that allows non-commercial use, distribution and reproduction in any medium, provided that the original work is duly cited. For commercial use, please contact revista.medicina@urp.edu.pe.
BIBLIOGRAPHIC REFERENCES