ORIGINAL ARTICLE
REVISTA DE LA FACULTAD DE MEDICINA HUMANA 2024 - Universidad Ricardo Palma10.25176/RFMH.v24i2.6209
QUALITY OF LIFE AND CLINICAL CHARACTERISTICS OF RENAL TRANSPLANT PATIENTS WITH AND WITHOUT CHRONIC RHINOSINUSITIS
CALIDAD DE VIDA Y CARACTERÍSTICAS CLÍNICAS DE PACIENTES CON TRASPLANTE RENAL CON Y SIN RINOSINUSITIS CRÓNICA
Clotilde Margarita Andrade-Bonilla
 1,a
1,a
Josué Helí Flores-Figueroa
 1,b
1,b
Marco Andrés González-Martínez
 2,c
2,c
Arturo García-Galicia
 1,d
1,d
Álvaro José Montiel-Jarquín
 1,e
1,e
Diana López García
 1,c
1,c
Maricarmen Tapia Venancio
 1,c
1,c
Nancy Rosalía Bertado-Ramírez
 1,f
1,f
Jorge Loria Castellanos
 3,g
3,g
1 High Specialty Medical Unit, Hospital de Especialidades de Puebla, National Medical Center
“Gral. de Div. Manuel Ávila Camacho”, Instituto Mexicano del Seguro Social, Puebla de Zaragoza, Mexico.
2 Faculty of Medicine, Universidad Popular Autónoma del Estado de Puebla, Puebla de Zaragoza,
Mexico.
3 Special Health Projects Coordination, Instituto Mexicano del Seguro Social.
a MD, Specialist in Otorhinolaryngology and Head and Neck Surgery, subspecialist in
Otoneurology
b MD, Specialist in Otorhinolaryngology and Head and Neck Surgery
c MD, General Practitioner
d MD, Specialist in Pediatrics. Master in Medical Sciences and Research
e MD, Specialist in General Surgery. Master in Medical Sciences and Research
f MD, Specialist in Neurology
g MD, Specialist in Emergency Medicine
ABSTRACT
Introduction: Transplantation is the treatment of choice for patients with chronic kidney disease
(CKD). It requires immunosuppression, which predisposes to the development of complications; chronic
rhinosinusitis (CRS) is one of the most significant.
Objetive: To compare the characteristics of patients with CKD and without CRS in a renal
transplant protocol at a specialized hospital in Puebla, Mexico.
Methods: A comparative, cross-sectional, retrospective study in patients with CKD and in renal
transplant protocol at a third-level care hospital. The SNOT-22 and Lund-Mackay scales were applied.
Descriptive statistics, Mann-Whitney U tests, Fisher's exact test, and Phi coefficient were used;
p<0.05 was considered significant.
Results: 360 patients were recruited: 49 presented with CRS; prevalence: 13.61%; mean age: 39.22
± 12.09 years and duration of progression: 17.73 ± 5.91 weeks. Naso-sinusal polyposis was present in
14.3%; nasal obstruction in 95.9%; facial pain in 67.3%; rhinorrhea in 49% and hyposmia/anosmia in
40.8%. Associated risk factors: allergy to acetylsalicylic acid (p=0.014) and atopy (p=0.000).
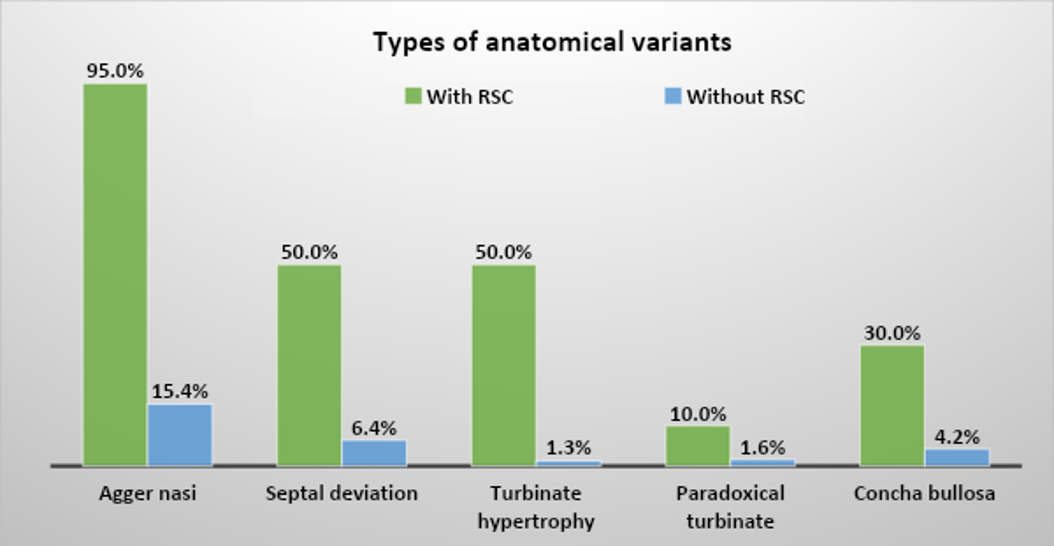
Anatomical variants in patients with and without CRS, respectively: Agger nasi cell 95% and 15.4%;
septal deviation, 50% and 6.4%; turbinate hypertrophy, 50% and 1.3%; concha bullosa, 30% and 4.2%; and
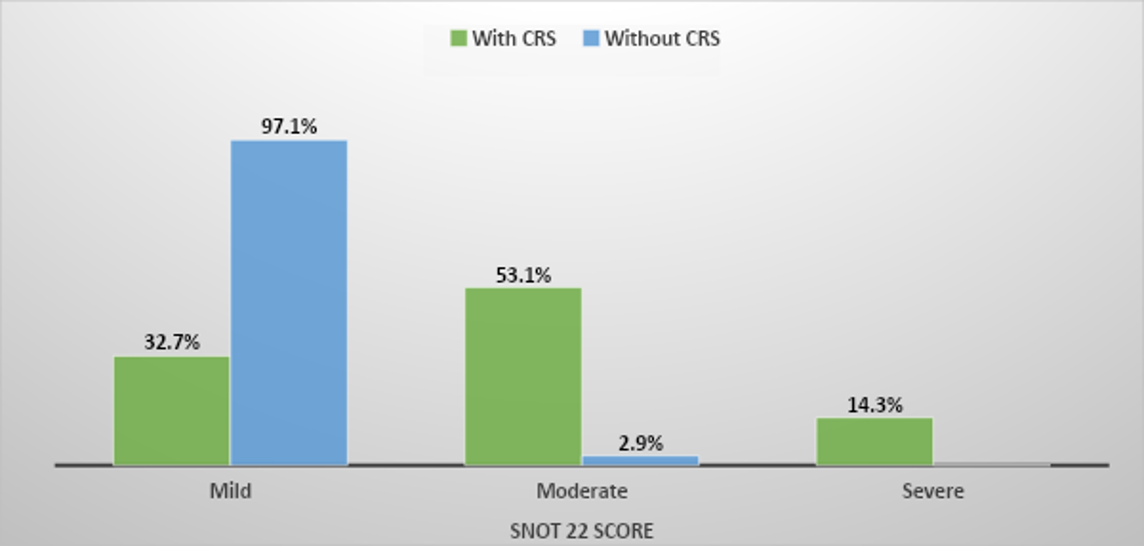
paradoxical turbinate, 10% and 1.6%. The predominant quality of life impact in patients with and without
CRS was moderate at 53.1% and mild at 97.1% (p=0.000).
Conclusion: The prevalence of CRS was 13.61%; the associated risk factors were allergy to
acetylsalicylic acid and atopy, and the predominant anatomical variant was Agger nasi. The tomographic
severity was mild, and the impact on quality of life was moderate.
Keywords: Quality of life, sinusitis, chronic kidney disease, kidney transplantation (source:
MeSH NLM)
RESUMEN
Introducción: El trasplante es el tratamiento de elección en pacientes con enfermedad renal
crónica (ERC). Requiere inmunosupresión, que predispone al desarrollo de complicaciones; la
rinosinusitis crónica (RSC) es una de las más importantes.
Objetivo: Comparar las características de pacientes con ERC con y sin RSC en protocolo de
trasplante en un hospital de concentración en Puebla, en México.
Métodos: Estudio comparativo, transversal, retrospectivo, en pacientes de un hospital de tercer
nivel de atención, con ERC y en protocolo de trasplante renal. Se aplicaron las escalas SNOT-22 y
Lund-Mackay. Se utilizó estadística descriptiva y pruebas U de Mann-Whitney, exacta de Fisher y
coeficiente de Phi; p<0.05, por lo que se consideró significativa.
Resultados: Se reclutaron 360 pacientes: 49 presentaron RSC; prevalencia, 13.61 %; medias edad,
39.22 ±12.09 años y tiempo de evolución, 17.73 ±5.91 semanas. Presentaron poliposis nasosinusal 14.3 %;
obstrucción nasal, 95.9 %; algia facial, 67.3%; rinorrea, 49 % e hiposmia/anosmia, 40.8 %. Factores de
riesgo asociados: alergia a ácido acetilsalicílico (p=0.014) y atopia (p=0.000). Variantes anatómicas en
pacientes con y sin RSC, respectivamente: Celdilla Agger-Nasi 95 % y 15.4 %; desviación septal, 50 % y
6.4 %; hipertrofia de cornetes, 50 % y 1.3 %; concha bullosa, 30 % y 4.2 % y cornete paradójico, 10 % y
1.6 %. La afectación de calidad de vida predominante en pacientes con y sin RSC fue moderada con un 53.1
% y leve, 97.1 % (p=0.000).
Conclusión: La prevalencia de RSC fue 13.61 %; los factores de riesgo asociados, alergia al ácido
acetilsalicílico y atopia y la variante anatómica predominante, Agger-nasal. La severidad tomográfica
fue leve y la afectación de la calidad de vida, moderada.
Palabras clave: Calidad de vida, sinusitis, enfermedad crónica del riñón, trasplante de riñón
(fuente: DeCS- BIREME)
INTRODUCTION
Chronic rhinosinusitis (CRS) is defined as inflammation of the nose and paranasal sinuses lasting at
least 12 weeks (1). It is multifactorial in etiology, but its infectious
origin underscores the
importance of the patient's immune status (2).
Patients with chronic kidney disease (CKD) who are preparing for kidney transplantation receive
immunosuppressive therapy to decrease the likelihood of graft rejection. The resulting exacerbated
immunosuppression state favors infections (3, 4, 5). CRS is one of the most significant infectious
complications and a major factor of morbidity (3). The prevalence of
rhinosinusitis in solid organ
transplant recipients is 12% among adults (5).
The diagnosis of CRS is clinical, and the most commonly used criteria are those established by the
European Position Paper on Rhinosinusitis and Nasal Polyps 2020 (EPOS 2020), which retained the 2012
criteria. These include: purulent rhinorrhea, nasal obstruction, hyposmia/anosmia, and facial pain. At
least two of these cardinal symptoms for 12 weeks and at least one of the first two must be present
(6, 7, 8, 9).
There are two clinical spectra of CRS based on the presence or absence of nasal polyps. Patients with
CRS plus nasal polyps predominantly present with nasal obstruction, hyposmia/anosmia, and rhinorrhea,
while those without nasal polyps show predominant alterations in taste, fatigue, facial pain, and
posterior nasal discharge (10, 11).
CRS is associated with comorbidities such as asthma and chronic obstructive pulmonary disease, allergic
rhinitis, atopy, respiratory disease exacerbated by acetylsalicylic acid, gastroesophageal reflux
disease, and Helicobacter pylori infection (12, 13).
Timely detection of CRS in patients with CKD optimizes decisions and interventions in the preparation
for renal transplantation, reduces morbidity and mortality, and avoids major complications such as graft
rejection and/or death (3).
The aim of this research was to identify the prevalence of CRS, associated risk factors, anatomical
variants, different subtypes, and their clinical characteristics in patients with CKD on protocol for
renal transplantation.
Methods
Study design and area
This was a comparative, cross-sectional, retrospective study at a third-level medical unit of the
Instituto Mexicano del Seguro Social in Puebla, Mexico, from 2017 to 2021.
Population and sample
Patients diagnosed with stage 5 chronic kidney disease of any etiology, in study protocol and management
for kidney transplantation, of any age and gender, were included.
Variables and instruments
The included variables were age, sex, presence of CRS (according to criteria established by EPOS in
2020), duration of CRS, associated comorbidities, clinical symptoms and signs, variants and anatomical
alterations, and affected paranasal sinuses.
Using this information, the following scales were applied:
- SNOT-22 (Sino-Nasal Outcome Test–22): Measures the impact on quality of life and severity of symptoms in patients with CRS. Validated by EPOS 2012, it includes 4 domains: otic and facial symptoms, nasal symptoms, sleep function, and psychological issues. Scores range from 0 to 110, with better quality of life and less clinical severity achieved with lower scores (14). Scores were stratified as: mild 1-36, moderate 37-73, and severe over 74.
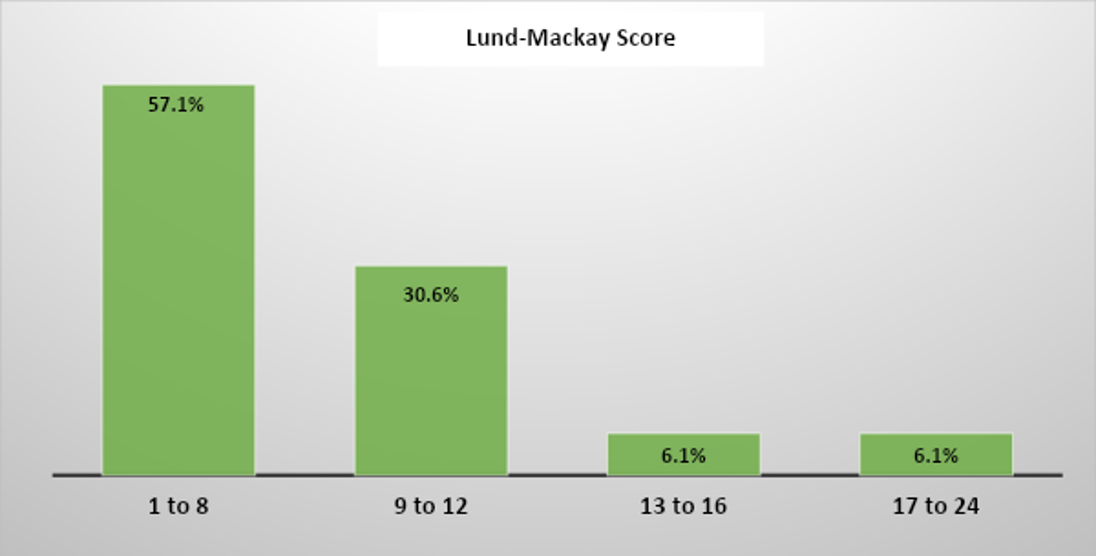
- Lund-Mackay Scale: Identifies tomographic severity of chronic rhinosinusitis and the presence of disease in each paranasal sinus and ostiomeatal complex. The scale scores from 0 to 24, proportional to severity. Scores are stratified as: 1 to 8, 9 to 12, 13 to 16, and 17 to 24 (15).
Procedures
Once the research project was approved by the corresponding Local Health Research Committee, patient
records with CKD in transplantation protocol were reviewed to gather information.
Statistical Analysis
Descriptive statistics were used. Mann-Whitney U was used for the comparison of qualitative variables
and Fisher's exact test and Phi coefficient were used for dichotomous variables. Significant values were
considered at p<0.05. Data were processed in the SPSS program for IBM version 25.
Ethical Considerations
This study was approved by the Local Research Committee in Health 2101 of the Instituto Mexicano del
Seguro Social. Personal data of the patients were handled with strict confidentiality and exclusively
for the purposes of the research.
RESULTS
Out of 360 patients in the renal transplant protocol, 49 had CRS, yielding a prevalence of 13.61%. Those
without CRS had a mean age of 37.3 years (±11.67, minimum 17, maximum 63); 54.7% were composed of 170
men. The mean age of patients with CRS was 39.22 years (±12.09, minimum 21, maximum 61), with a
predominance of females: 53.1% (26 women).
The most frequent respiratory clinical manifestation in CRS patients, in decreasing order of percentage,
was nasal obstruction at 95.9%; facial pain at 67.3%; nasal discharge at 49%, and hyposmia at 40.8%. In
patients without CRS, nasal obstruction was 7.7%; facial pain, 4.2%; nasal discharge, 0.6% and hyposmia,
0.3%.
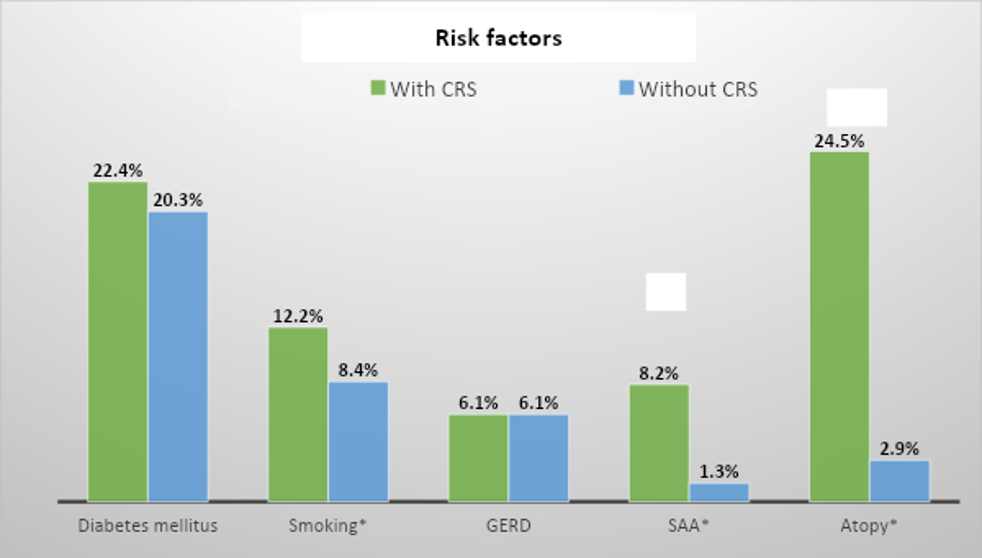
Risk factors present in both groups with similar frequencies were diabetes, smoking, and
gastroesophageal reflux disease. Notable differences were in terms of allergy to acetylsalicylic acid
(p=0.014) and atopy (p=0.000). See figure 1.
Figure 1. Distribution of risk factors in patients with and without chronic rhinosinusitis GERD: Gastroesophageal reflux disease. SAA: Salicylic Acid Allergy. * Factors with significant association (p<0.05).
Regarding physical examination findings, in patients with CRS, edema/hyperemia is the most frequent at
95.9%, followed by mucopurulent meatal discharge at 46.9%. Meanwhile, the only finding in patients
without CRS is mucosal edema at 5.5%. Those with CRS and nasal polyps: 14.3%. Risk factors significantly
related to the presence of nasal polyps were: smoking (p=0.018), allergy to acetylsalicylic acid
(p=0.000), and atopy (p=0.000).
Anatomical variation in CRS occurred in 40.8% of patients; while in patients without CRS it is 16.4%
(p=0.000).
The distribution of the type of anatomical variant in patients with and without chronic rhinosinusitis,
both their percentage and frequency, are represented in Figure 2.
Figure 2. Types of anatomical variants in patients with and without chronic rhinosinusitis
The average duration of illness before the diagnosis of chronic rhinosinusitis was 17.73±5.91 weeks.
The group of paranasal sinuses affected in patients with CRS were, in order of frequency: maxillary
93.9%, ethmoidal 36.7%, sphenoidal 10.2%, and frontal 8.2%.
Regarding the distribution of the Lund-Mackay score in patients with chronic rhinosinusitis, the most
frequent range was from 1 to 8 with 57.1%, followed by 9 to 12 with 30.6%, then 13 to 16 and 17 to 24
with 6.1%, respectively. (See figure 3).
Figure 3: Distribution of the Lund-Mackay score in patients with chronic rhinosinusitis
The SNOT 22 score distribution found in patients with CRS was moderate in 53.1%, followed by mild in 32.7%, and finally severe in 14.3%. In patients without CRS, it was mild in 97.1% and moderate in 2.9% (p=0.000) (See Figure 4).
Figure 4: Distribution of the SNOT 22 score in patients with chronic rhinosinusitis
DISCUSSION
CRS has a high incidence in immunocompetent patients. However, in those preparing for renal
transplantation, it has been little explored and often underdiagnosed. These patients undergo
immunosuppression, both due to the presence of CKD and pre-transplant therapy. Additionally,
comorbidities such as diabetes contribute to immunosuppression (1, 2, 3). This makes patients especially
susceptible to acquiring CRS, which often goes unnoticed. These cases cause additional complications and
increase the possibility of death (3, 4). This study shows
the prevalence of CRS in patients preparing
for renal transplantation treated at a specialized hospital of the Instituto Mexicano del Seguro Social
in Puebla, Mexico. The prevalence found in this study (13.6%) is higher than that reported in South
Korea (4.2%), and very similar to that in the USA (12%) in transplant populations (5, 16). This
reaffirms the importance of deliberate detection in transplant candidate patients.
The age and gender are similar to other reports in similar studies. The female-to-male ratio generally
remains between 45-50 or the reverse, depending on the study (17, 18).
The most frequent clinical manifestations found in this study align with those described in other
populations with CRS: Nasal congestion and discharge, facial pain, and olfactory alterations (19). The
same similarity occurs regarding comorbidities, with predominance of: Atopy/allergy, diabetes, smoking,
sensitivity to acetylsalicylic acid, and gastroesophageal reflux (16). The
prevalence of atopy in
different populations indicates its deliberate search in patients to be transplanted to detect hidden
naso-sinusal disease.
The relatively low frequency of polyps in the CRS patients in this study (14.3%) contrasts with previous
reports in populations without renal pathology (44.6% and 52.6%) (16, 20). This finding requires
subsequent work to confirm this low prevalence of polyps in patients with CKD.
In this study, a significant presence of atopy and allergy to acetylsalicylic acid in patients with
nasal polyps stands out. They make up the so-called Samter's triad, which explains the high prevalence
of respiratory disease exacerbated by this substance in patients with chronic rhinosinusitis (21).
Also, the prevalence of anatomical variants in populations with and without CRS was similar to other
reports, with predominance of Agger nasi and septal deviation. The low frequency of frontal sinus
involvement supports the pathophysiological theory of naso-sinusal mucosal inflammation over mechanical
obstruction in CRS (22). The severity of CRS, in this study, assessed by
the Lund-Mackay scale
(predominantly in stage 1-8), did not differ greatly from other studies of patients with CRS unrelated
to transplants (23).
The quality of life in patients with CRS, in various studies, varies widely from mild to moderate
(20, 24). In our research, the most frequent assessment
was moderate. As a reminder, the construct of quality
of life refers to sociodemographic, cultural, and economic factors that differ according to the surveyed
population (25).
This study is expected to provide necessary information for decision-making in these patients preparing
for transplantation. The deliberate search for these clinical manifestations in these patients and their
timely study favors the early diagnosis of CRS, which can improve their outcome and prevent transplant
failure.
CONCLUSION
The prevalence of chronic rhinosinusitis in patients in the renal transplant protocol in the
central-southern region of Mexico is 13.61%. It predominates in women in their third decade of life. The
associated factors are atopy and allergy to acetylsalicylic acid. The most frequent anatomical variants
are Agger nasi and septal deviation. The most affected paranasal sinuses were the maxillary sinuses, and
the severity was mild by tomography. The quality of life was moderate.
This high prevalence can lead these patients to transplant failure and even death.
Authorship contributions:
CMAB participated in the conception and design of the article, analysis and interpretation
of data, drafting, critical revision, and approval of the final version.
JHFF participated in the conception and design of the article, analysis and interpretation
of data, drafting, and approval of the final version.
MAGM contributed to data analysis and interpretation, critical review of the article,
technical or administrative advice, and approval of the final version.
AGG participated in the article design, data analysis and interpretation, drafting of the
article, critical revision, and approval of the final version.
AJMJ collaborated in data analysis and interpretation, drafting of the article, critical
revision, and approval of the final version.
NRBR participated in data analysis and interpretation, drafting of the article, critical
revision, and approval of the final version.
Financing:
Self-funded
Declaration of conflict of interest:
The authors declare no conflict of interest.
Received:
December 21, 2023
Approved:
April 11, 2024
Correspondence author:
Arturo García-Galicia
Address:
Calle 2 Norte # 2004. Colonia Centro. CP 72000. Puebla, Puebla, México
Phone:
(+51) 998776732
E-mail:
neurogarciagalicia@yahoo.com
Article published by the Journal of the faculty of Human Medicine of the Ricardo Palma University. It is an open access article, distributed under the terms of the Creatvie Commons license: Creative Commons Attribution 4.0 International, CC BY 4.0 (https://creativecommons.org/licenses/by/1.0/), that allows non-commercial use, distribution and reproduction in any medium, provided that the original work is duly cited. For commercial use, please contact revista.medicina@urp.edu.pe.
BIBLIOGRAPHIC REFERENCES