CLINIC CASE
REVISTA DE LA FACULTAD DE MEDICINA HUMANA 2024 - Universidad Ricardo Palma10.25176/RFMH.v24i3.6255
HEART FAILURE WITH RECOVERED LEFT VENTRICULAR EJECTION FRACTION. A CASE REPORT
INSUFICIENCIA CARDIACA CON FRACCIÓN DE EYECCIÓN DEL VENTRICULO IZQUIERDO RECUPERADA. REPORTE DE CASO
Omar Díaz-Cucho
 1,a,b
1,a,b
1 Hospital Alberto Barton Thompson, Callao, Perú.
a Médico cardiólogo.
b Máster en insuficiencia cardíaca.
ABSTRACT
Heart failure with recovered ejection fraction is defined as the improvement of left ventricular
systolic function (LVEF) to values ≥ 40%, after having presented a reduced LVEF (< 40%) at a previous
time and ≥10% absolute improvement in LVEF. It is a chronic and dynamic condition with a high risk
of relapse and deterioration, so close monitoring and optimal medical therapy are essential for its
management. A case is presented of a young male patient with dilated cardiomyopathy with severe left
ventricular systolic dysfunction, who with neurohormonal therapy for heart failure, showed rapid
clinical recovery and improvement of ejection fraction and left ventricular remodeling. Further
studies are needed to better understand this condition and its long-term treatment.
Keywords: Heart failure; pharmacotherapy; dilated cardiomyopathy; ventricular remodeling.
(source: MeSH NLM)
RESUMEN
La insuficiencia cardíaca con fracción de eyección recuperada se define como la mejoría de la
función
sistólica del ventrículo izquierdo (FEVI) hasta valores ≥ 40%, después de haber presentado una FEVI
reducida (< 40%) en un momento previo y con un incremento absoluto de la FEVI ≥10%. Es una condición
crónica y dinámica con alto riesgo de recaída y deterioro, por lo que, el seguimiento estrecho y
la terapia médica óptima son fundamentales para su manejo. Se presenta el caso de un paciente
varón joven con cardiopatía dilatada con grave disfunción sistólica del ventrículo izquierdo,
que con terapia neurohormonal de falla cardiaca, presenta una rápida recuperación clínica y
mejoría de la fracción de eyección y remodelado ventricular izquierdo. Se requieren más estudios
para comprender mejor esta condición y su tratamiento a largo plazo.
Palabras clave: Insuficiencia cardíaca; farmacoterapia; cardiomiopatía dilatada;
remodelación
ventricular.
(fuente: DeCS-BIREME)
INTRODUCTION
Heart failure with recovered ejection fraction is defined as the improvement of left ventricular
systolic function (LVEF) to values ≥40% after having presented a reduced LVEF (<40%) at a previous
time and with an absolute increase in LVEF ≥10%. Although it is associated with lower mortality and
hospitalization than heart failure with reduced or preserved ejection fraction, it remains a chronic and
dynamic condition with a high risk of relapse and deterioration. It is essential to maintain close
follow-up and appropriate medical therapy (1-3). The
evidence related to the improvement of LVEF is still limited, so the objective of this report was to
describe the clinical characteristics, comorbidities, auxiliary examinations and analyze the evolution
of LVEF in a patient with heart failure with recovered ejection fraction.
CLINICAL CASE
37-year-old male from Lima-Peru, cargo transportation supervisor. Male without a history of high blood
pressure, diabetes, ischemic heart disease, or arrhythmias. Mother died suddenly at age 33 with an
apparent cardiac cause by autopsy, maternal uncle with heart failure, maternal uncle with a cardiac
pacemaker. The patient came to the outpatient clinic with an illness of 4 months due to lower limb
edema, palpitations, 3-pillow orthopnea, and progressive exertional dyspnea until reaching mild
exertion. He is found with BP 110/70 mmHg, HR 120 bpm, RR 18x', normal temperature. Weight 95kg, size
170cm. Positive jugular engorgement, edema +++/++++. The cardiovascular examination showed displaced tip
shock, rhythmic, tachycardic heart sounds, presence of third heart sound, and mitral II/VI systolic
murmur. In addition, he had crackles and decreased murmur at the lung bases. The rest of the exam was
non-contributory
The blood count, blood glucose, kidney function, serum electrolytes, thyroid and liver profile were
within normal values. ProBNP was 953 pg/ml. The electrocardiogram showed sinus tachycardia, left axis,
left atrial enlargement, left ventricular hypertrophy, poor r-wave progression in the precordials, and
QRS of 100 ms. The chest x-ray revealed cardiomegaly and pulmonary congestion. Holter monitoring showed
sinus rhythm and simple low-load ventricular extrasystoles. The baseline echocardiogram showed dilated
cardiomyopathy with severely depressed left ventricular systolic function (EF 26%), moderately depressed
right ventricular systolic function (FAC 23%, TAPSE 14mm), grade III diastolic dysfunction, functional
grade II/VI mitral regurgitation, high probability of pulmonary hypertension (PSAP 44mmHg, TAP 72ms).
(Figure 1).
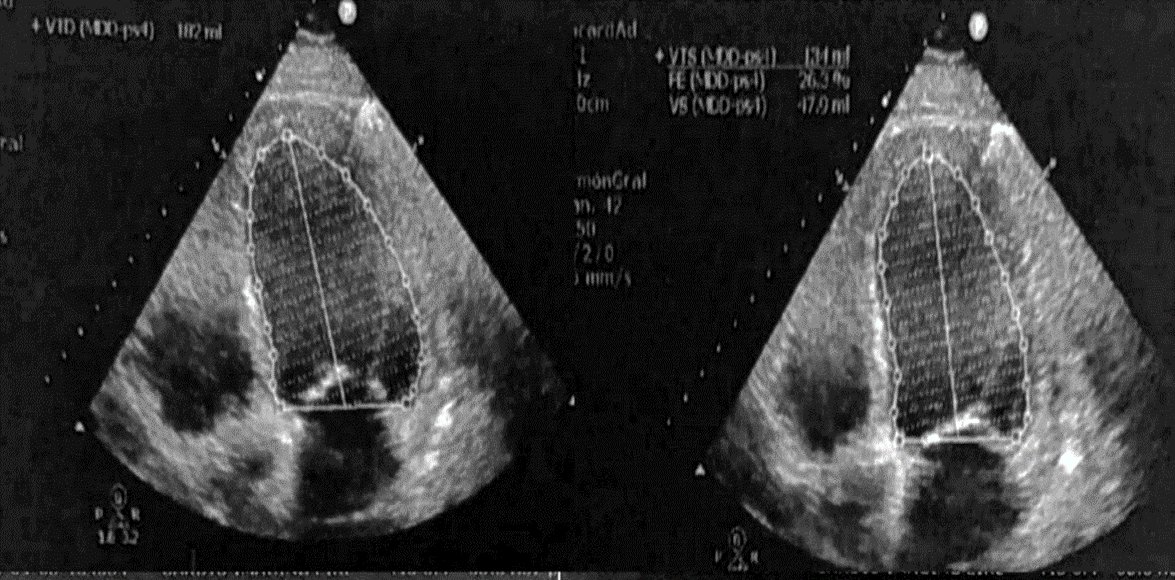
FIGURE 1. Baseline echocardiogram. Shows severely depressed systolic function.
A magnetic resonance study was performed that showed non-ischemic dilated cardiomyopathy, with severe
biventricular systolic dysfunction (LVEF 18% and RVEF 22%), severe biventricular dilation, as well as
intramyocardial linear fibrosis equivalent to 5% of the myocardial mass located in the lateral wall,
anterior and septal of the left ventricle, and, in the lateral and inferior wall of the right ventricle.
Coronary CT angiography showed coronary arteries without significant alterations and a calcium score of
0.
Patient was managed on an outpatient basis due to refusal and fear of being hospitalized during a health
emergency due to Covid-19. Treatment was started with spironolactone 25mg/day, furosemide 40mg bid,
sacubitril/valsartan 50mg bid and water restriction to 1000ml/day. Telephone follow-up was carried out
after two weeks, reporting adherence to treatment, with improvement in orthopnea and edema, but still
with dyspnea on mild exertion. Bisoprolol 2.5 mg/day was added. He attended an in-person appointment
after a month, showing a 10kg weight loss, BP 100/60 mmHg, HR 82bpm, negative jugular engorgement, lower
limb edema +/++++, absence of third sound. Control echocardiogram showed LVEF 30-33% and improvement in
LV filling pressures (figure 2). The dose of sacubitril/valsartan was increased to 100 mg bid,
bisoprolol 5 mg/day. The dose of furosemide was reduced to 40 mg/day, and spironolactone was continued.
Water restriction of up to 1500ml/day is also indicated.
Three months later, it is evident that he tolerates medication. He is found to have BP 110/70 mmHg, HR
70bpm, absence of edema, tolerance of recumbency, and functional class improvement to NYHA II. A control
echocardiogram was performed, showing LVEF 50% with normal diastolic function, even with significant
dilation of the left ventricle (Figure 3). Medication was maintained except for sacubitril/valsartan,
which was suspended as the patient could not afford it. It was changed to enalapril 10 mg bid, with good
adherence and tolerance.
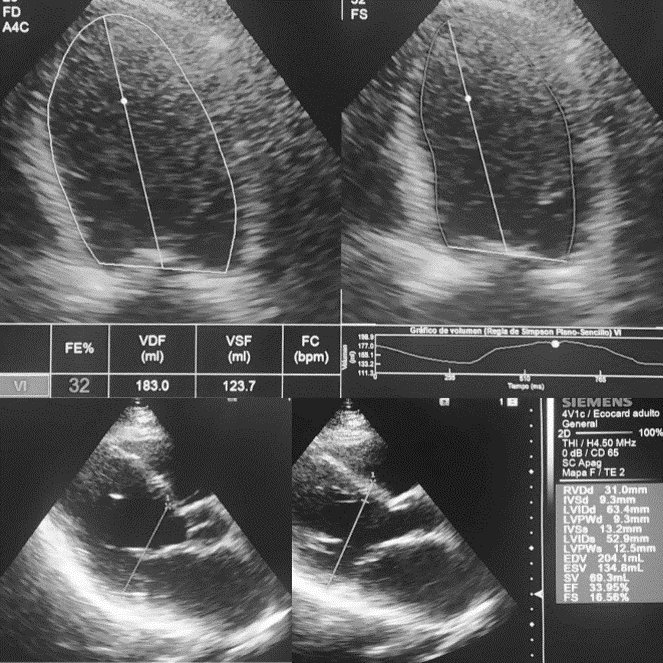
FIGURE 2. Echocardiogram one month after treatment. Presents an increase in FEVI to 33%. Additionally, it was found: TAPSE 20mm, E/e'15, PSAP 38mmHg.
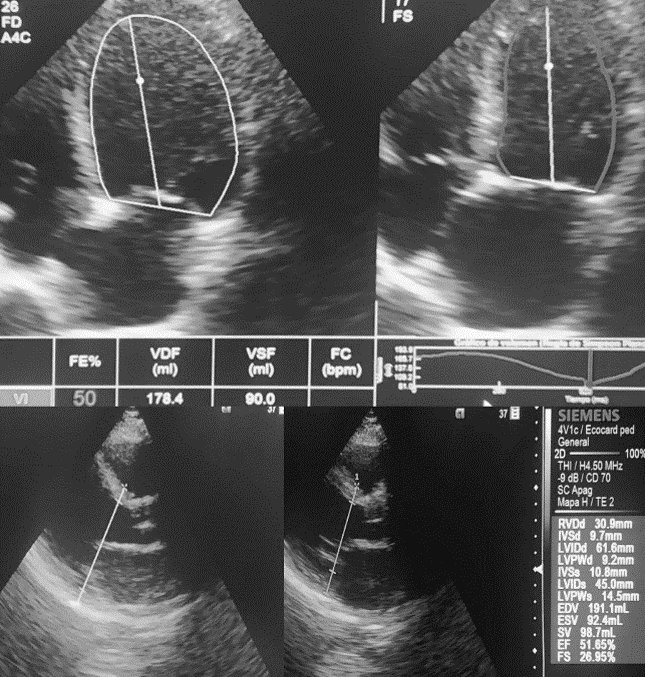
FIGURE 3. Echocardiogram after the third month of treatment. Shows improvement in LVEF to 50%. even with dilation of the left cavities. Also: E/e´6. PSAP 35mmHg.
The echocardiogram after one year showed an LVEF of 65%, normal diastolic function and no dilation of
the left ventricle (figure 4). The follow-up electrocardiogram no longer showed signs of left atrial
enlargement or left ventricular hypertrophy (figure 5). Functional class improvement was observed
through a stress test performed with a beta blocker, in which it reached 70% of the maximum heart rate
and 9.1 METS. It was decided to suspend furosemide, reduce the dose of bisoprolol to 2.5 mg, and
continue with the rest of the medications at established doses. The control showed a good response after
one month.
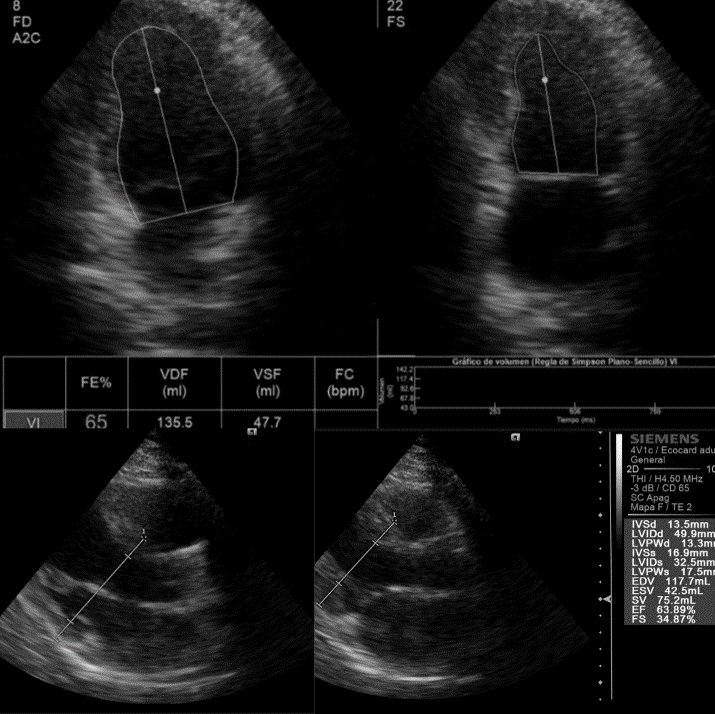
FIGURE 4. Echocardiogram one year after treatment. Preserved LVEF and decreased left ventricular volume are seen.
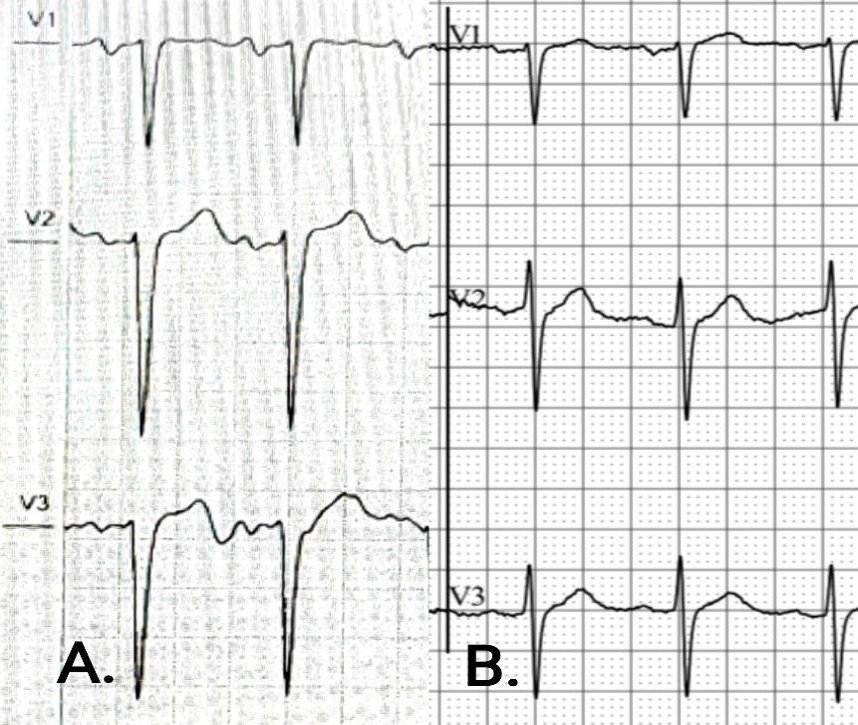
FIGURE 5. A. Baseline ECG. B. ECG at one year. Both taken at 10mm/mV and 25mm/s. Changes in voltage are evident. Mainly lower amplitude in the P wave and S wave, improved R wave progression and less wide QRS complex.
DISCUSSION
Dilated cardiomyopathy is defined as dilation of the left ventricle (or both), associated with depressed
ejection fraction in the absence of hypertensive heart disease, congenital heart disease, coronary
artery disease, and valvular disease. It is the most common indication for heart transplant. Its
etiology can be idiopathic, genetic, viral, autoimmune and toxic (alcohol, drugs). In 50% of cases it is
considered idiopathic. Dilated heart disease has familial origin in 20 to 50% and it should be
considered if it is present in two or more first-degree relatives or in the case of a relative with
sudden death at an early age (4-6).
Dilated heart disease frequently presents as congestive heart failure. To reach the diagnosis, in
addition to a detailed history and a thorough physical examination, it is essential to perform a
transthoracic echocardiogram, since it allows estimating the ejection fraction, estimating ventricular
volumes and ruling out other causes (6). Likewise, magnetic resonance also
has an important role, since it allows identifying the pattern of myocardial fibrosis in late gadolinium
enhancement, which is associated with advanced stages of the disease (7).
Mortality due to dilated heart disease is estimated between 20 to 30% per year, and can reach 50% 2
years after diagnosis. Death is sudden in approximately half of the cases. Optimal medical treatment
with angiotensin-converting enzyme inhibitors, angiotensin II receptor blockers, dual neprilysin and
angiotensin receptor inhibitors, beta-blockers, mineralocorticoid receptor antagonists, and recently,
sodium-glucose cotransporter inhibitors type 2 has significantly reduced mortality in these patients
(2, 3, 6).
In the case presented, our patient showed rapid clinical recovery with neurohormonal management of heart
failure, showing reverse remodeling in the left ventricle and improvement in ejection fraction. Entity
known as heart failure with recovered LVEF, which has different characteristics in etiology,
comorbidities, response to treatment and prognosis compared to failure with reduced or preserved LVEF.
Patients with heart failure with recovered LVEF have an improved quality of life and a lower rate of
hospitalization and mortality (1). Although the patient's recovery could
also be the result of the natural history of a self-limiting background myocardial disease, the current
recommendation is to continue treatment due to the high risk of relapse, as well as close monitoring of
the patient (8-10).
CONCLUSION
It is not uncommon for patients with dilated heart disease to show improvement in LVEF with
neurohormonal treatment, even when myocardial dysfunction has been severe; however, information on the
management of heart failure with recovered LVEF is still limited. The risk of relapse is high.
Therefore, it is advisable to maintain neurohormonal therapy for heart failure. Experimental studies are
required on new therapeutic targets that allow lasting remission of heart failure.
Authorship contributions:
ODC participated as the sole author in the conception of the article, the search for
information, the writing, and the approval of the final version.
Financing:
Self-funded
Declaration of conflict of interest:
The author declares that he has no conflict of interest.
Recevied:
December 31, 2023
Approved:
April 12, 2024
Correspondence author:
Omar Díaz Cucho.
Address:
Jr. Río Chira 552, San Luis, Lima.
Phone:
(+51) 990011235
E-mail:
omardiazcucho@hotmail.com
Article published by the Journal of the faculty of Human Medicine of the Ricardo Palma University. It is an open access article, distributed under the terms of the Creatvie Commons license: Creative Commons Attribution 4.0 International, CC BY 4.0 (https://creativecommons.org/licenses/by/4.0/), that allows non-commercial use, distribution and reproduction in any medium, provided that the original work is duly cited. For commercial use, please contact revista.medicina@urp.edu.pe.
BIBLIOGRAPHIC REFERENCES
