ORIGINAL ARTICLE
REVISTA DE LA FACULTAD DE MEDICINA HUMANA 2024 - Universidad Ricardo Palma10.25176/RFMH.v24i1.6323
ANATOMICAL PREPARATION OF THE VISCERAL ASPECT OF THE HUMAN LIVER TO DEMONSTRATE THE BRANCHES OF THE HEPATIC PORTAL VEIN APPLYING THE LASKOWSKI FILLING, DISSECTION AND CONSERVATION TECHNIQUES
PREPARADO ANATÓMICO DE LA CARA VISCERAL DEL HÍGADO HUMANO PARA EVIDENCIAR LAS RAMAS DE LA VENA PORTA HEPÁTICA APLICANDO LAS TÉCNICAS DE REPLECIÓN, DISECCIÓN Y CONSERVACIÓN LASKOWSKI
Emanuel Balarezo Rebaza
 1,a
1,a
Cesar Pretell León1
 1,a
1,a
Pamela Torres Blas
 1,a
1,a
Athenas Alvaro Montes
 1,a
1,a
Ana Lucero Canales Guevara
 1,a
1,a
1 Universidad Nacional del Santa, Chimbote, Perú
a Medical student - IV semester
ABSTRACT
The human anatomy course is crucial in the education of medical students, and therefore, the shortage of
anatomical specimens poses a challenge in teaching. This study aims to create an anatomical preparation
of the visceral surface of the liver, allowing visualization of the branches of the hepatic portal vein
using the repletion, dissection, and Laskowski preservation techniques. The preparation successfully
revealed the distribution of suprahepatic veins and branches of the portal vein irrigating their
respective segments, without encountering anatomical variations. Through this study, successfully,
produced an anatomical specimen primarily showcasing the branches of the hepatic portal vein. It is
recommended inspecting the anatomical specimen before commencing the work, as well as conducting tests
to determine the appropriate amount of plant dye to use.
Keywords: Anatomy, liver, anatomical preparation, dissection, portal vein (source: MeSH – NLM)
RESUMEN
El curso de anatomía humana es crucial en la formación de los estudiantes de medicina y, debido a ello,
la escasez de preparados anatómicos significa una dificultad en la enseñanza. El presente estudio tiene
como objetivo realizar un preparado anatómico de la cara visceral del hígado que permita visualizar las
ramas de la vena porta hepática mediante la aplicación de las técnicas de repleción, disección y
conservación Laskowski. En el preparado, se logró visualizar la distribución de las venas suprahepáticas
y las ramas de la vena porta que irrigan sus respectivos segmentos, sin encontrar variantes anatómicas.
Mediante este trabajo, se logró crear un preparado anatómico que permite visualizar principalmente las
ramas de la vena porta hepática. Se recomienda realizar una inspección de la pieza anatómica antes de
realizar el trabajo y realizar pruebas para determinar la cantidad adecuada de tinte vegetal a utilizar.
Palabras clave: Anatomía, hígado, preparado anatómico, disección y vena porta (fuente: DeCS –
BIREME)
INTRODUCTION
In the academic career of medical students, the Human Anatomy course is positioned as the essential
basic science that will lay the foundation for their future medical career (1, 2).
Human anatomy constitutes the fundamental pillar of good medical practice and serves as the basis for
clinical studies (3); therefore, it is essential to learn it correctly
through direct contact with
anatomical parts that allow an adequate understanding of the structures studied. For the correct
understanding of this course, the study material must be preserved correctly and neatly; however,
preserving its integrity and preventing its natural decomposition may be adequate without appropriate
techniques (4). The dissection technique will be the favoring tool that
allows separating structures and
accessing certain cavities using a blunt or sharp instrument (4). At the
same time, the study of the
vascular elements will be favored by the technique of filling the hepatic vessels thanks to the
injection of solutions inside (5), to later preserve the organ through the
conservation technique with
glycerin, which replaces formalization, thus avoiding any possible negative impact on the health of
students and teachers (6).
In recent years, our university has been implementing the exhibition of anatomical samples that allow
the student's first-hand visual impression with the appropriate permission of the teacher. However, this
material is still scarce, making it challenging to identify structures in a correct state and without
previous damage. The choice of the topic was inspired by the anatomical preparation exhibited by the
"Juan José Naón" Anatomy Museum located in the Faculty of Medical Sciences of the Universidad de Buenos
Aires, which details with specificity the internal structure of the organ presented, thus allowing way
correct learning for subsequent students and contributing with a new anatomical sample for the
Professional School of Human Medicine, supporting their progress and recognition. As previous works
carried out on the subject include Durand C., Rázuri C. and Cervera A. in Peru in 2018, they sought to
introduce new definitions and proposals related to the anatomy of the liver to improve the understanding
of its structure. They observed 286 human livers of different sexes, races, and ages using techniques
such as dissection, acrylic injection, radiology, and three-dimensional tomographic reconstructions. The
result was the presentation of anatomical definitions for various hepatic elements, such as portal
segments, portal pedicles, portal fissures, and hepatic veins, among others. Furthermore, new anatomical
definitions were proposed. They concluded that these contributions have significantly improved the
detailed understanding of liver structure (7).
Durand C. in 2017 set out to clarify the anatomy of portal segment V, due to divergent interpretations
between authors that generated confusion in research and clinical practice. The research included
evaluating the intrahepatic vascular structure in 200 human livers of both sexes and various ages, using
techniques such as acrylic injection and fresh dissection. A single segmental portal branch was
identified for the right medial division of the liver, notable for its considerable size and specific
divisions. In 80% of cases, this branch originated from the right portal vein. These findings provide
clarity to the anatomy of portal segment V, with the potential to influence the terminology and approach
to liver anatomy and surgery, contributing to a more precise and complete understanding of this
fundamental anatomical structure (8).
Therefore, the present study aims to obtain an anatomical preparation of the visceral side of the human
liver to demonstrate the branches of the hepatic portal vein, applying the repletion, dissection, and
Laskowski conservation techniques.
METHODS:
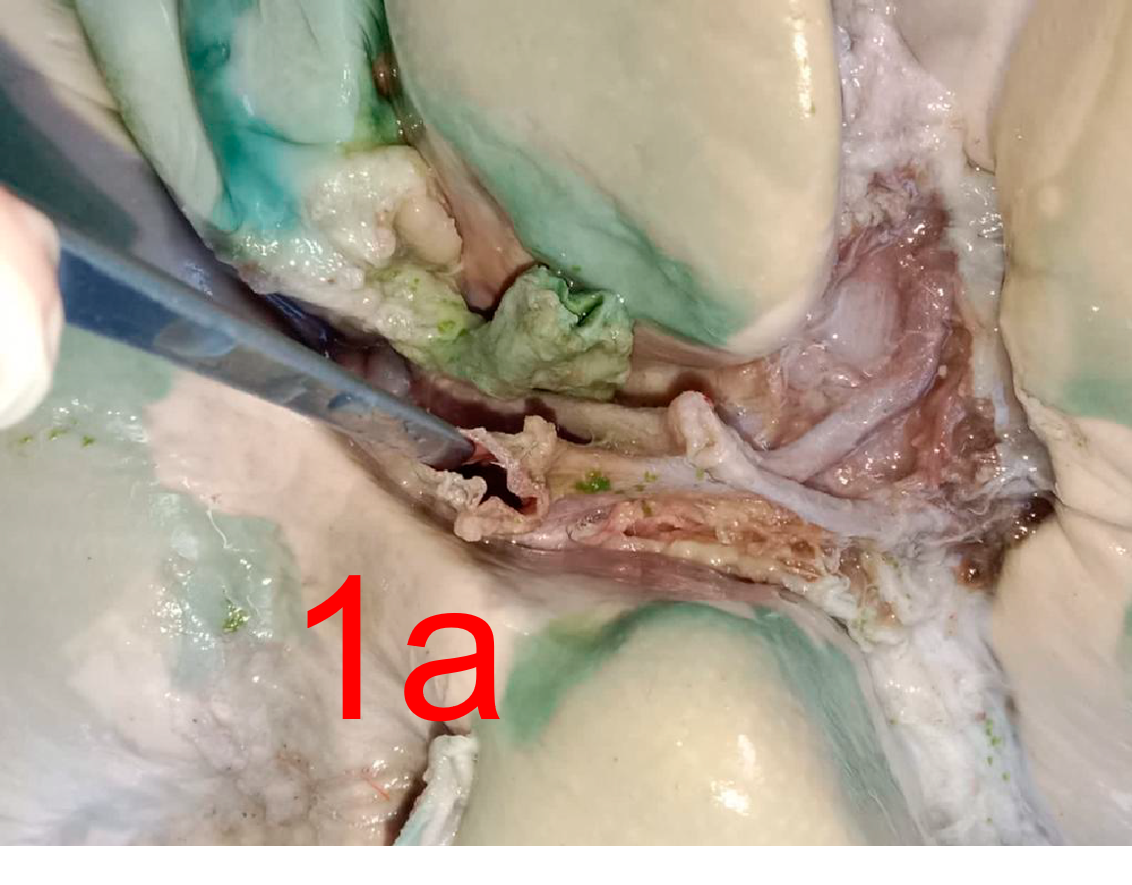
The authors proceeded to fix the human liver in a 10% formaldehyde solution for two weeks. Subsequently,
we cleaned the visceral side of the liver by removing the fat and visceral peritoneum from the hepatic
pedicle with great care trying to isolate the portal vein, the proper hepatic artery and the common
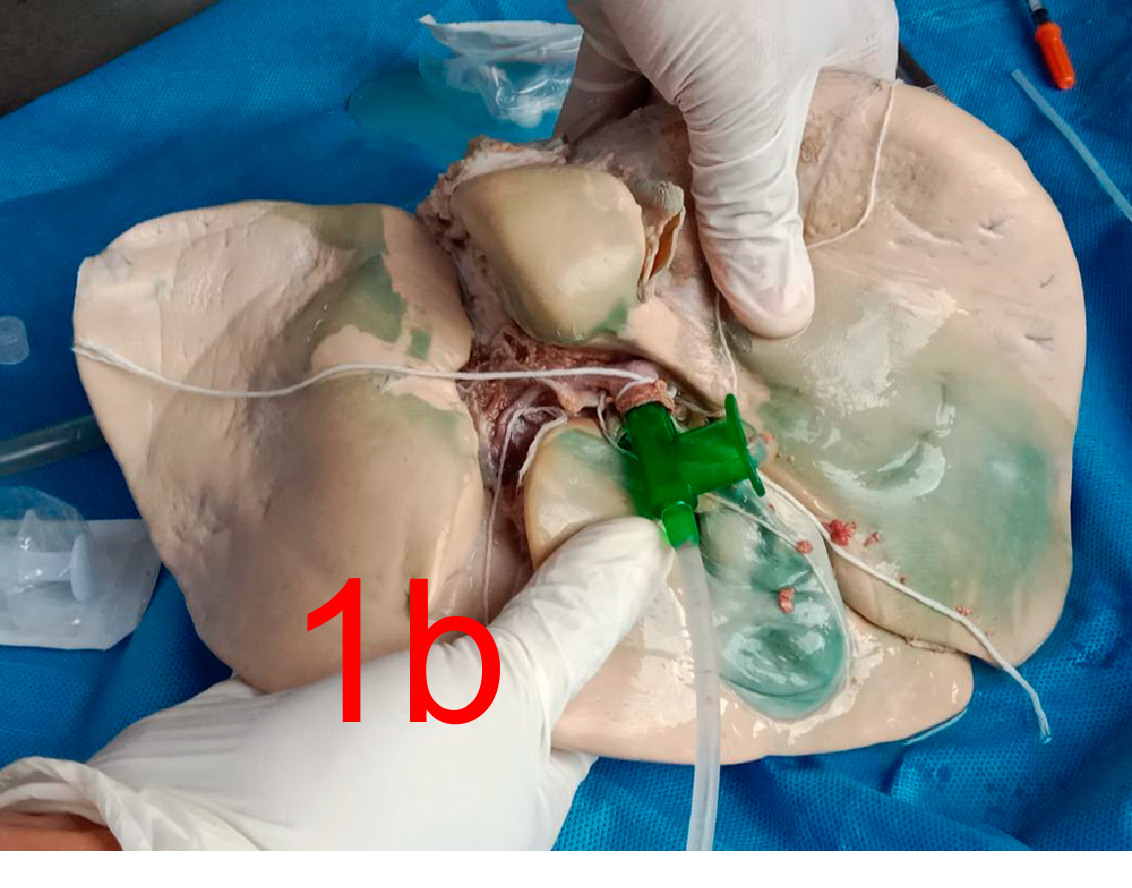
hepatic duct (Figure 1a). Once the hepatic pedicle has been identified, we proceed to canalize the
portal vein, securing the proximal end of the vessel to prevent reflux of the solution (Figure 1b). We
connected a syringe, and with moderate pressure, began to inject the heparin sodium solution diluted in
water to clean the blood vessels. After cleaning the vasculature, we changed the cannulas and, securing
the proximal end of the portal vein, connected a syringe with the latex solution with blue vegetable
ink. Next, with gentle pressure, began to inject the colored latex into the portal vein.
We let it dry for an approximate period of 4 hours. After drying, with a scalpel blade, traced a
circumference starting from the edges on the visceral side of the liver, leaving 1 cm of healthy
parenchyma around the four lobes. Subsequently, with the handle of the scalpel or grooved probe, we
begin to scrape the parenchyma starting from the hepatic pedicle. As we go deeper, we can recognize the
branches of the portal vein for the hepatic segments. We immersed the anatomical piece in 4 L of
Lakowski solution for a period of 30 days. We remove the liver and leave it to dry in a colander for a
period of 7 days. The chocolate color can be seen in all the structures. We painted all the branches of
the holder with glossy acrylic varnish and then matte white acrylic. Finally, we painted all the portal
branches with blue vegetable dye, adding the green tone for the gallbladder and red tone for the evident
hepatic artery.
RESULTS
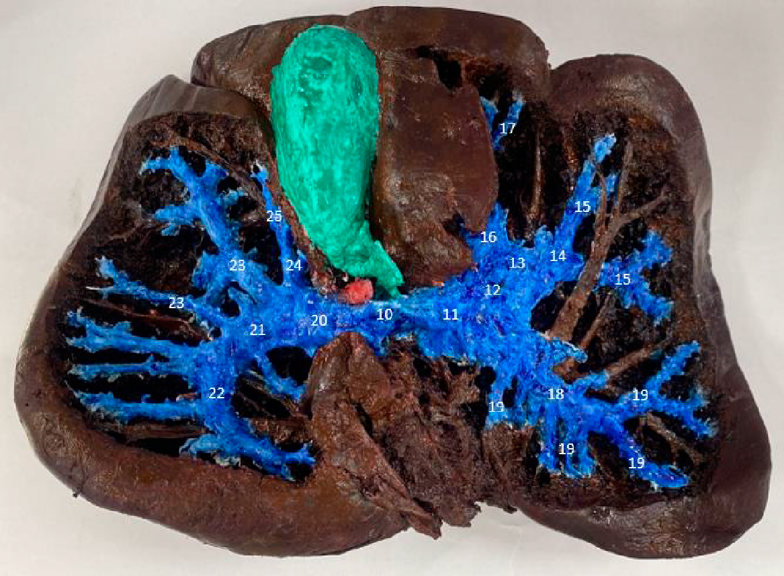
Figure 2 shows the dissection of the visceral side of the human liver, where the following numbered
structures are indicated: (1) Inferior vena cava. (2) Gallbladder. (3) Common bile duct. (4) Proper
hepatic artery. (5) Square lobe of the liver. (6) Caudate lobe of the liver. (7) Right hepatic vein. (8)
Tributaries of the right hepatic vein. (9) Tributaries of the left hepatic vein.
In Figure 3 you can see the dissection of the visceral side of the human liver, where the following numbered structures corresponding to the portal veins and their branches are indicated, (10) Hepatic portal vein. (11) Left branch of the hepatic portal vein. (12) Left paramedian vein. (13) Rex Recess. (14) Left branch of Rex recess. (15) Branches for segment III of the liver. (16) Right branch of Rex recess. (17) Branch for segment IV of the liver. (18) Left lateral vein. (19) Branches for segment II of the liver. (20) Right branch of the hepatic portal vein. (21) Right lateral vein. (22) Branch for segment VII of the liver. (23) Branches for segment VI of the liver. (24) Right paramedian vein. (25) Branch for segment V of the liver.
DISCUSSION
The liver, which stands out as the largest gland in our body, plays a vital role in digestive and
metabolic processes, such as releasing bile to facilitate digestion, as well as secreting and storing
glucose, proteins and clotting factors. It is located in relation superior to the diaphragm, inferior to
the duodenum, and anterior to the stomach (9, 10).
Regarding venous irrigation, the hepatic veins carry all the blood that reaches the liver through the
hepatic artery and portal vein to the inferior vena cava (4). The inferior
vena cava is located in the
sulcus of the vena cava, a vertical depression located in the middle part of the bare area of the
liver (Figure 1 with legend (1)) (9, 10).
These hepatic veins Rouviere divides into major hepatic veins and minor hepatic veins, while Latarjet
also divides it into two groups, but an upper group and an lower group. However, the minor hepatic veins
that Rouviére mentions are the hepatic veins of the lower group that Latarjet mentions. These veins are
variable in number, but range from approximately 20 to the inferior vena cava and drain blood from the
caudate lobe (9, 10). Likewise, as its name suggests, the
group of hepatic veins or superior group flows
into the inferior vena cava but superior to those of the inferior group. According to Rouviere, these
veins are usually two, a right one that is larger than the left and drains blood from the right lobe of
the liver, while the left hepatic vein comes from the left, square lobe, and the caudate (10). In our
work, after dissecting the anatomical structure, the tributaries of the right and left hepatic veins
could be easily visualized, as well as the right hepatic vein itself (Figure 1, legend (7), (8) and (9
)) as mentioned by Rouviere.
The functional blood supply of the liver comes from the hepatic portal vein, which, according to
Rouviere, undergoes a bifurcation at the level of the hepatic portal vein, dividing into two branches:
right and left. The right branch, shorter and thicker than its left counterpart, forms an obtuse angle.
On the contrary, according to Latarjet, the division of this vein presents asymmetry, since the left
branch separates from the right branch creating a right angle (9, 10). In our study, we confirmed the
asymmetry in the division of the portal vein, coinciding with what is described in the literature
(Figure 2, legend (11) and (20)).
Each of the branches of the portal vein presents a special distribution in its respective anatomical
lobe, giving rise to thick and thin branches that correspond to the segments of the liver. Rouviere and
Latarjet have different names. These names and their comparison with our product will be discussed in
the next paragraph.
According to Latarjet, the right branch of the hepatic portal vein is divided into an anterior and a
posterior branch, the posterior branch is more horizontal and directed backwards, originating the
branches for segments VI and VII, while the anterior branch is directed towards above and behind,
originating the branches of segment V (3). According to Rouviere, the right
branch of the hepatic portal
vein has two divisions, a medial division near the main portal fissure and another lateral one limited
by the right portal fissure, in both divisions the anterior and posterior segments originate (10). The
anterior branch of the medial division gives the branch for segment V and the second division gives the
branches for segment VI and VII (10). In this case, the anterior and
posterior branch described by
Latarjet corresponds to the result of the medial division of the hepatic portal vein given by Rouvier.
In our work, the corresponding branches for the liver segment can be visualized (Figure 2, legend (22),
(23) and (25)).
Regarding the division of the left branch of the portal vein and its corresponding hepatic segments.
Rouviere mentions that the left branch gives rise to small branches for segment I and two main branches,
the umbilical and the thin lateral that supplies segment II, while the umbilical divides again into a
medial branch for segment IV and a lateral branch for the segment III (10).
Latarjet, for its part,
mentions that the left portal vein has two portions, a transverse portion that ends up dividing into a
lateral branch that corresponds to segment II and an umbilical portion that ends in the recess of rex
and divides into the medial branches for the segment IV and lateral for segment III (9). In our product
you can view the branches mentioned in Figure 2 with the legends (11), (13), (14), (15), (16), (17),
(18) and (19).
CONCLUSION
This project provides a valuable resource for medical student learning and sets a precedent for future
projects creating anatomical preparations. The recommendations presented at the end of the report will
serve as a guide for those who wish to replicate this procedure, improving the effectiveness of the
process and contributing to the availability of quality anatomical material for medical education.
Authorship contributions:
The authors participated in conceptualizing, researching, using methodology and resources,
and writing the original draft and final version.
Financing:
self-financed.
Declaration of conflict of interest:
The authors declare that they have no conflict of interest.
Recevied:
January 7, 2024
Approved:
April 18, 2024
Correspondence author:
Emanuel Sebastian Balarezo Rebaza
Address:
Urb. Cáceres Aramayo L´21 - Nuevo Chimbote, Perú
Phone:
+51 912 021 466
E-mail:
ebalarezor.iepelnazareno@gmail.com
Article published by the Journal of the faculty of Human Medicine of the Ricardo Palma University. It is an open access article, distributed under the terms of the Creatvie Commons license: Creative Commons Attribution 4.0 International, CC BY 4.0 (https://creativecommons.org/licenses/by/1.0/), that allows non-commercial use, distribution and reproduction in any medium, provided that the original work is duly cited. For commercial use, please contact revista.medicina@urp.edu.pe.
BIBLIOGRAPHIC REFERENCES