ORIGINAL ARTICLE
REVISTA DE LA FACULTAD DE MEDICINA HUMANA 2024 - Universidad Ricardo Palma10.25176/RFMH.v24i1.6340
ASSOCIATED FACTORS WITH JAUNDICE REQUIRING PHOTOTHERAPY: A CASE-CONTROL STUDY IN A HOSPITAL IN PERU
FACTORES ASOCIADOS A ICTERICIA CON REQUERIMIENTO DE FOTOTERAPIA: ESTUDIO DE TIPO CASOS Y CONTROLES EN UN HOSPITAL DE PERÚ
Mary Claudia Huambo Panduro
 1,a
1,a
Andrea P. Ramirez-Ortega
 1,b
1,b
Luis Roldan-Arbieto
 1,c
1,c
José M. Vela-Ruiz
 1,a,d
1,a,d
1 Instituto de Investigación en Ciencias Biomédicas de Universidad Ricardo Palma. Lima, Perú
a Medical Doctor
b Human Medicine Student
c Master in Strategic Business Administration
d Master in Health Services Management
ABSTRACT
Objective: The aim was to identify the factors linked to jaundice that necessitates phototherapy.
Material and Methods: An observational, analytical, and retrospective case-control study was
conducted. The medical records of 212 patients aged 0 to 7 days from the neonatology service at Hospital
Carlos Lanfranco La Hoz were reviewed, divided into 106 cases (with phototherapy) and 106 controls
(without phototherapy).
Results: Preterm neonates showed a significant association with an OR: 5.526; 95% CI
(2.038-14.981), P= 0.001; and ABO incompatibility had an OR: 4.373, 95% CI (1.934-9.889), P= 0.001.
Conclusions: The study concludes an association between preterm neonates, ABO incompatibility,
and the necessity for phototherapy.
Keywords: Jaundice neonatal, risk factors, phototherapy. (Source: MeSH NLM).
RESUMEN
Objetivo: Determinar los factores asociados a ictericia con requerimiento de fototerapia.
Material y Métodos: Estudio observacional, analítico, y retrospectivo de tipo casos y controles.
Se revisaron las historias clínicas de 212 pacientes de 0 a 7 días de nacidos del servicio de
neonatología del Hospital Carlos Lanfranco La Hoz, divididos en 106 casos (con fototerapia) y 106
controles (sin fototerapia).
Resultados: Se encontró una asociación significativa entre los neonatos pretérmino y la necesidad
de fototerapia, con un OR:5.526; IC 95% (2.038-14.981), P= 0.001; así como una asociación entre la
incompatibilidad ABO y la fototerapia, con un OR:4.373, IC 95% (1.934-9.889), P= 0.001.
Conclusiones: Se concluye que existe asociación entre neonatos pretérmino, la incompatibilidad
ABO con la necesidad de fototerapia.
Palabras clave: Ictericia neonatal, factores de riesgo, fototerapia. (Fuente: DeCS
BIREME).
INTRODUCTION
Jaundice is the most common clinical sign in neonates and is often the reason for readmissions and
admissions to Intermediate Care Units (IMCU) to receive phototherapy. It occurs in 50-60% of term
neonates and close to 80% of preterm infants. Of these, 20% require phototherapy to prevent
complications such as encephalopathy and Kernicterus (1).
A study in the United States on hospitalizations for jaundice and Kernicterus revealed a decrease in
Kernicterus cases and related hospitalizations. However, between 1988 and 2005, the trend of
hospitalized neonates with jaundice was still 15.6% (2). A meta-analysis
revealed that the rate of
severe neonatal jaundice is significantly higher in Africa, with 667.8 cases per 10,000 live births,
compared to Europe, which has an incidence of 3.7 per 10,000 live births (3). In Peru, the incidence of
neonatal jaundice is 39 per 1000 live births, with Lima and Callao accounting for 48% of cases, while
the regions of Cusco, Arequipa, La Libertad, and Ica have the highest incidence rates (4).
Jaundice is the seventh leading cause of neonatal mortality worldwide, with a rate of 1306.3 per 100,000
live births, highlighting the importance of timely management (5). Two types
of hyperbilirubinemia are
distinguished: physiological and pathological, and it is crucial to identify their possible causes, such
as hemolysis, infections, and obstetric complications (6). Phototherapy is
the first-line treatment for
hyperbilirubinemia. However, it is important to note that some studies mention its association with
allergic diseases after its use, such as asthma, allergic rhinitis, atopic dermatitis, and even food
allergies (1). According to a study in California, USA, 8% of 50,000
newborns received this treatment
(7).
In Peru, studies have been conducted on factors associated with neonatal jaundice. However, this
research aims to highlight the importance of neonates requiring phototherapy in intermediate care and
analyze the maternal-neonatal conditions that affect their length of stay. It also aims to identify
strategies to reduce admission to the neonatal IMCU.
Therefore, this study sought to determine the factors associated with jaundice requiring phototherapy at
Hospital Carlos Lanfranco La Hoz during the period 2021-2022.
Design and Study Area
Observational, analytical, retrospective case-control study.
Population and Sample
The study population consisted of 212 neonatal patients aged 0-7 days, with gestational ages between 35
and 41 weeks, diagnosed with jaundice. These patients were divided into two groups: 106 cases (required
phototherapy) and 106 controls (did not require phototherapy). Neonates with congenital malformations
were excluded.
Variables and Instruments
The main variable was: Jaundice requiring phototherapy. The independent variables analyzed were:
gestational age, birth weight, ABO incompatibility, Rh incompatibility, neonatal sepsis, maternal
Urinary Tract Infection (UTI), and maternal anemia.
Procedures
To collect information on neonatal jaundice, both in cases requiring phototherapy and those without, the
technique of reviewing medical records was used. These records collected data from both the neonate and
the mother, who were treated in the neonatology hospitalization service of Hospital Carlos Lanfranco La
Hoz during the period from 2021 to 2022, according to the established objectives. Subsequently, the
collected data were entered into the Microsoft Excel 2019 program, and the corresponding analyses were
performed using the IBM SPSS v29 program.
Statistical Analysis
A database was extracted from a data collection form and recorded in Microsoft Excel 2019. It was then
processed in IBM SPSS v29 for statistical analysis. Qualitative variables were described using
frequencies and percentages, while quantitative variables were evaluated for normality, and measures of
central tendency and dispersion were calculated. To identify factors associated with neonatal jaundice
requiring phototherapy, a bivariate analysis was performed using the chi-square test, considering a
significance level of p <0.05 and a confidence interval of 95%. The Odds Ratio (OR) measure of
association was also used. For the multivariate analysis, the adjusted Odds Ratio measure of association
was used, considering a significance level of p <0.05.
Ethical Aspects
The study followed current ethical standards and received approval from the Ethics Committee of the
Universidad Ricardo Palma and the Hospital Carlos Lanfranco La Hoz. The proper use of data and research
ethics were guaranteed, maintaining the integrity and confidentiality of the participants' medical
records. Since the information was obtained from the review of medical records, specific informed
consent was not used for this study.
Results
The research covered 212 medical records of neonates diagnosed with neonatal jaundice, divided into two
groups: 106 neonates requiring phototherapy (cases) and 106 neonates not needing phototherapy
(controls). The mean gestational age for the entire sample was 38.26 weeks, and the mean birth weight
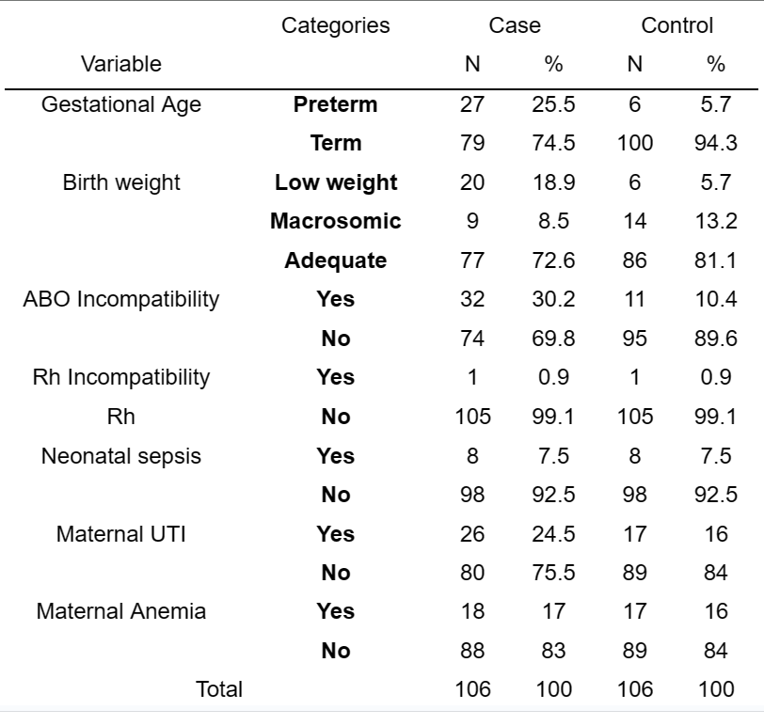
was 3213g. In the univariate analysis (see Table 1), it was observed that 25.5% of neonates in the case
group were preterm, and 74.5% were term. Regarding weight, 18.9% had low birth weight, 72.6% had
adequate weight, and 8.5% were macrosomic. It was also found that 30.2% of neonates in the case group
had ABO incompatibility, and only 0.1% with Rh incompatibility required phototherapy. 7.5% of cases had
a positive diagnosis of neonatal sepsis, while 24.5% had maternal UTI, and 17% had a history of maternal
anemia (Table 1).
Source: Own elaboration
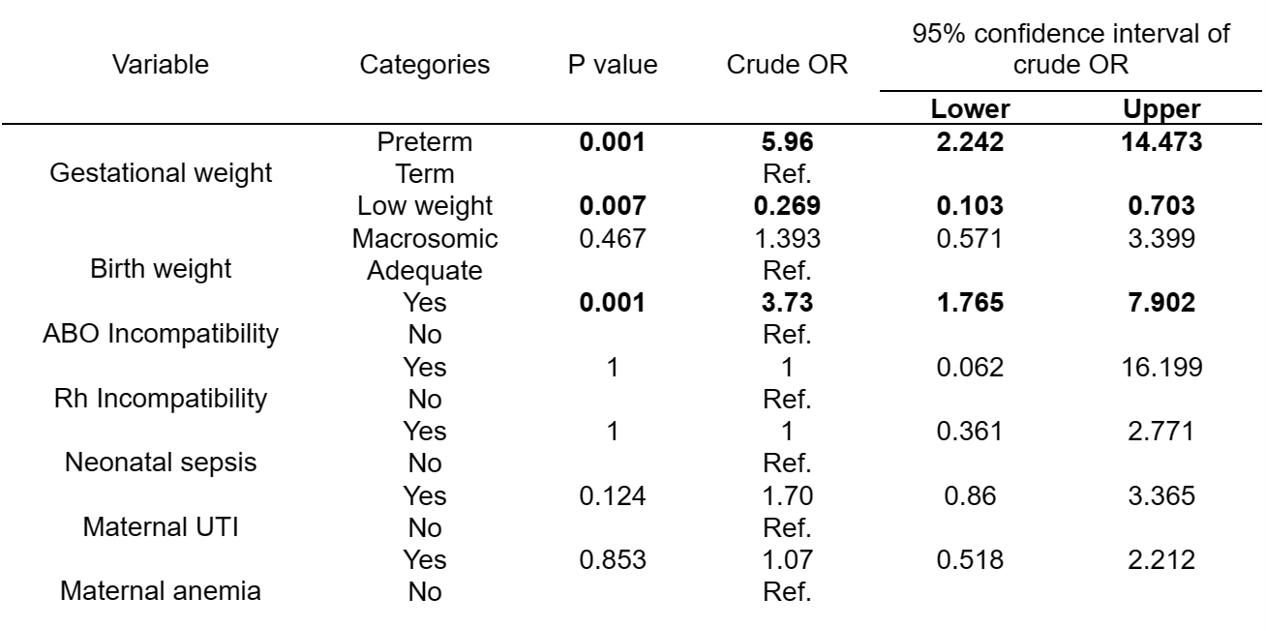
In the bivariate analysis, a significant difference was found in the risk of needing phototherapy
according to gestational age, with preterm neonates being 5.96 times more likely to require it than term
neonates. Birth weight also showed statistical significance, with low-birth-weight neonates having 73.1%
fewer chances of needing phototherapy. However, macrosomic neonates did not show a solid association.
ABO incompatibility showed a significant association, with neonates with a positive diagnosis being 3.73
times more likely to require phototherapy than those without ABO incompatibility. The other variables
analyzed did not show a statistically significant association (Table 2).
Source: Own elaboration
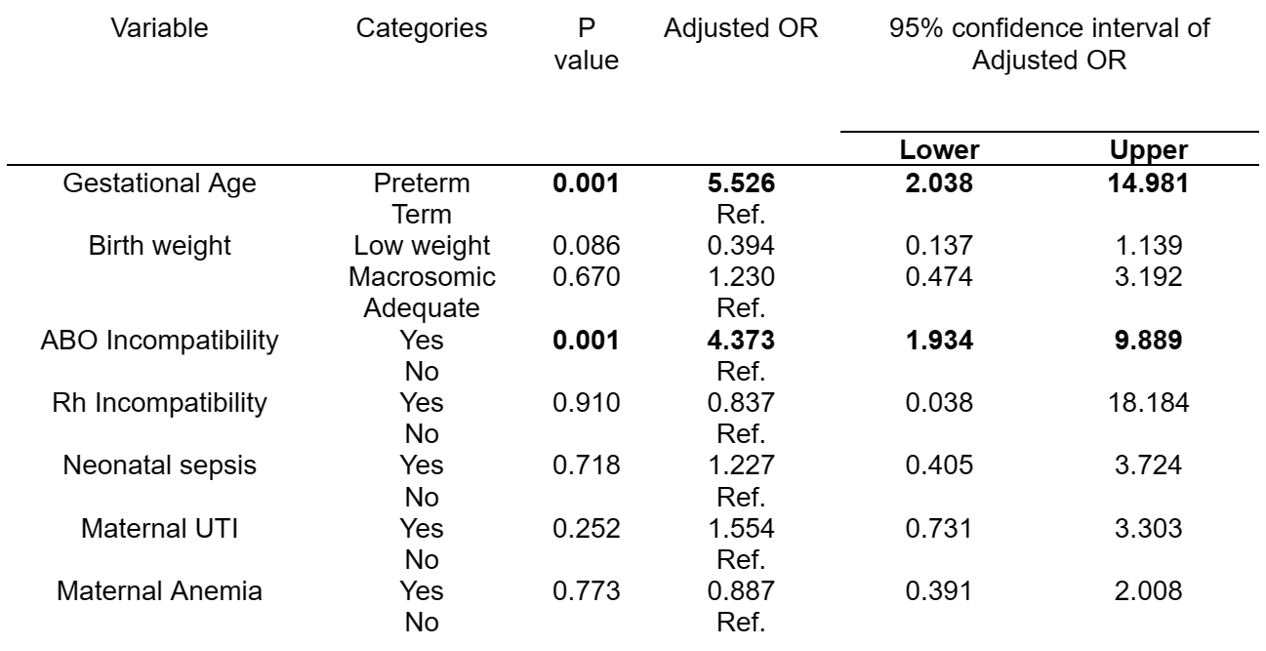
In the multivariate analysis, gestational age and the presence of ABO incompatibility continued to show
statistical significance. Preterm neonates were 5.52 times more likely to need phototherapy compared to
term neonates, and neonates with ABO incompatibility were 4.37 times more likely to require it compared
to those without the diagnosis. However, birth weight lost significance in the multivariate analysis
(refer to Table 3).
Source: Own elaboration
Discussion
Main Findings
In our study, statistically significant factors associated with neonatal jaundice requiring phototherapy
were identified, including a gestational age of less than 37 weeks and the presence of ABO
incompatibility. The lack of statistically significant results related to jaundice and Rh
incompatibility may be attributed to the low incidence of Rh incompatibility in our sample. With only 2
neonates out of 212 cases presenting Rh incompatibility, the scarcity of cases limits our ability to
detect a significant association between Rh incompatibility and jaundice in this study.
Comparison with other studies
This study analyzed a sample in which 15.5% of neonates were born prematurely (<37 weeks), and within
this group, 25.5% required phototherapy. The results revealed a statistically significant relationship
with a value of p=0.001 and an OR=5.52. These findings coincide with those of Amable O., who also found
a statistically significant association between prematurity and the need for phototherapy, with an
OR=2.98 and a value of p<0.001. Another study conducted by Meza P. supports these results,
demonstrating a significant association between prematurity and phototherapy, with an OR=2.03 and a
value of p<0.015. However, there is a study in Brazil, conducted by Dias V. et al., where it was
observed that term neonates had a greater association with the need for phototherapy. In this study,
gestational age ranged between 38 and 39 weeks (8 - 10).
This is explained because late preterm newborns (34 0/7-36 6/7 weeks of gestation) show a decrease in
UGT1A1 enzyme activity, which affects bilirubin clearance, prolonging jaundice. Additionally, they may
have difficulties in the feeding behavior and suckling reflex, which can lead to poor breastfeeding
(11).
Several previous studies have observed an association between ABO incompatibility and the requirement
for phototherapy in newborns. For instance, a strong association between both variables was found in
studies conducted by Dias V. and Avalos M., with OR=12 and OR=24 respectively. Another study in
Huancayo, a highlander city of Perú, found a statistically significant association with OR=1.21. In our
research, a significant association was also found between ABO incompatibility and the need for
phototherapy, with an OR=4.37 and a p-value of 0.001 (10, 12,
13).
We know that jaundice due to ABO incompatibility is caused by hemolysis and occurs in around 20% of
pregnancies, where the presentation is usually O-B or O-A (11, 14). These results support the idea of a
strong association between ABO incompatibility and the need for phototherapy in newborns.
Low birth weight and macrosomia are risk factors for developing neonatal jaundice. In the study, it was
found that 18.9% of newborns with low birth weight, 8.5% of macrosomic newborns, and 72.6% of newborns
with adequate weight required phototherapy. In the bivariate analysis, low birth weight was significant
and acted as a protective factor with an OR=0.269 and a p-value of 0.007. However, in the multivariate
analysis, this relationship lost statistical significance (OR=0.394; p=0.086), probably due to the
sample size of the hospital. These results are consistent with similar studies conducted by Dias V. and
Meza P., where no statistically significant association was found between birth weight and phototherapy.
In contrast, another study conducted by Amable O. showed a strong association between low birth weight
and jaundice requiring phototherapy, with a p-value of 0.001 and an OR=3.26, and a higher presentation
frequency of 41.7%.5,6,7
Low birth weight can alter the blood-brain barrier and increase the risk of Kernicterus. In the case of
macrosomic newborns, higher body weight can lead to increased bilirubin formation, as bilirubin
formation per day can range between 8-10mg per kilogram of weight, increasing the risk of
hyperbilirubinemia. (15)
Recommendations
It is recommended to investigate variables such as the history of phototherapy in siblings or parents,
but these could not be studied due to the lack of registration in medical records. Additionally, proper
breastfeeding technique is another variable of interest, but its complete evaluation was limited by the
absence of periodic assessments during hospitalization, which could introduce biases.
A prospective study is suggested to determine if neonates who received phototherapy developed allergic
diseases such as asthma, atopic dermatitis, or allergic rhinitis.
Further studies on possible rebound cases after phototherapy treatment are also recommended. Variables
such as gestational age less than 37 weeks, neonatal sepsis, early onset of phototherapy, and hemolytic
diseases should be considered, as they could be causes of hospital readmissions.
Limitations
Difficulty in finding cases that met the inclusion criteria.
Conclusions
The factors associated with the need for phototherapy were prematurity and ABO incompatibility. It is of
utmost importance to recognize the risk factors, to treat them preemptively in order to avoid
complications, and also to improve the health and quality of life of newborns. Additionally,
surveillance and guidance to mothers during the gestation period and hospitalization in rooming-in are
recommended since there are other influential factors in the development of jaundice.
Authorship contributions:
MCHP participated in conceptualization, investigation, methodology, resources, and drafting
of the original manuscript. APRO participated in investigation and drafting of the final
manuscript. LRA participated in investigation and resources of the original manuscript. JMVR
participated in conceptualization, investigation, and methodology of the original
manuscript.
Financing:
Self-funded
Declaration of conflict of interest:
The authors declare no conflict of interest.
Recevied:
January 25, 2024
Approved:
March 27, 2024
Correspondence author:
Andrea Patricia Ramirez Ortega
Address:
Av. Alfredo Benavides 5440, Santiago de Surco, Lima-Perú.
Phone:
(+51) 941455431
E-mail:
ramirezandreapatricia@gmail.com
Article published by the Journal of the faculty of Human Medicine of the Ricardo Palma University. It is an open access article, distributed under the terms of the Creatvie Commons license: Creative Commons Attribution 4.0 International, CC BY 4.0 (https://creativecommons.org/licenses/by/1.0/), that allows non-commercial use, distribution and reproduction in any medium, provided that the original work is duly cited. For commercial use, please contact revista.medicina@urp.edu.pe.
BIBLIOGRAPHIC REFERENCES