REVIEW ARTICLE
REVISTA DE LA FACULTAD DE MEDICINA HUMANA 2024 - Universidad Ricardo Palma10.25176/RFMH.v24i1.6341
HYPERGLYCEMIA AS A RISK FACTOR FOR IN-HOSPITAL MORTALITY IN MYOCARDIAL INFARCTION
HIPERGLICEMIA COMO FACTOR DE RIESGO DE MORTALIDAD HOSPITALARIA EN INFARTO DE MIOCARDIO
Ciro Barrantes-Alarcon
 1,2,a
1,2,a
Rosalia Fernández-Coronado
 1,3,b
1,3,b
Adriel Olortegui-Yzu
 1,3,c
1,3,c
1 Faculty of Human Medicine, Universidad Nacional Mayor de San Marcos, Lima, Peru
2 Cardiology Service, Hospital Nacional Guillermo Almenara Irigoyen, Social Health Insurance.
Lima, Peru
3 Instituto Nacional del Corazón, Social Health Insurance. Lima, Peru
a MD, Specialist in Cardiology. Master of Medicine
a MD, Specialist in Cardiology. Master of Medicine
b MD, Specialist in Cardiology. Doctor of Public Health
c MD, Epidemiologist
ABSTRACT
Introduction: Myocardial infarction continues with high mortality rates, from 4.6% to 13.1%.
There are predictive risk stratification models, such as the Grace Score, which does not include
glycemia as a variable. Patients hospitalized for myocardial infarction with hyperglycemia on admission
may have higher mortality, in ST elevated and non-elevated infarcts.
Objectives: The objective of this review is to identify and systematize the evidence on
hyperglycemia on admission as a biomarker of mortality and heart failure in acute myocardial infarction.
Materials and Methods: The search was carried out in the MEDLINE database including the MeSH
terms hyperglycemia and hospital mortality or heart failure in myocardial infarction, selecting 12
articles.
Results: Hospital mortality was calculated in 11 articles, in 9 of them a significant association
was found between hyperglycemia and hospital mortality, both in the bivariate and multivariate analysis,
and in 2 articles this association was not demonstrated. For in-hospital mortality, the results of 11
articles included in this review were synthesized. The frequency of occurrence of heart failure was
determined in 11 articles, finding a higher frequency in 9 of them. For in-hospital mortality, the
results of 11 articles included in this review were synthesized and analyzed, in 8 the analysis was
performed in non-diabetics, obtaining OR: 4.15, IC 95% (2.853-6.035), in 3 for diabetics obtaining OR
2.365 IC 95% (1.778- 3,146) and in 6 for the total population finding OR 3,314 (2,910-3,774).
Conclusions: Hyperglycemia on admission is associated with increased mortality and frequency of
occurrence of heart failure during hospitalization for myocardial infarction, with evidence of moderate
quality.
Keywords: hyperglycemia, hospital mortality, myocardial infarction (Source: MeSH).
RESUMEN
Introducción: El infarto de miocardio continúa con altas tasas de mortalidad, desde 4.6 % hasta
13.1 %. Existen modelos predictivos de estratificación de riesgo, como el Score Grace, que no incluye la
glicemia como variable. Los pacientes hospitalizados por infarto de miocardio con hiperglicemia al
ingreso pueden tener mayor mortalidad, en infarto ST elevado y no elevado.
Objetivo: Identificar y sistematizar la evidencia sobre hiperglicemia al ingreso como biomarcador
de mortalidad y de insuficiencia cardiaca en infarto de miocardio.
Materiales y Métodos: La búsqueda se realizó en la base de datos Medline, se incluyeron los
términos MeSH hiperglicemia y mortalidad hospitalaria o insuficiencia cardiaca en infarto de miocardio y
se seleccionaron 12 artículos.
Resultados: La mortalidad hospitalaria se calculó en 11 artículos; en 9 de ellos se encontró
asociación significativa entre hiperglicemia y mortalidad hospitalaria; en el análisis bivariado y en el
multivariado y en dos artículos, no se demostró dicha asociación. En 11, se determinó la frecuencia de
aparición de insuficiencia cardiaca y se encontró mayor frecuencia en nueve de ellos. Para mortalidad
hospitalaria, se sintetizaron y analizaron los resultados de 11 artículos incluidos en esta revisión; en
ocho, se realizó el análisis en no diabéticos y se obtuvo OR: 4,15, IC 95 % (2,853-6,035); en tres, para
diabéticos, OR 2,365 IC 95 % (1,778-3,146) y en 6, para población total, OR 3,314 (2,910-3,774).
Conclusiones: Hiperglicemia al ingreso está asociada a mayor mortalidad y frecuencia de aparición
de insuficiencia cardiaca durante la hospitalización por infarto de miocardio, con evidencia de moderada
calidad.
Palabras clave: Hiperglicemia, mortalidad hospitalaria, infarto del miocardio (Fuente:
DeCS-BIREME)
INTRODUCTION
Ischemic coronary heart disease is a prevalent condition worldwide, and acute myocardial infarction (MI)
is one of its forms with high mortality rates. Over the years, with the aging of the global population,
an increase in mortality due to ischemic diseases has been observed. According to the WHO, in 2000,
there were 2 million deaths from ischemic heart disease, which increased to 8.9 million in 2019. In
2019, 16% of deaths worldwide were attributed to ischemic heart disease (1).
In Peru, cardiovascular disease mortality has increased to constitute 33% of the top 20 causes of
mortality (2).
The mortality rate for myocardial infarction globally ranges from around 5-10%, with reports ranging
from 4.6% (3) to 13.1% (4). In Peru, studies
have been published on hospital mortality in myocardial
infarction, for both types of infarctions: ST-elevated and non-ST-elevated, with figures of 3.4%
(5),
7.3% (6), and 4.9% (7), and specifically for
ST-elevated myocardial infarction, 10.1% (8) and 8.5% (9).
These values remain high despite technological advances. Predictive risk stratification models, such as
the Grace Score (10), exist; however, new predictive scales may be
necessary to properly identify
high-risk patients and attempt to reduce these mortality rates.
Hyperglycemia upon emergency admission is a prognostic marker for mortality and morbidity in
hospitalized patients with any disease. In the case of MI, stress hyperglycemia is defined as elevated
admission glucose levels, typically above 140 mg/dL (11). However, the
definition may vary among
authors. A systematic review found hyperglycemia to be a predictor of in-hospital mortality for any
cause(12). In MI, hyperglycemia upon admission is common, and several
studies suggest that patients with
hyperglycemia upon admission may have higher mortality rates, both in ST-elevation MI (13 - 15) and
non-ST-elevation MI (16), although its value remains controversial. This
association also extends to
non-diabetic groups (16 - 18). Furthermore, this
association persists when evaluating the occurrence of
complications such as pulmonary edema and cardiogenic shock (19). However,
admission glucose levels are
not included in classic predictive models of in-hospital mortality for MI.
The objective of this review is to identify and systematize evidence regarding admission hyperglycemia
as a biomarker for mortality and heart failure in acute MI.
SEARCH METHODOLOGY
The study design is based on a literature review on hyperglycemia, hospital mortality, and heart failure
in MI.
1. Eligibility Criteria
Inclusion criteria were as follows: Studies involving patients with MI who presented with hyperglycemia
upon admission. The definition of MI used was the third (20) or fourth
(21) definition of MI that was in
effect at the time of the study. Hyperglycemia was defined at the discretion of the author. The study
types included observational studies, systematic reviews, or clinical trials that corresponded to the
PICO question. They were studies published in English or Spanish.
Exclusion criteria were based on study type: preclinical studies, case series, case reports, letters to
the editor, editorials, comments, technical notes, and narrative reviews.
2. PICO Question: Is hyperglycemia a prognostic marker for in-hospital mortality and heart failure in
MI? The population comprised hospitalized patients with MI. The exposure was hyperglycemia, and the
comparator was normoglycemic. Outcomes were in-hospital mortality or heart failure.
3. Search Strategy: The search strategy was conducted in the Medline database through PubMed using MeSH
terms related to the PICO question: Myocardial infarction, myocardial infarct, acute myocardial infarct,
hyperglycemia, high blood sugar, in-hospital mortality, in-hospital mortalities, inhospital mortalities,
inhospital mortality, acute heart failure, shock cardiogenic. Literature from 2013 to 2023 was reviewed
in English and Spanish. The search date was September 25, 2023. The search strategy is shown in
Supplementary Figure 1.
Methodological shortcuts included using only one database (PubMed/Medline), excluding manual or grey
literature searches, limiting the search to the last 10 years, including studies in English or Spanish,
and filtering the search to cohort studies, systematic reviews, or clinical trials. Study selection and
data extraction were not performed in duplicate.
After the search, articles were imported, and the reference manager Zotero was used to remove duplicate
articles.
4. Evidence Selection and Data Extraction
After an initial phase of title and abstract reading, potentially relevant articles underwent full-text
reading, and data were extracted into an Excel template, including the following data: First author,
article title, year of publication, journal, sample size, gender, age, exposure characteristics,
comparator characteristics, study design, outcome variable, independent variables, statistical analysis,
univariate results, measure of association, final outcome, and conclusion. This stage was performed by
the authors.
5. Bias Risk or Evidence Quality
Given that these were cohort studies, the Newcastle-Ottawa Scale was used to assess bias risk or
evidence quality. This evaluation was conducted by the authors. Low risk of bias (high quality) was
defined as seven to nine stars, and high risk (low quality) was defined as six or fewer stars.
6. Synthesis and Analysis
Frequencies of in-hospital mortality and heart failure from each study were compared, as well as the
odds ratio between hyperglycemia and in-hospital mortality for both bivariate and multivariate analyses
in studies reporting such data.
Subsequently, data from the studies were analyzed and synthesized, and a meta-analysis was performed
using Jamovi version 2.3.18 for the variables hyperglycemia and in-hospital mortality, using a
random-effects model to mitigate the effect of clinical and methodological heterogeneity among studies.
Studies were categorized into two groups: Hyperglycemia and normoglycemia, according to the definition
used by each author; if more than two categories were reported, such as moderate or severe
hyperglycemia, they were included as a single group. Studies were classified into three subgroups:
non-diabetics, diabetics, and the general population. The p-value (< 0.1 indicates heterogeneity
present), and I 2 were used to quantify heterogeneity (>50% indicates substantial heterogeneity).
RESULTS
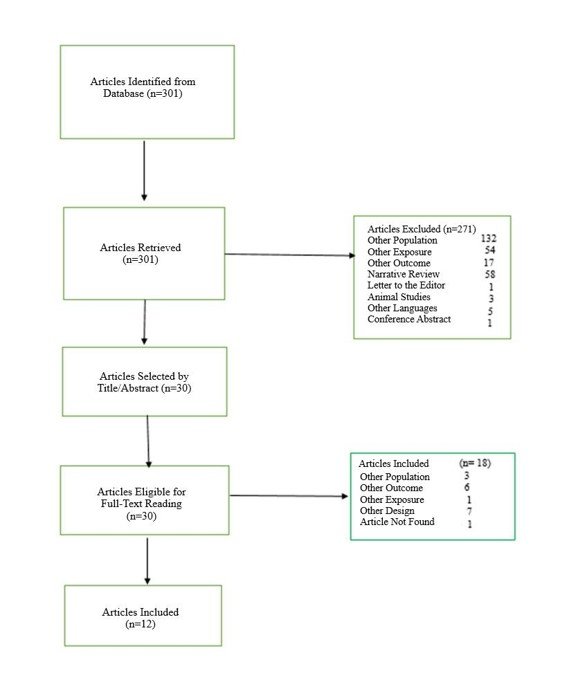
A total of 301 bibliographic citations were identified. Following screening by titles and abstracts, 271
articles were excluded, leaving 30. Full-text reading was then conducted; 18 were excluded, and 12 were
selected. The study selection flowchart is shown in Figure 1. The characteristics of the selected
studies are presented in Table 1, and the reasons for exclusion are detailed in Supplementary Table 1.
General Characteristics of Included Studies
Twelve studies were identified. According to design, six were retrospective cohorts (4, 14, 16, 22 - 24)
and six were prospective (25 - 30). The studies were
conducted between 2013 and 2022; and the origins were
Asia (6): China (4), Korea (1), Japan (1); Europe (3): Italy (1), Serbia (1), and Turkey (1); Africa
(2): Tunisia (1), Egypt (1); and USA (1). Cohort sizes varied from 275 patients (25) or 503 patients
(29) to 10,538 (4) and 12,625 patients (27), totaling 33,264 patients across the 12 studies.
Regarding pre-existing diabetes, in this review, it was found in between 15% (25) and 35% of the cohorts
(27), and it has a direct relationship with the threshold used to determine
hyperglycemia; higher
thresholds were associated with higher frequencies of diabetes. However, in two of the studies, diabetes
was not included in the subgroup analysis (23, 26).
Electrocardiogram stratifies infarctions into 2
types: ST elevated and non-ST-elevated; in six articles, the type of infarction was not considered
(4, 16, 23, 24, 27, 28), and in the other six, ST elevated infarctions
were included (14, 22,
25, 26, 29, 30). No
study evaluated non-ST-elevated infarction separately.
Regarding gender, males were the majority in all cohorts, ranging from 58% (4) to 90% (29). This
predominance was consistent across all studies, regardless of the hyperglycemia threshold used.
All patients were adults with ages whose means or medians varied according to the hyperglycemia
threshold used but were always higher in hyperglycemic than in normoglycemic individuals, with
statistically significant differences. This relationship also held in subgroup analyses of diabetics and
non-diabetics. If using glycemia >140 mg/dl: 73 years (63-81) and <140 mg/dl: 69 (58-78), p<0.001
(28); <180 mg/dl: 61.7+/-10.1; >180 mg/dl: 63.9+/-12.4; p=0.031 (22); for diabetics, glycemia <200
mg/dl or >200 mg/dl: 64.7+/-12.05 versus 66.1+/-11.2; p<0.001, in non-diabetics <200 mg/dl
63+/-13.01 versus >200 mg/dl 66+/-13.26; p<0.001 (27).
Glycemia was measured in all studies upon emergency admission; nine studies were multicenter, so the
same laboratory and methodology were not used; only three studies were single-center (16, 23, 30).
Specific Characteristics of Included Studies
In 11 studies, hospital mortality was analyzed as the primary outcome, and in 11, the presence of heart
failure during hospitalization was determined. Only one article analyzed the composite outcome of
hospital mortality, reinfarction, and revascularization of the culprit vessel (29).
In this latter case, patients were divided into three groups according to admission glycemia: <118,
118-145, and >145 mg/dl, and it was found that hospital mortality was directly related to admission
glycemia. Hospital mortality was 0%, 1.1%, and 5.3%; p=0.01, in each of the groups. The presence of
cardiogenic shock was related to the value of glycemia at admission: 0.6%, 4.1%, and 10%, respectively.
In the bivariate analysis for the composite outcome, the OR was 1.01 (1.00-1.02; p<0.01), and in the
multivariate analysis, the OR was 1.009 (1.003-1.015; p=0.01). Age, systolic blood pressure at
admission, left ventricular ejection fraction, and creatinine were used as variables in the multivariate
analysis (29).
In the remaining 11 articles, outcomes were evaluated separately: Hospital mortality and occurrence of
heart failure.
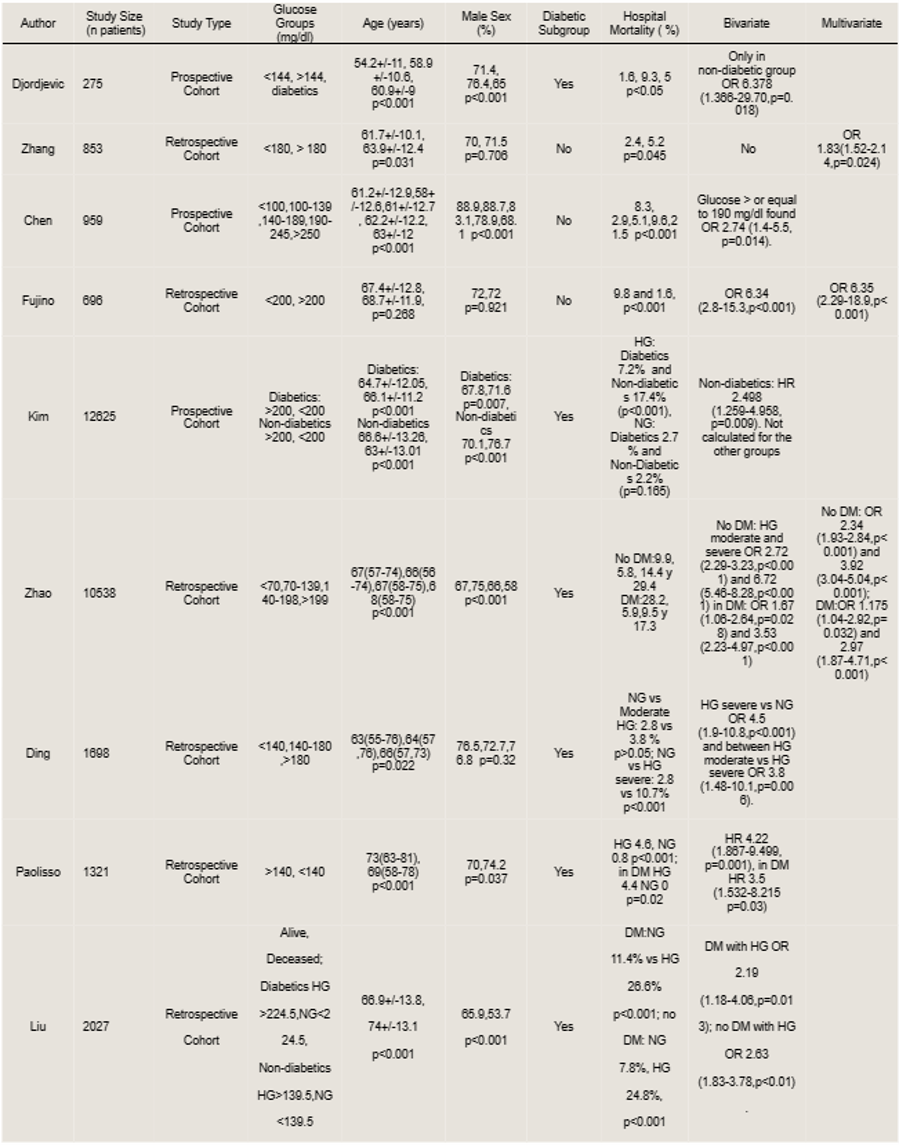
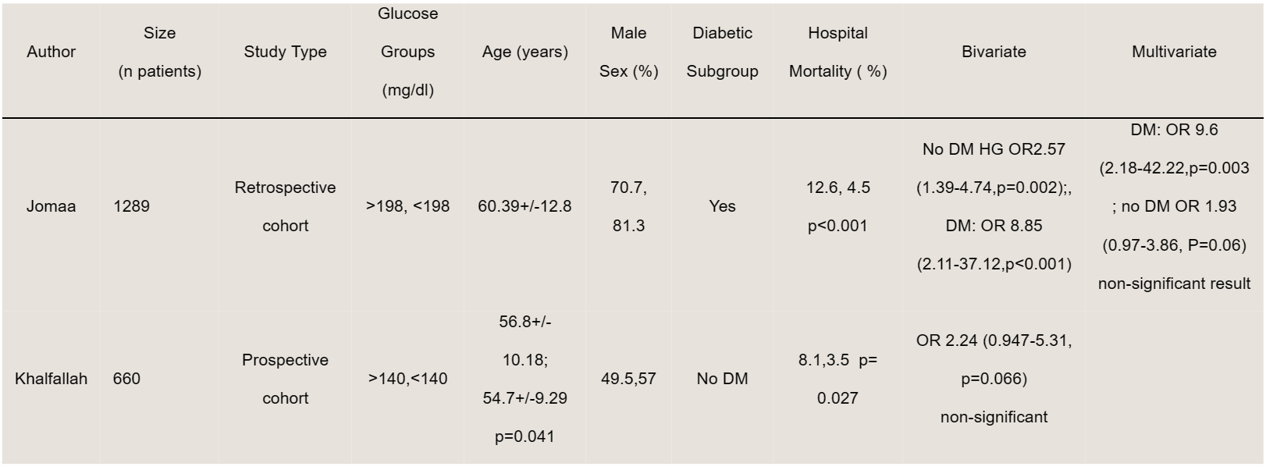
Hospital Mortality
In nine articles, a significant association was found between hyperglycemia and hospital mortality
(Table 2), and in two, no association was demonstrated (Table 3).
In the group of hyperglycemic patients, hospital mortality is higher compared to normoglycemic patients,
regardless of the threshold of hyperglycemia used, such as >140 (4, 16, 25, 26, 28 - 30), >180 (31), or
>198-200 mg/dl (14, 23, 27). Moreover,
it was found that with a higher threshold for hyperglycemia,
there is higher hospital mortality; if >140 mg/dl was used, mortality was 4.6% (28), >180 mg/dl was
found 5.2% (31), and >200 mg/dl was 9.8% (23).
For the subgroup of diabetics, this relationship also
holds, with hospital mortality of 4.4% in hyperglycemics and 0% in normoglycemics, p=0.02 (28).
The OR of hyperglycemia and hospital mortality, for the bivariate analysis, was significant in nine
studies, regardless of the threshold of hyperglycemia used, at >140 mg/dl: OR 2.72 (2.29-3.23;
p<0.001) (4), >180 mg/dl: OR 3.873 (1.485-10.10; p=0.006) (16), or >190 mg/dl: OR 2.74 (1.4-5.5;
p=0.004) (26). It also holds for the subgroup of diabetics: OR 2.19
(1.18-4.06; p=0.013) (24) and in
non-diabetics: OR 2.63 (1.83-3.78; p<0.01) (24) or 6.37 (1.366-29.70,
p=0.018) (25).
The same behavior was found in the multivariate analysis. One study found a significant association
between hyperglycemia and hospital mortality OR 6.95 (2.29-18.9; p<0.001); the other variables used
were: Age, gender, smoking, previous infarction, Killip class at admission, STEMI, primary PCI,
reperfusion time (23). In the subgroup analysis, another study demonstrated
an association in
non-diabetics with moderate hyperglycemia (140-198 mg/dl) or severe (>199 mg/dl); OR 2.34 (1.93-2.84;
p<0.001) and 3.92 (3.04-5.04; p<0.001), respectively, and in diabetics with moderate or severe
hyperglycemia: OR 1.175 (1.04-2.92; p=0.032) or 2.97 (1.87-4.71; p<0.001), respectively (4).
On the other hand, in two studies, a significant association could not be obtained; both included
non-diabetics and ST elevation. In one of them, the results were not significant in the bivariate
analysis for non-diabetics and ST elevation; OR 2.24 (0.947-5; p=0.066) was obtained (30). The other
study found no association in the multivariate analysis, for the group of non-diabetics: OR 1.93
(0.97-3.86; p=0.06). In this case, the other variables used were: Age, anemia, heart rate at admission,
and creatinine (14).
HG: Hyperglycemic
NG: Normoglycemic
DM: Diabetics
No DM: Non-diabetics
HG: hyperglycemic
NG: normoglycemic
DM: diabetics
No DM: non-diabetics
Heart failure
Hyperglycemia upon admission is also related to the presence of heart failure in patients hospitalized
for myocardial infarction. Eleven articles that calculated it were found; in nine, the frequency was
higher (Table 4).
Heart failure is a complication of myocardial infarction; there is a clinical classification method
called Killip, ranging from II to IV (cardiogenic shock); the latter being the most severe. The
occurrence of heart failure is variable and appears more frequently in the hyperglycemic group than in
the normoglycemic group. In one study, hyperglycemic patients had heart failure in 35% versus 14% in
normoglycemic patients, p <0.001 (23); in another 15.1% versus 9.1%;
p=0.02 (31). Similarly, in the
case of cardiogenic shock, another study found, according to the glycemic interval of 70-139 mg/dl: 2%,
140-198 mg/dl: 6%, and >198 mg/dl: 11%, p <0.001 (4).
Only in two studies, there was no statistical difference between the hyperglycemia and normoglycemia
groups regarding the presence of heart failure (25, 30)
(Table 5).
No measures of association between hyperglycemia and heart failure were reported in any study.
HG: Hyperglycemic
NG: Normoglycemic
DM: Diabetic
No DM: Non-diabetic
HF: Heart Failure
CS: Cardiogenic Shock
Evidence Quality of Studies
It was found that seven studies had a low risk of bias (4, 14,
16, 24, 28 - 30) and 5
had a high risk of
bias (23, 25 - 27, 31) (see supplementary table 2).
Analysis and Synthesis of Studies
Out of the 12 articles included in this review, analysis and synthesis were conducted for hospital
mortality in 11 of them. Three subgroups were determined: Non-diabetics (eight articles), diabetics
(three articles), and the general population (without distinguishing between diabetics and
non-diabetics, six articles).
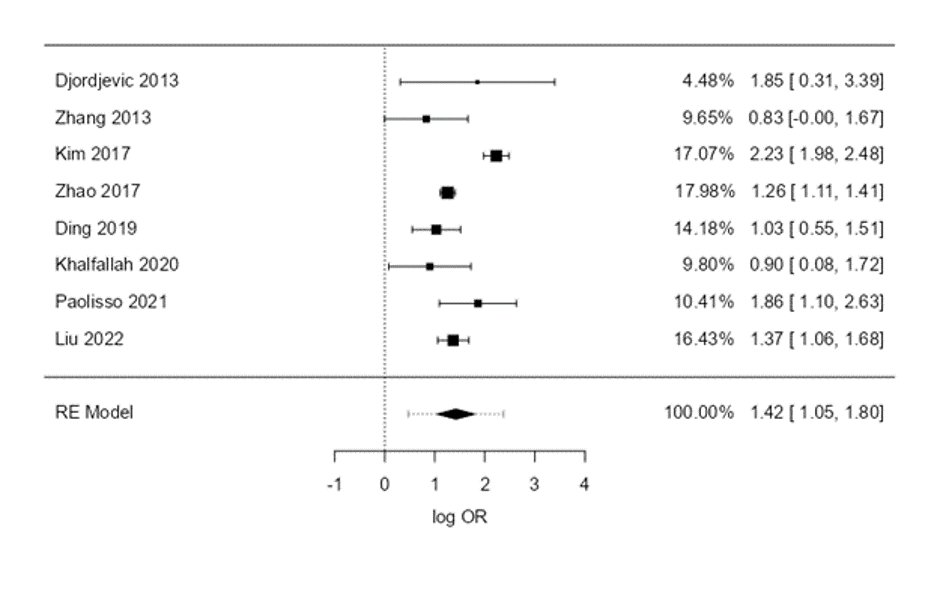
Non-Diabetic Patients
There were eight articles, with the study by Zhao et al. (4) from 2017
having the highest weight at
17.98%. When conducting meta-analysis for hyperglycemia and hospital mortality, an OR of 4.15 was
obtained with a 95% CI (2.853-6.035), and the log OR was 1.42 with a 95% CI (1.049 - 1.798) and p
<0.001. Heterogeneity was high, with p < 0.001 and I2 = 84.5% (see supplementary figure
2). The
forest plot is presented in figure 2.
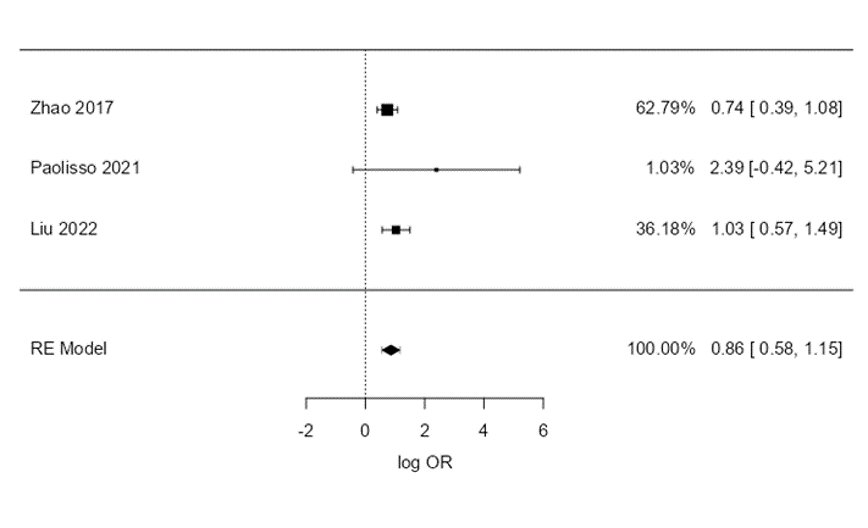
Diabetic Patients
There were three articles; again, the study by Zhao (49) had the highest weight at 62.79%. In this
group, a logOR of 0.861 was obtained with a 95% CI (0.575-1.146), p <0.001, and an OR of 2.365 with a
95% CI (1.778-3.146). Heterogeneity was low: p = 0.341 and I2 = 3.18% (see supplementary
figure 3). The
forest plot is presented in figure 3.
General Population
There were six articles. The study by Zhao accounted for 58.34% of the weight (4). The log OR was 1.20
with a 95% CI (1.068-1.328) and p <0.001, and the OR was 3.314 (2.910-3.774). Mild heterogeneity was
found, with p = 0.188 and I2 = 9.12% (see supplementary figure 4). The forest plot is presented in
figure 4.
DISCUSSION
Hyperglycemia upon admission is more frequently encountered in myocardial infarction complications such
as mortality or heart failure. Observational studies in the literature attempt to determine this
association. There are no recent systematic reviews or meta-analyses determining this association. Two
meta-analyses found a significant association, but they used different outcomes: 30-day mortality
(15)
or the composite of in-hospital mortality and mortality at 30-90 days32. A systematic review from 2000
determined the relationship between hyperglycemia and in-hospital mortality in both diabetic and
non-diabetic patients; it included studies conducted between 1985 and 1993 (33)
The phenomena occurring during hyperglycemia are varied. Stress induces a hyperadrenergic state, leading
to catecholamine release, induction of glycogenolysis, increased free fatty acids, insulin resistance,
nitric oxide inactivation, and increased reactive oxygen species production, resulting in oxidative
stress. Additionally, there is increased thrombin formation, platelet activation (34, 35), and reduced
coronary flow by interfering with nitric oxide-mediated vasodilation (36, 37).
The quality of evidence in our review was moderate, with 58% of articles rated as good quality according
to the Newcastle Ottawa Quality Assessment Scale. Singh reported 82% and Cheng reported 96% of articles
as good quality. Compared to other reviews, the issues in ours included lack of comparability with other
factors and problems with outcomes such as self-reporting or loss to follow-up (supplementary table 2).
Although admission hyperglycemia has a poor prognosis, it is not included in risk scores for myocardial
infarction. The GRACE score is widely used for mortality risk stratification in myocardial infarction;
it could be improved by including an easily obtainable variable like admission glycemia. Some studies
seek to evaluate the effect of glycemia on the GRACE score. Some small studies found no benefits
(34, 35). Timóteo et al. developed a new model that added
glycemia to the GRACE score and better classified
low-risk patients as truly low-risk and high-risk patients similarly to the GRACE score, although the
improvement was small. This could prevent unnecessary interventions that would increase costs and the
risk of procedure-related adverse events (38).
In our review, age in all cohorts was higher in the hyperglycemic group compared to the normoglycemic
group, except in the study by Fujino. This cohort had some particularities; it used higher thresholds
for hyperglycemia (> 200 mg/dl), and the number of diabetics was higher than in other cohorts (69% in
hyperglycemic versus 24% in normoglycemic) (23).
Diabetes, being a condition with a worse prognosis, should be analyzed separately. In this review, only
three studies analyzed diabetic patients separately and found a significant odds ratio, albeit lower
than in the non-diabetic group. The effect of hyperglycemia in diabetics is attenuated by various
factors; it may be that they are receiving prior insulin, which prevents hyperglycemia-induced damage,
or that chronic exposure to hyperglycemia produces antioxidant defenses that protect tissue from
oxidative stress induced by hyperglycemia (39).
The threshold used for hyperglycemia may depend on the cohort's place of origin and be a source of
different outcomes. Cohorts from Europe usually use 140-170 mg/dl, while those from Asia or Eastern
Europe prefer >200 mg/dl. Cheng et al. (32), in their review, found a
greater effect of hyperglycemia on
mortality in cohorts from Asia (RR 3.04: 2.61-3.55) and Europe (RR 3.55: 2.6-4.85), and a lesser effect
in those from Africa (RR 2.24: 1.04-4.83) and North America (OR 1.85: 1.59-2.16). In our review, in the
non-diabetic group, a stronger association was found in cohorts from Eastern Europe (25) (OR 6.3:
1.36-29.7) and Asia (OR 6.72: 5.46-8.28; p<0.001) (4) than in those from
North America (OR 2.63:
1.83-3.7; p<0.01) (24).
The value of hyperglycemia as a prognostic factor for hospital mortality is better demonstrated in the
subgroup of ST-elevation myocardial infarctions. Our rapid review and that of Singh included only
ST-elevation cases; on the other hand, Cheng only included one article with non-ST-elevation cases. The
reason may be that ST-elevation myocardial infarctions, having a greater extent of necrosis, represent a
more severe disease and therefore raise blood glucose levels more and have a greater effect on
mortality. Cheng et al., in their review, found that the association between hyperglycemia and mortality
is strengthened when divided by subgroups, geographical regions, and types of infarctions, being greater
in ST-elevation myocardial infarctions, followed by non-ST-elevation ones, and finally the group
composed of both types of infarction (32). In our review, most studies were
in non-diabetic ST-elevation
myocardial infarction cases; that is, they used a lower threshold for hyperglycemia. If only diabetic
cases were studied, they would predominantly be non-ST-elevation cases, and it may be the case that no
effect is found because lower thresholds for hyperglycemia would be used. In our rapid review, only in
the study by Liu et al., were different thresholds used for diabetic and non-diabetic cases (24).
Regarding short and medium-term mortality, Cheng et al. found that hyperglycemia at admission was
associated with mortality to a greater extent at 30-90 days (RR 2.66: 2.10-3.36) than in-hospital
mortality (RR 2.43: 2.18-2.72) with moderate-quality evidence (32).
Mortality found by Cheng et al. (32)
in the overall population was 2.12 times higher, 1.3 times higher in the diabetic subgroup, and 1.12
times higher in the non-diabetic subgroup; unlike Singh 15 and Capes 33, who found 3.3, 0.71, and 2.93
times, respectively. In our review, we found 2.31, 1.365, and 3.15 times, respectively. The association
for the overall population was weaker in Cheng's review and ours; the reason could be that in more
recent studies, modern treatments are more effective, and the impact of hyperglycemia would be
attenuated. On the other hand, the cohorts of Singh and Capes were fundamentally from the West (USA,
Western Europe), while those of Cheng and ours mostly came from the East: Asia, Eastern Europe, another
reason for finding different results.
Another point to consider is the timing of blood sampling, fasting or at admission. Some studies have
found that fasting blood glucose has better prognostic accuracy (40). On
the other hand, blood glucose,
when taken fasting, is usually on the second day, after performing angioplasty. In older reviews, such
as those by Capes and Singh, both revascularization methods, lysis, and angioplasty, were used, while in
Cheng's and ours, predominantly angioplasty was used, which is more effective than lysis. This could be
another reason for finding a weaker association in these latter studies.
The difference between our review and the others is that ours had more specific criteria; they were
cohorts that analyzed admission blood glucose and in-hospital mortality. The other reviews grouped
admission and fasting blood glucose, on the second day, and also took into account composite mortality
or 30-90 days.
Limitations
Not all studies had the same definition of admission hyperglycemia.
In this rapid review, only studies from the Medline database were included, reducing the possibility of
literature from our region. The populations were predominantly Asian.
An analysis and synthesis of observational study data were performed, which do not have the same level
of evidence as meta-analyses; however, their effect may have a similar direction.
Glycosylated hemoglobin determination was not routinely performed, which would allow for determining
whether we are dealing with a stress hyperglycemia phenomenon or an unrecognized diabetes, a situation
that can lead to confusion.
Conclusions
The magnitude of the association between hyperglycemia and hospital mortality depends on the threshold
used to define hyperglycemia, being greater if the threshold is higher, with moderate-quality evidence.
Admission hyperglycemia is more frequently encountered in myocardial infarctions that presented heart
failure during hospitalization.
Most studies demonstrated the association between hyperglycemia and hospital mortality in ST-elevation
myocardial infarctions; there is little information for non-ST-elevation myocardial infarctions.
The value of hyperglycemia as a prognostic factor for hospital mortality is better demonstrated for the
subgroup of non-diabetics, with moderate-quality evidence.
Authorship contributions:
CBA, RFC, and AOY participated in conceptualization, research, methodology, resources, and
drafting of the original manuscript.
Financing:
Self-funded
Declaration of conflict of interest:
The authors declare no conflicts of interest.
Recevied:
January 25, 2024
Approved:
March 31, 2024
Correspondence author:
Ciro Barrantes Alarcon
Address:
Calle Reynolds 111 San Borja.
Phone:
941392086
E-mail:
cirobarrantes@yahoo.com
Article published by the Journal of the faculty of Human Medicine of the Ricardo Palma University. It is an open access article, distributed under the terms of the Creatvie Commons license: Creative Commons Attribution 4.0 International, CC BY 4.0 (https://creativecommons.org/licenses/by/1.0/), that allows non-commercial use, distribution and reproduction in any medium, provided that the original work is duly cited. For commercial use, please contact revista.medicina@urp.edu.pe.
BIBLIOGRAPHIC REFERENCES
display_static_image=no&:display_spinner=no&:display_overlay=yes&:display_count=yes&:language=es-ES&:loadOrderID=0