CLINIC CASE
REVISTA DE LA FACULTAD DE MEDICINA HUMANA 2024 - Universidad Ricardo Palma10.25176/RFMH.v24i3.6434
NEAR-FATAL ASTHMA: REPORT OF AN EMERGENCY CASE FROM THE SANTA ROSA HOSPITAL
ASMA CASI FATAL: REPORTE DE UN CASO EN EMERGENCIA DEL HOSPITAL SANTA ROSA
Williams Trinidad-Rodríguez
 1,a*
1,a*
José Manuel Carlos Segura-González
 1,b
1,b
Ariadna Rodríguez-Reyes
 1,a
1,a
Daniela Vidal-Santiago
 1,a
1,a
1 Instituto Mexicano del Seguro Social. Centro Médico Nacional Manuel Ávila Camacho. Puebla,
México.
a Physician, General Surgery Resident.
b Physician assigned to the digestive surgery department.
ABSTRACT
Introduction: Diverticula are intestinal saccular dilations; They can be classified as false or
true, congenital or acquired. Complications can be serious, bleeding is the most characteristic sign.
Case report: Female, 68 years old, the condition began with upper digestive bleeding, endoscopic
studies did not show any bleeding site; intestinal transit reported 2 duodenal diverticula. Due to
multiple transfusions and hospitalizations, surgery was scheduled. Two duodenal diverticula and multiple
diverticula were found in the jejunum. Duodenal diverticulectomies and segmental resection of the
jejunum with entero-entero anastomosis were performed. During the post-surgery period she presented
intestinal fistula, which was resolved with mixed nutrition.
Discussion: Intestinal transit revealed diverticula as a probable cause of bleeding. Since there
were no minimally invasive options as determined by the guidelines, less morbid surgical treatment was
provided.
Conclusions: In the absence of endoscopic or endovascular options, surgical intervention is a
viable option; however, each case must be individualized to offer the lowest morbidity and mortality
rate.
Keywords: Duodenal-jejunal diverticula, upper gastrointestinal bleeding. Diverticulectomy.
(source: MeSH NLM)
RESUMEN
Introducción: Los divertículos son dilataciones saculares intestinales; pueden clasificarse en
falsos o verdaderos, congénitos o adquiridos. Las complicaciones pueden ser graves, el sangrado es el
signo más característico.
Reporte de caso: Femenino 68 años, inició padecimiento con sangrado digestivo alto, estudios
endoscópicos no evidenciaron sitio de sangrado; tránsito intestinal reportó 2 divertículos duodenales.
Debido a múltiples transfusiones y hospitalizaciones se programó cirugía. Se encontraron 2 divertículos
duodenales y múltiples en yeyuno. Se realizó diverticulectomías duodenales y resección segmentaria de
yeyuno con entero-entero anastomosis. Durante posquirúrgico presentó fistula intestinal, se resolvió con
nutrición mixta.
Discusión: El tránsito intestinal evidenció divertículos como probable causa de sangrado. Al no
contar con opciones de mínima invasión como determinan las guías, se otorgó tratamiento quirúrgico menos
mórbido.
Conclusiones: En caso de falta de opciones endoscópicas o endovasculares, la intervención
quirúrgica es una opción viable, sin embargo, se debe individualizar cada caso para ofrecer la menor
tasa de morbimortalidad.
Palabras clave: Divertículos duodeno-yeyunales, hemorragia digestiva alta. Diverticulectomía.
(fuente: DeCS-BIREME)
INTRODUCTION
Diverticula are saccular dilations that can cover the entire intestinal layers (true diverticula) or
partially (pseudodiverticula). The duodenum is the second most common site of formation after the colon.
The incidence is estimated at 22%, generally near the toilet ampulla (1) and
they are commonly located in the second duodenal portion in 62%, third portion 30% and fourth portion
8%. The radiological incidence is 1 - 5% and the incidence by autopsy is 11 - 22%. It is generally
discovered after the age of 40, there is no predominant gender (2).
They can be classified as congenital or acquired. Congenital duodenal diverticula are a failure of
recanalization of the duodenum during embryogenesis, leaving a diaphragm that invaginates from the
duodenal lumen, and are a rare incidental finding. There is a theory where the pons or saccular network
can elongate over time due to the mechanical traction exerted by peristalsis and thus form a
diverticulum (3).
In most cases the discovery of these entities is incidental in upper gastrointestinal contrast studies
or autopsy. Studies with Barium show that up to 5% of patients will have a duodenal diverticulum. When
the endoscopic era began, an increase in the frequency of duodenal diverticula was observed by up to 20%
(4).
More than 90% of duodenal diverticula are asymptomatic, a low percentage will develop symptoms which
will require surgical intervention. They rarely cause symptoms; abdominal pain, bloating, nausea,
vomiting, and fever may occur. Related complications are rare and may include hemorrhage,
biliopancreatic manifestations, intestinal obstruction or perforation (1, 4).
Complications of duodenal diverticula can be serious: outpouching (possible cause of bleeding),
obstruction, infection, perforation and duodenal fistulas. Bleeding is the most characteristic sign,
with perforation being the least common, with less than 20 cases reported (2, 4).
Obstruction is rare and it is less common for the Ampulla of Vater to become obstructed. Due to its
location in the periampullary region, recurrent pancreatitis, cholangitis, and choledocholithiasis can
also develop, even after cholecystectomy. Patients who experienced a cholecystectomy and also have
duodenal diverticula may present with stenosis of the Ampulla of Vater, which may develop excessive
growth of bacteria causing bilirubinate stones in the common duct(1, 4).
The initial evaluation should be carried out endoscopically, and in case of bleeding, a hemostatic stent
is injected, coagulated or placed. If it is not controlled, a bleeding diverticulum should be suspected
and invasive studies such as arteriography, angiotomography or scintigraphy with erythrocytes should be
performed. radiolabeled with technetium to locate the bleeding site, followed by endovascular therapy,
with the placement of coils or foam to coagulate the affected region (3, 4). The last resort should be surgical exploration; It is approached using
the Kocher maneuver. If the bleeding site is identified, the pancreatic duodenal artery must be sutured
directly and the duodenal pancreatic artery must be ligated and the ligation of the bleeding vessel
within the duodenal diverticulum must be completed directly. Since cephalic pancreaticoduodenectomy is
an extreme measure to resolve significant hemorrhage, there is very little literature that describes
this procedure for the condition (1, 4). Perforation is one
of the most feared and least common complications; traumatic perforations or abscess require surgical
exploration (3, 4).
Surgical intervention is the mainstay for complicated duodenal diverticulum; various authors propose
excision of the diverticulum and repair of the defect in plane. If this failure occurs, duodenal
exclusion must be completed with a reconstruction with “Roux Y” taking the bile duct to the end of the
jejunal loop and the distal pylorus towards the same branch. One of the potential complications will be
pancreatic fistula (1).
Case report:
Female 68 years old. Allergies: denied. Chronic degenerative: Type 2 diabetes, 8 years of evolution, in
adequate control. Subclinical hypothyroidism treated with levothyroxine 25mcg daily, adequate control.
Surgical history: Salpingo-oophorectomy 45 years ago, right inguinal plasty 15 years ago, left inguinal
plasty 10 years ago. Oncology: Questioned and denied. December 2021: The condition began with
hematemesis on one occasion, melena for two days, associated with colicky pain 3/10 in the mesogastrium
with irradiation to the hypogastrium. Partial analgesia to the ingestion of anti-inflammatories,
exacerbated by fasting. He denied temperature increases, acholia, choluria, tenesmus and hematochezia.
Weight loss 9kg in 3 months. A protocol was initiated due to upper digestive bleeding, the following
studies were performed:
Endoscopy January 3, 2022: Chronic gastropathy in the body, erosive in the antrum. No active bleeding.
Colonoscopy January 5, 2022: Ulcerated scar in descending colon, hemorrhoidal disease.
Histopathological report January 6, 2022: Biopsy of ileum and colon, mild edema of the lamina propria
with mild and nonspecific inflammation.
Enterotomography January 6, 2022: No alterations in the loops by this means of study.
Capsule endoscopy January 25, 2022: Erosive gastropathy in antrum, polyp in duodenum.
Abdominal scan February 17, 2022: No molecular evidence suggesting ectopic gastric tissue.
Intestinal transit February 17, 2022: Two giant diverticula in the 3rd and 4th portion of the duodenum
(Figure 1).

Figure 1: Intestinal transit showing duodenal diverticula.
No bleeding site was found in the endoscopies, endovascular therapy was not available, nor extension
studies for the exact localization of bleeding such as arteriography, angiotomography or scintigraphy
with technetium-labeled erythrocytes; The patient required transfusion of 3 - 5 erythrocyte concentrates
in different hospitalizations, for which reason a surgical schedule was decided, with high suspicion of
hemorrhagic diverticula observed in intestinal transit.
Two months prior to the surgical event, nutritional therapy was initiated by the parenteral and enteral
nutritional support service (SANPyE) based on a polymeric diet.
On June 2, 2022, the surgical procedure was performed, finding the following findings: 2 diverticula in
the 3rd and 4th duodenal portion (Figure 2), 12 jejunal diverticula in the mesenteric border from 40cm
from the Treitz angle (Figure 3).
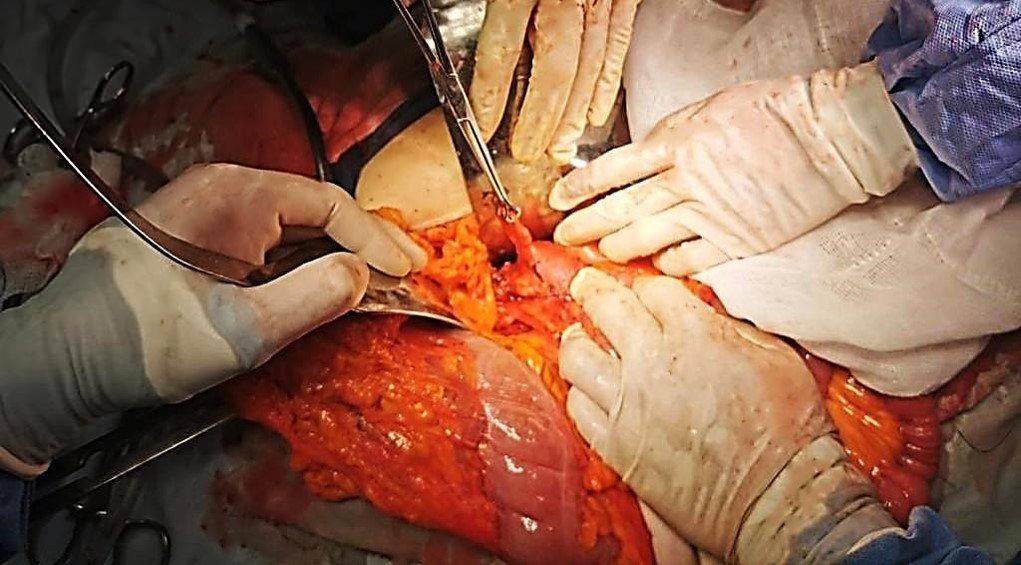
Figure 2: Duodenal diverticulum.

Figure 3: Multiple jejunal diverticula at the mesenteric border.
Intestinal resection of 60 cm was performed from 40 cm of Treitz Angle, entero-entero isoperistaltic
mechanical jejunal anastomosis, with 75 mm linear staplers; Mechanical duodenal diverticulectomies are
performed with 55 mm linear staplers (Figure 4). He bled 700cc, which was calculated as allowable; an
erythrocyte concentrate was transfused. Two saratogas drains were placed, one directed to the 3rd
duodenal portion and the other to the anastomosis site. The procedure was terminated without accidents
or incidents.

Figure 4: Mechanical diverticuloectomy.
The immediate post-surgery was completed adequately and fasting for 5 days was indicated. A series of
esophagogastroduodenal images were performed 5 days after surgery, no contrast leaks were observed, and
a polymeric diet was started. On June 10, 2022, on the 8th post-surgical day, he presented intestinal
output due to drainage, less than 100 cc per day. It was managed as a low-output intestinal fistula;
conservative treatment was given with parenteral and oral nutrition for 10 days and subcutaneous
administration of octreotide 100 mcg every 8 hours for 5 days. Thirteen days after surgery, discharge
was decided as there was no systemic inflammatory response, no elevation of inflammatory markers and low
drainage output. During outpatient follow-up, she was reported to be asymptomatic, with no signs of
digestive bleeding, oral tolerance, regular bowel movements, fistula without output. Histopathological
report of surgical specimen (Figure 5): Uncomplicated diverticular disease of the small intestine, with
congested subserosal blood vessels (Figure 6).

Figure 5: Jejunal diverticula. Pathological piece obtained from surgical resection.
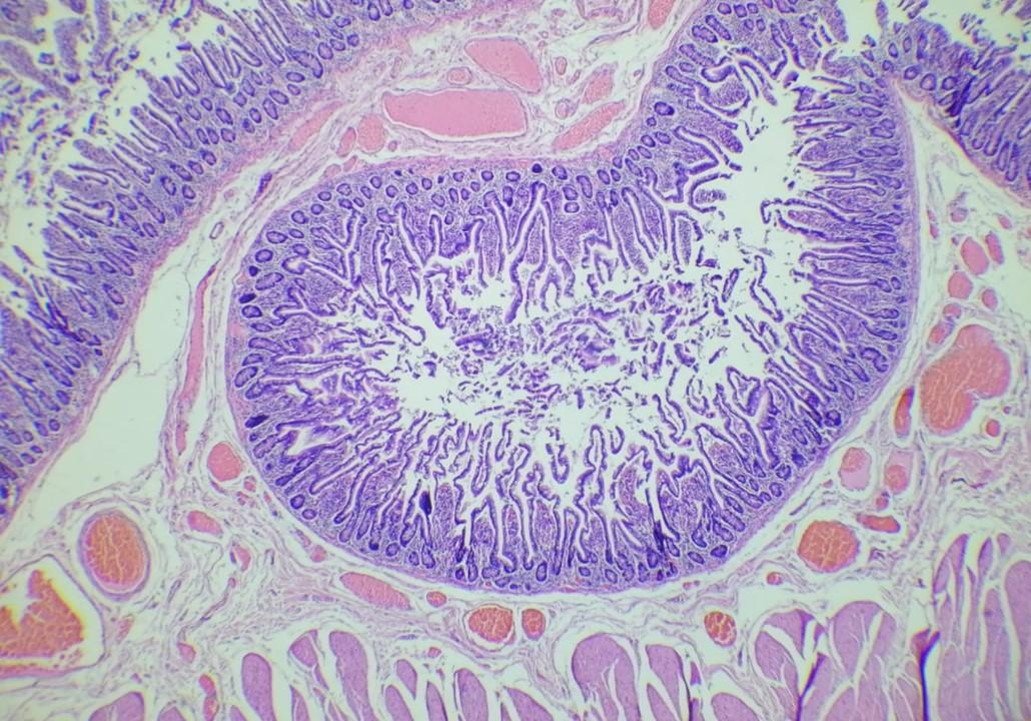
Figure 6: Histopathological view of intestinal diverticula.
DISCUSSION
Diverticula commonly arise from the second portion of the duodenum, within 2 cm of the Ampulla of Vater
due to weakness of the wall (1). In our case, we located the diverticula in
the 3rd and 4th portion of the duodenum, an unusual location. These predominated at the mesenteric
border, the site where blood vessels enter and become intraparietal, supporting the theory that they
originated from sites of weakness in the intestinal wall.
In most cases, the patient is asymptomatic in 90% and may present various complications (stasis and
biliopancreatic obstruction), bleeding, diverticulitis, and perforation(1),
the main symptom reported by our patient was data of upper digestive bleeding, which led him to require
multiple transfusions. They are usually diagnosed incidentally during autopsies or endoscopies, however,
with our patient the capsule endoscopy did not make the diagnosis; the diverticula were evidenced by
intestinal transit, making it a good diagnostic option when suspicion is high and studies are negative.
When there is a retroperitoneal perforation, it is usually contained and does not present signs of
peritoneal irritation; abdominal pain, nausea, vomiting, cholestasis and pancreatitis usually
occur(5, 6, 7). The patient's clinical
presentation should guide the method and management on an individualized basis. Surgical management is
challenging; if found in the 2nd portion of the duodenum, it is recommended to identify papilla
intraoperatively endoscopically by inserting a catheter (8, 9). In our case report, there was no perforation or diverticulitis; it
debuted as a condition of upper digestive bleeding. During the study protocol, diverticula were evident
as a probable cause of bleeding. The patient had multiple hospitalizations for anemia, reflected in
asthenia, adynamia and melena.
Surgical treatment has a high morbidity and mortality rate, so it should be chosen only in indicated
cases due to post-surgical complications. The most common intervention to resolve this pathology is
diverticulectomy with closure in two planes. There are interventions for more complex cases such as:
pyloric exclusion, gastroduodenostomy or gastrojejunostomy, duodenostomy and cephalic
duodenopancreatectomy(10, 11). We decided to perform
mechanical duodenal diverticulectomy due to the size of the diverticula; Intestinal resection was
reserved for the segment in the jejunum with multiple small diverticula. Later, during the same surgical
event, reconstruction with side-to-side mechanical anastomosis was performed; considering this as a
high-risk anastomosis due to the tension it could present, and the high flow in this segment secondary
to gastric and pancreatobiliary secretions; however, despite the nutritional prehabilitation, during the
post-surgical period we had one of the most expected complications, intestinal fistula, which was
resolved with mixed nutrition, oral and parenteral, managed by SANPyE.
CONCLUSION
In the absence of endoscopic or endovascular options, surgical intervention is a viable option. We must
individualize each case to offer the best medical or surgical management with the lowest morbidity and
mortality rate.
THANKS:
To Dr. María Esther Ramírez Hurtado, the Doctor assigned to the Parenteral and Enteral Nutrition Support
Service (SANPyE), for the management of our patient during the pre- and post-surgical period.
Authorship contributions:
José Manuel Carlos Segura González physician assigned to the digestive surgery service, and
general surgery residents Williams Trinidad Rodríguez of 3rd year, Ariadna Rodríguez Reyes
of 4th year and Daniela Vidal Santiago of 2nd year at the C.M.N. Manuel Ávila Camacho IMSS
U. M. A. E. Puebla, Mexico; we have participated in the conception and design of the case
report, as well as the performance of the surgical procedure, the collection of images, its
writing and approval of the final version.
Financing:
Self-funded
Declaration of conflict of interest:
The authors declare that they have no conflict of interest.
Recevied:
March 15, 2024
Approved:
May 29, 2024
Correspondence author:
Williams Trinidad Rodríguez.
Address:
Calle 2 norte, Núm. 2004 CP. 72000 Col. Centro. Puebla, Puebla; México.
Phone:
(+52) 9373693696
E-mail:
Williamstrinidad.med@outlook.com
Article published by the Journal of the faculty of Human Medicine of the Ricardo Palma University. It is an open access article, distributed under the terms of the Creatvie Commons license: Creative Commons Attribution 4.0 International, CC BY 4.0 (https://creativecommons.org/licenses/by/4.0/), that allows non-commercial use, distribution and reproduction in any medium, provided that the original work is duly cited. For commercial use, please contact revista.medicina@urp.edu.pe.
BIBLIOGRAPHIC REFERENCES
