CLINIC CASE
REVISTA DE LA FACULTAD DE MEDICINA HUMANA 2024 - Universidad Ricardo Palma10.25176/RFMH.v24i3.6602
NEAR-FATAL ASTHMA: REPORT OF AN EMERGENCY CASE FROM THE SANTA ROSA HOSPITAL
ASMA CASI FATAL: REPORTE DE UN CASO EN EMERGENCIA DEL HOSPITAL SANTA ROSA
William Rojas Pérez
 1,a,b
1,a,b
Jorge L. Delgado Del Aguila
 1,c
1,c
1 Santa Rosa Hospital. Lima Peru.
a Emergency Physician.
b Head of the Emergency Service.
c Resident of Emergency and Disaster Medicine.
ABSTRACT
Introduction: Asthma, classically, is defined as a chronic inflammatory disease of the airways;
characterized by a history of respiratory symptoms, such as wheezing, shortness of breath, chest
tightness, and cough, that vary over time and in intensity. Near-fatal asthma are situations in which
asthma exacerbations can lead to cardiorespiratory arrest, orotracheal intubation and mechanical
ventilation, admission to an intensive care unit (ICU); Knowing the characteristics and risk factors
that predict this situation in a patient who arrives at the emergency room is very important for early
action.
Clinical case: We present a 23-year-old patient with a history of asthma since he was 5 years old
and irregular treatment; with a stay in the ICU and on mechanical ventilation for almost fatal asthma 8
months before; the clinical signs and the arterial blood gas analysis predicted an almost fatal asthma
condition, which is why it was decided to intubate and mechanically ventilate the patient, and then
transfer to the ICU with a favorable evolution and discharge 9 days after admission.
Conclusion: Patient who already had a previous admission for almost fatal asthma and admission
to the ICU, persistence of desaturation in the face of rescue treatment for said pathology; determining
factors for deciding rapid sequence orotracheal intubation and transfer to the intensive care unit; with
remission of the admission clinical picture and prompt discharge of the patient.
Keywords: asthma, near-fatal asthma, mechanical ventilation. (source: MeSH NLM)
RESUMEN
Introducción: El asma, clásicamente, se define como una enfermedad inflamatoria crónica de las
vías respiratorias; caracterizado por la historia de síntomas respiratorios, como sibilancias,
dificultad para respirar, opresión en el pecho y tos, que varían con el tiempo y en intensidad. El asma
casi fatal son situaciones en que las exacerbaciones asmáticas pueden conducir al paro
cardiorrespiratorio, intubación orotraqueal y ventilación mecánica, ingreso en una unidad de cuidados
intensivos (UCI); conocer las características y los factores de riesgo que predicen dicha situación en
un paciente que llega a emergencia es muy importante para la actuación temprana del mismo.
Caso clínico: Presentamos un paciente de 23 años con antecedente de asma desde los 5 años y
tratamiento irregular del mismo; con estancia en UCI y en ventilación mecánica por asma casi fatal 8
meses antes; la clínica y el examen de análisis de gases arteriales predijeron un cuadro de asma casi
fatal por lo cual se decidió la intubación y ventilación mecánica del paciente, para luego pasar a UCI
con evolución favorable de mismo y alta a los 9 días del ingreso.
Conclusión: Paciente que ya tenía ingreso anterior por asma casi fatal y su ingreso a UCI,
persistencia de desaturación ante el tratamiento de rescate para dicha patología; factores determinantes
para decidir intubación orotraqueal de secuencia rápida y su pase a la unidad de cuidados intensivos;
con remisión del cuadro clínico de ingreso y el alta pronta del paciente.
Palabras clave: asma, asma casi fatal, ventilación mecánica. (fuente: DeCS-BIREME)
INTRODUCTION
Asthma is a syndrome that includes several clinical phenotypes that share similar clinical
manifestations, but probably different etiologies. Classically, it is defined as a chronic inflammatory
disease of the airways, involving different cells and mediators of inflammation, conditioned in part by
genetic factors, with bronchial hyperresponsiveness and variable airflow obstruction, totally or
partially reversible, either by drug action or spontaneously (1).
Asthma is a heterogeneous disease, generally characterized by chronic inflammation of the airways. It is
defined by a history of respiratory symptoms, such as wheezing, shortness of breath, chest tightness,
and cough, which vary over time and in intensity, along with variable expiratory airflow limitation.
Airflow limitation may later become persistent (2).
Several asthma-related risk factors for death have been identified, such as history of previous
intubation, ICU stay, multiple emergency room visits in the previous year, beta-agonist drug abuse,
respiratory tract infections, aeroallergen sensitivity, old age, respiratory tract infections, systemic
glucocorticoid dependence (3).
In Peru, up to epidemiological week 08 - 2023, 7530 episodes of bronchial obstructive syndrome/asthma
have been reported in the country. In 2022, during the same period, 5808 episodes were reported in Peru,
and the cumulative incidence rate (CIR) was 21.95 cases per 10,000 inhabitants (4).
Asthmatic exacerbation accounts for approximately 10% of emergency department visits. Life-threatening
asthma, near-fatal asthma, asthmaticus or status asmaticus are known as asthmatic exacerbations leading
to cardiorespiratory arrest, orotracheal intubation and mechanical ventilation, admission to an
intensive care unit (ICU), hypercapnia or acidosis. Of the exacerbated asthmatics who will be
hospitalized, 2.4% presented the first situation and 6.3% the second in the EAGLE study. Patients
requiring life support had an in-hospital mortality of 2.5%. The following are predictors of
life-threatening asthma: history of sudden exacerbations; previous intubation and ventilation for
asthma; previous admission to the ICU for asthma; two or more hospitalizations in the last year for
asthma; three or more visits to the emergency room for asthma in the last year; use of more than 2
salbutamol canisters in one month; recent abandonment of systemic corticosteroid treatment; poor
perception of dyspnea; low socioeconomic status; use of illicit substances: cocaine, heroin (5).
Classically, two types of exacerbations have been identified: type 1, with inflammatory predominance,
slow onset and slow response to treatment, which represents 90% of crises, and type 2, with bronchial
spasm predominance and rapid response to treatment, which represents 10% of cases (5).
In addition, seizures can be mild, moderate, severe or near-fatal.
|
|
Mild crisis |
Moderate crisis |
Severe crisis |
Life crisis |
|---|---|---|---|---|
|
Disnea |
Slight |
Moderate |
Intense |
Agonal respiration, respiratory arrest |
|
Speech |
Paragraphs |
Phrases |
Words |
Absent |
|
Respiratory frequency |
Augmented |
>20 |
>25 |
Bradypnea, apnea |
|
Heart rate |
<100 |
>100 |
>120 |
Bradycardia, cardiac arrest |
|
Blood pressure |
Normal |
Normal |
Normal |
Hypotension |
|
Use of accessory musculature |
Absent |
Present |
Very evident |
Paradoxical or absent thoracoabdominal motion |
|
Wheezing |
Present |
Present |
Present |
Auscultatory silence |
|
Level of consciousness |
Normal |
Normal |
Normal |
Diminished or coma |
|
FEV1 or PEF (reference values) |
>70% |
<70% |
<50% |
Not applicable |
|
SaO2 |
>95% |
<95% |
<90% |
<90% |
|
PaO2 mmHg |
Normal |
<80 |
<60 |
<60 |
|
PaCO2 |
Normal |
<40 |
<40 |
>45 |
Taken from the Spanish Guide for the Management of Asthma (GEMA 5.3). 2023. Pag. 97 (https://www.semg.es/index.php/consensos-guias-y-protocolos/399-gema-5-3-guia-espanola-para-el-manejo-del-asma)
|
1 |
Previous episodes of ICU admission, or mechanical intubation/ventilation. |
|
2 |
Frequent hospitalizations in the previous year. |
|
3 |
Multiple visits to the Emergency Department in the previous year. |
|
4 |
Traits (alexithymia), psychological disorders (denial attitudes) or psychiatric illnesses (depression) that hinder adherence to treatment. |
|
5 |
Cardiovascular comorbidity |
|
6 |
Abuse of short-acting β2-adrenergic agonist. |
|
7 |
Sudden onset of the crisis. |
|
8 |
Patients without regular monitoring of their disease |
Taken from the Manual of Diagnostics and Therapeutics in Pneumology. 3rd ed. Chapter 35. Page 391 (https://www.neumosur.net/files/publicaciones/ebook/35-ASMATICA-Neumologia-3_ed.pdf)
Objectively, we identify patients as life-threatening because they present with agonal respiration or
apnea, absence of speech, bradypnea or apnea, bradycardia or cardiac arrest, hypotension, paradoxical
pulse, paradoxical thoracoabdominal movement, auscultatory silence, impaired level of consciousness or
coma, pulse oximetry less than 90%, hypoxemia and hypercapnia (5).
The initial evaluation of the patient will respect the ABC of any emergency, identifying and assisting
in order of priority the difficulty to defend the airway, the assistance of ventilation and oxygenation
and circulatory support (5).
Regarding airway instrumentation in apneic patients, with impaired level of consciousness or hypercapnic
acidosis, if rapid sequence intubation is required, the use of propofol or ketamine is preferred, while
atracurium and morphine are discouraged due to histamine release, which could enhance bronchospasm
(5).
Patients requiring mechanical ventilatory support are those who present to the emergency department in
apnea, with impaired level of consciousness, hypoxemia and hypercapnia or who do not respond to initial
treatment. The goal of ventilation is to reverse hypoxemia, stabilize hemodynamics, prevent and reverse
air trapping and mechanical ventilation-induced damage.(5)
DESCRIPTION OF THE CLINICAL CASE
Male patient, 23 years old, with incomplete high school, born and coming from Lima-Peru, currently a
student; he presents asthma since he was 5 years old with irregular salbutamol inhaler treatment;
allergic rhinitis since he was 5 years old with symptomatic treatment; Asperger syndrome; as an
important antecedent, he presented severe asthmatic crisis in December 2022, hospitalized for 28 days at
the Santa Rosa Hospital in the Intensive Care Unit in mechanical ventilation and tracheostomy for
prolonged intubation (more than 21 days). In addition, he presented psychiatric post-traumatic syndrome
in treatment for 5 months.
Patient 5 days before admission presented "flu-like process" characterized by rhinorrhea, cough and
general malaise, with symptomatic treatment; 1 day before admission he presented shortness of breath
despite the use of salbutamol inhaler with no apparent improvement; the day of admission patient with
increased respiratory distress and decreased oxygen saturation going directly to the trauma shock unit.
BP: 155/100 mmHg HR: 130 min FR: 30 x min T°: 37.2 °C Sat O2: 87%.
On examination, decreased vesicular murmur in both lung fields with diffuse wheezing; rhythmic,
tachycardic heart sounds of regular intensity, no murmurs; Glasgow Coma Scale: 15, no meningeal signs or
focalization.
DIAGNOSIS AND INITIAL MANAGEMENT: severe asthmatic crisis. Oxygen therapy; Nebulization with SABA/SAMA,
intravenous and inhalation corticotherapy, intravenous magnesium sulfate.
EVOLUTION AND TREATMENT: 40 minutes after admission to the trauma shock unit, the patient was evaluated
with arterial blood gas examination interpreted as respiratory acidosis and hypoxemia; also vital
functions: BP: 160/100 mmHg HR: 155 x min FR: 32 x1min Sat O2; 81% (FiO2 0.40) with final diagnosis of
ALMOST FATAL ASTHMA and orotracheal intubation is decided under rapid sequence using ketamine at a dose
of 2 mg/kg and mechanical ventilation (continuous pressure controlled mechanical ventilation: PC-CMV).
Poor respiratory mechanics, respiratory acidosis (pCO2: 64), previous history of severe asthmatic crisis
with orotracheal intubation and long-stay ICU (Figure 1 and Table 3).
|
PARAMETER |
RESULT FiO2: 0.40 |
NORMAL VALUES |
|---|---|---|
|
pH |
7.21 |
7.35-7.45 |
|
pCO2 (mmHg) |
64 |
35-45 |
|
PO2 (mmHg) |
58 |
80-100 |
|
Sat O2 (%) |
85 |
95-100 |
|
PaO2/FiO2 |
148 |
>300 |
|
HCO3 (mEq) |
25 |
22-26 |
Taken from the Manual of Diagnosis and Therapeutics in Pulmonology. 3rd ed. Chapter 35. Page 391. (https://www.neumosur.net/files/publicaciones/ebook/35-ASMATICA-Neumologia-3_ed.pdf)
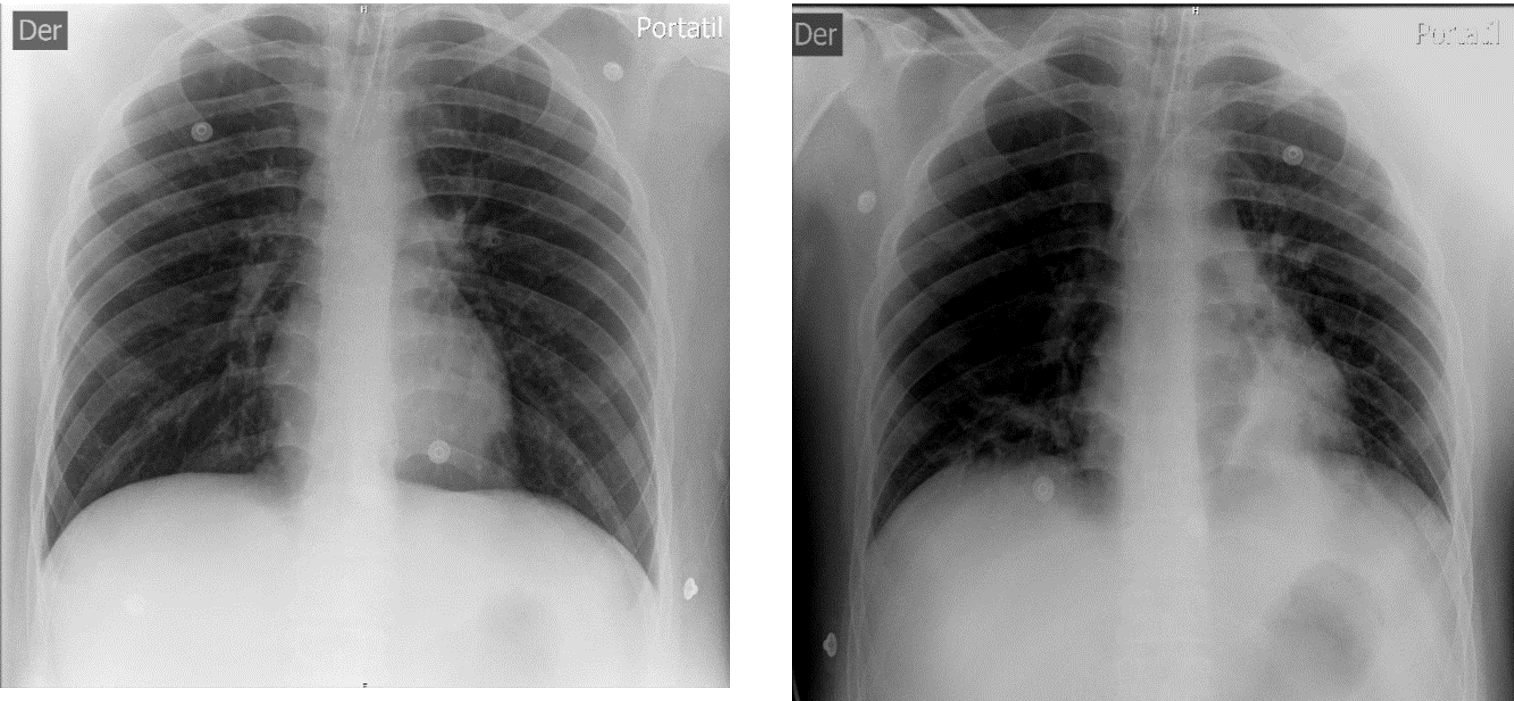
Figure 1: Chest X-ray, taken in emergency. 3a. Preserved radiotranslucent lung fields. Orotracheal tube in D3. 3b. Lung fields show left basal alveolar radio opacity. Central venous catheter projected in left subclavian vein.
Patient is transferred to the intensive care unit to continue management of critically ill patient on mechanical ventilation with diagnostics:
- Acute respiratory failure on mechanical ventilation
- Near-fatal asthma
- Respiratory sepsis: rule out aspiration pneumonia
- Asperger Syndrome
Daily evolution of the arterial blood gas test showing pCO2 correction on the second day and correction
of the acid-base disorder on admission (Table 4).
|
PARAMETER |
DAY 1 |
DAY 2 |
DAY 3 |
DAY 4 |
DAY 5 |
DAY 6 |
NORMAL VALUES |
|---|---|---|---|---|---|---|---|
|
pH |
7.20 |
7.19 |
7.27 |
7.40 |
7.52 |
7.52 |
7.35-7-45 |
|
pCO2 (mmHg) |
65 |
37 |
48 |
40 |
38 |
35 |
35-45 |
|
PO2 (mmHg) |
153 |
102 |
72 |
107 |
93 |
69 |
80-100 |
|
Sat O2 (%) |
99 |
98 |
95 |
98 |
98 |
96 |
95-100 |
|
PaO2/FiO2 |
191 |
340 |
300 |
382 |
332 |
180 |
> 300 |
|
HCO3 (mEq) |
25 |
14 |
22 |
24 |
31 |
28 |
22-26 |
Hemogram showing leukocytosis with left deviation on the second day (abstinence 9%) related to the
respiratory infectious picture associated with probable aspiration pneumonia (Table 3 and Figure 2).
|
HEMOGRAMA |
DIA 1 |
DIA 2 |
DIA 3 |
DIA 4 |
DIA 5 |
DIA 6 |
|---|---|---|---|---|---|---|
|
LEUCOCITOS |
17250 |
50260 |
41510 |
34790 |
26070 |
17510 |
|
HEMOGLOBINA |
11.5 |
11 |
10.1 |
10.3 |
10.9 |
12.6 |
|
PLAQUETAS |
354000 |
397000 |
361000 |
373000 |
380000 |
384000 |
|
ABASTONADOS |
1 |
9 |
5 |
2 |
3 |
2 |
|
SEGMENTADOS |
92 |
80 |
89 |
85 |
83 |
75 |
|
LINFOCITOS |
2 |
3 |
4 |
6 |
6 |
14 |
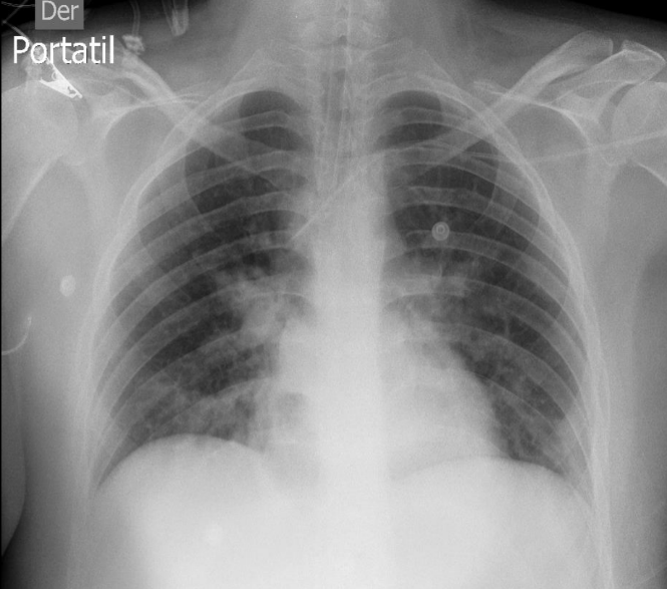
Figure 2: Chest X-ray in ICU. There is evidence of accentuation of the pulmonary interstitium, with confluent posterobasal alveolar opacities predominantly on the right and bilateral hilar reinforcement.
The mainstays of treatment were antibiotic therapy (Ceftriaxone/Clindamycin), intravenous and inhalation
corticotherapy, short-acting beta agonists (SABA), short-acting antimuscarinics (SAMA), magnesium
sulfate, aminophylline, sedoanalgesia and neuromuscular blocking agents (vecuronium).
Patient with favorable evolution, on the fourth day is extubated and on the sixth day goes to the
medical hospital for 3 days, discharged on the ninth day of emergency admission.
DISCUSSION
Near-fatal asthma defines a subset of patients with asthma who are at increased risk of death from their
disease. Studies show that deaths from asthma attacks typically occur in patients who present with
poorly controlled asthma and whose condition gradually deteriorates over days or weeks before presenting
with a fatal or near-fatal asthma episode.
Despite advances in treatment, asthma continues to be a disease of high prevalence and incidence
worldwide. Approximately 2 to 4% of hospitalized patients with critical asthma syndrome develop acute
ventilatory failure requiring mechanical ventilation, among which mortality ranges from 6.5% to 10.5%
(6).
Infections, especially viral infections, are also a risk factor as an important trigger for near-fatal
asthma. Viral nucleic acids have been detected in up to 55% of patients, and patients with asthma and
lower respiratory infection tend to have more severe and prolonged symptoms. There is progressive airway
obstruction, with mucus plugs, loss of respiratory epithelium, mucous gland hyperplasia and submucosal
eosinophilia (late phase). These patients have frequent use of bronchodilators and little use of inhaled
steroids with a higher risk of reaching an asthmatic state (6).
The signs and symptoms evidenced in the patient were progressive respiratory distress with decreased
oxygen saturation (87%), rescue treatment for severe asthmatic crisis was started on admission with
oxygen therapy, corticotherapy, SABA (nebulization) and SAMA (inhalation), magnesium sulfate 2g EV.
After 20 minutes the patient was clinically reevaluated, tachypnea and low oxygen saturation persisted
(81%), silent thorax and arterial gas analysis (pH: 7.21, pCO2: 64, pO2: 58, PaO2/FiO2: 148) with a
diagnosis of ALMOST FATAL ASTHMA and orotracheal intubation is decided by rapid intubation sequence with
the use of ketamine at a dose of 2 mg/kg, for its bronchodilator effect as it relaxes the bronchial
smooth muscle and mechanical ventilation with PC-CMV mode (continuous pressure controlled mandatory
ventilation). Among the poor prognostic factors that make us suspect and predict the possible use of
mechanical ventilation is the patient's history of mechanical ventilation for a similar asthmatic
crisis, associated with the lack of adherence to treatment (he only used the medication during
exacerbations) and the post traumatic psychiatric syndrome disorder associated with a history of
Asperger's syndrome; Apart from insufficient oxygenation and ventilation, the expected clinical
evolution of the patient was clinical deterioration and the need for intubation and mechanical
ventilation (PC-CMV).
The decisions made upon admission to the emergency room regarding intubation and early mechanical
ventilation may have influenced the patient's prompt recovery and discharge at 9 days, in contrast to
the previous similar situation.
It is important to know the history of emergency admission, adherence or not to the treatment received,
precipitating risk factors and clinical factors to decide on orotracheal intubation in this type of
patient, since early intervention improves morbidity and mortality (superinfections, prolonged stay).
CONCLUSION
Despite advances in treatment, asthma continues to be a disease of high prevalence and incidence
globally; asthmatic crises are an important percentage of emergency care; knowing, diagnosing and
treating this pathology in a timely and appropriate manner is very important for the patient's
prognosis.
Patients with near-fatal asthma have an increased risk of death from their disease, related to the
complication of the disease.
The signs and symptoms evidenced in the patient were progressive respiratory distress with decreased
oxygen saturation (87%), which did not respond to initial rescue treatment; persisting low oxygen
saturation (81%), at physical examination silent chest and arterial gas analysis examination pH: 7.21,
pCO2: 64, pO2: 58, PaO2/FiO2: 148; with diagnosis of ALMOST FATAL ASTHMA and orotracheal intubation is
decided by rapid intubation sequence.
The favorable response of the patient from his emergency admission, transfer to the intensive care unit
and discharge was determined by a rapid response to the emergency admission and the treatment followed
in the ICU.
Authorship contributions:
The authors participated in the conceptualization, research, methodology, resources and
writing of the original draft.
Financing:
Self-funded
Declaration of conflict of interest:
The authors declare that they have no conflict of interest.
Recevied:
April 3, 2024
Approved:
June 13, 2024
Correspondence author:
William Rojas Pérez.
Address:
Av. Simón Bolivar, cuadra 8 s/. Pueblo Libre.
Phone:
980514590
E-mail:
wrpmedico@gmail.com
Article published by the Journal of the faculty of Human Medicine of the Ricardo Palma University. It is an open access article, distributed under the terms of the Creatvie Commons license: Creative Commons Attribution 4.0 International, CC BY 4.0 (https://creativecommons.org/licenses/by/4.0/), that allows non-commercial use, distribution and reproduction in any medium, provided that the original work is duly cited. For commercial use, please contact revista.medicina@urp.edu.pe.
BIBLIOGRAPHIC REFERENCES
