Introduction
Mixed reality (MR) lies between augmented reality (AR) and virtual reality (VR), combining elements of both to offer a more advanced interactive experience. VR creates fully virtual and immersive environments that can engage multiple senses, while AR overlays virtual data onto the real-world environment, without deep interaction
1
. In contrast, MR integrates virtual data into the real environment, allowing real-time interaction, providing a more immersive and functional experience
2
3
, as shown in Table 1. Devices such as HoloLens enable the visualization of three-dimensional data during surgical procedures without disrupting the workflow, although they face challenges such as the need for specialized software and potential side effects for users
4
5
(Figure 1). Globally, the majority of studies have been conducted in the United States (1883), followed by England (677), Canada (600), Germany (509), and Italy (444), with Peru falling below 100 studies
6
. Despite these challenges, MR has the potential to transform surgery and medical education, improving precision and real-time decision-making.
Figure 1
Proposal for future collaborative implementation of brain surgery, utilizing virtual reality glasses to visualize the morphology of the organ. Original contribution.
Table 1. Comparison of mixed reality (MR) technologies in surgery
| Characteristic |
Augmented Reality (AR) |
Mixed Reality (MR)/th>
|
| Interaction |
Real-time direct or indirect view of a physical real-world environment enhanced/augmented by computer-generated information
7
8
.
|
It integrates physical and digital environments, allowing continuous interaction between them. It helps design and evaluate how users interact with physical and digital elements simultaneously
9
.
|
| Devices |
Phones, tablets, AR glasses, headsets like HoloLens
10
.
|
Head-mounted display, wearable display devices, monitor-based and projection-based screens
11
.
|
| Applications |
Advertising and commercial, entertainment and education, medicine, and mobile applications for iPhones
12
.
|
Education with integrated learning, collaborative design with virtual models in real environments
11
, neurosurgery, maxillofacial surgery, general surgery
13
.
|
In this context, computer-assisted surgery (CAS) emerges
14
15
, integrating mechatronic systems with MR to provide surgeons with training without compromising patient safety
16
, as seen in robotic surgery
17
, neurosurgery, orthopedics, laparoscopy, endoluminal intervention with flexible robots, the use of medical capsules, and unconnected micro/nano robots, among others, demonstrating significant progress in enhancing precision and minimizing invasiveness
18
(Figure 2). In 2009, Mauro et al. developed an MR neurosurgical microscope for training and intraoperative purposes, with realistic simulation (visual and haptic) for palpation of low-grade gliomas, along with augmented reality stereoscopic visualization of 3D data relevant for safe surgical movements in image-guided interventions
19
20
21
.
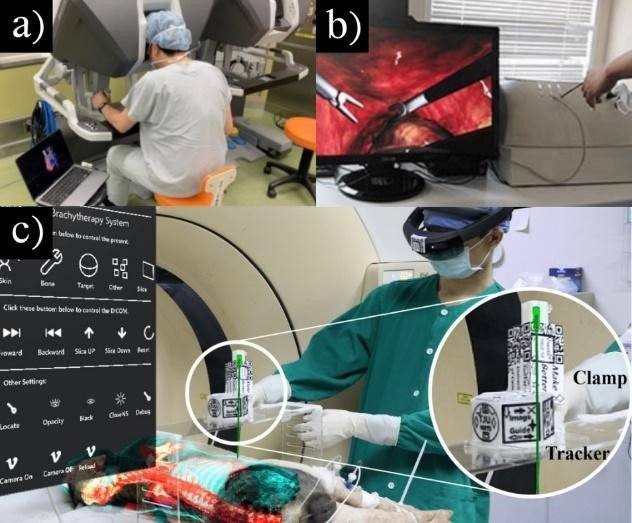
Figure 2
(a) Visualization of intraoperative surgery with 3D virtual reality models
22
.
(b) Laparoscopic simulator with high-fidelity soft tissue representation
23
.
(c) Mixed reality (MR) navigation system
24
.
Other studies have also explored the use of MR in surgical and microsurgical simulation environments. In 2020, Galati et al. proposed a system based on Microsoft HoloLens, a Digital Imaging and Communication in Medicine (DICOM) viewer, and a visualization tool developed in Unity. This system improves the speed and precision of surgeries by displaying real-time information directly in the surgeon's visor, eliminating the need to leave the operating table. However, this approach presents challenges such as increased physical strain, discomfort due to the device's weight, and battery autonomy issues
25
. In 2023, Xiang et al. developed an MR framework for microsurgery simulation, combining a surgical microscope with real precision instruments, offering an immersive experience with visual and tactile interaction. This system enables the practice of anastomosis skills and uses vision-based tracking to monitor instruments and artificial blood vessels, as well as to quickly create virtual assets in various microsurgical specialties
26
. Also in 2023, Jain et al. explored the use of mixed reality (MR) technology in neurosurgical teaching, given the decline in cadaveric dissections and the need for new learning methods. Three neurosurgeons served as facilitators using the HoloLens 2 device without prior student training. Eight neurosurgery residents evaluated the experience, finding a short learning curve and rating the device as engaging, reliable, and easy to use. Although opinions were mixed on whether MR should replace traditional methods, the study demonstrates that this technology is viable for neurosurgical training
27
. These studies highlight the potential of MR to enhance both training and surgical outcomes, though technological challenges remain to be addressed.
Application in surgical innovation
MR is gaining traction in surgical education, with several companies heavily investing in this technology (Table 2). Microsoft, through its HoloLens project and Windows Mixed Reality, has developed an MR system that combines high-precision hardware and software. This system has been used in medical, industrial, and educational applications, allowing surgeons to visualize three-dimensional holograms during surgical procedures without disrupting workflow. This technology improves precision and reduces errors; moreover, it is a pioneer in clinical studies and simulations
28
. Magic Leap, on the other hand, has developed light field technology that provides a better sense of fusion between the physical and virtual worlds, achieving greater realism in 3D image projection. This enables real-time medical collaboration and has enhanced training and diagnostics in surgical specialties
29
30
. Finally, MetaVision is bringing MR to the end user by commercializing a more affordable device, although it is geared toward the consumer market; this company has popularized MR and facilitated its adoption in medical education and clinical simulation
31
.
Table 2. Main features of the leading MR devices
| Device |
Main features |
Price (USD) |
| HoloLens (28) |
Transparent holographic lenses, 2-3 hours battery life in active use, Wi-Fi 802.11ac and Bluetooth 4.1 connectivity, 2MP cameras, 64GB storage. |
3,000 |
| Magic Leap One (28) |
40° FOV, 1280 x 960 resolution per eye, rechargeable battery, Bluetooth 4.2 and Wi-Fi connectivity, 1080p RGB color camera, 64GB SSD storage. |
2,500 |
| Meta 2 (32) |
90° field of view, 2.5K resolution, 9-foot cable for data and power, wired connectivity, 720p RGB camera, 128GB storage. |
1,500 |
In Mexico, the Universidad Nacional Autónoma de México (UNAM) successfully used an innovative lens system to visualize a hologram of the patient and performed the first surgery using MR. The experience gained has led to collaboration with Microsoft on a holographic surgery project involving specialists from 13 countries
33
, Additionally, in 2019, Arroyo-Berezowsky et al. conducted a study with 10 residents, where the VR group completed the task in 25.84 minutes, compared to 31.6 minutes for the control group, highlighting that the VR group tended to finish earlier
34
. On the other hand, in 2024, García et al. developed VirtualCPR, a virtual reality application for CPR training
35
. Finally, in 2016, Medellín-Castillo et al. presented a new 3D digital cephalometry approach with haptic support, which improved precision and reduced errors and variability compared to 2D and 2½D methods, proving to be more intuitive and efficient for dental surgeons
36
.
In Brazil, in 2016, da Cruz et al. studied preoperative warm-up with virtual reality simulators and found a significant improvement in surgical performance among medical students with basic laparoscopy experience
37
. Additionally, in 2016, de Faria et al. developed an interactive and stereoscopic resource for teaching neuroanatomy, significantly improving student learning compared to traditional teaching methods
38
.In Spain, researchers from the Universidad de Málaga demonstrated that virtual reality is a viable and more efficient alternative to 3D-printed models for classifying proximal humerus fractures in pre-surgical planning
39
.
In Peru, the situation is different. Although the country has approximately 35 medical schools or faculties in 18 of its 24 provinces, only about 14% of them use virtual reality interfaces
40
, and not all employ digital devices or have annual subscriptions for courses such as Physiology, Anatomy, Histology, Surgery, and/or Pathology
41
42
43
. This contrasts with other countries in the region and around the world that are promoting the use of augmented and virtual reality to improve educational processes
44
45
. While efforts are being made to incorporate new technologies in line with global developments, such as the use of surgical robots like Da Vinci
46
, the current Peruvian context requires an accelerated renewal of medical education systems
47
48
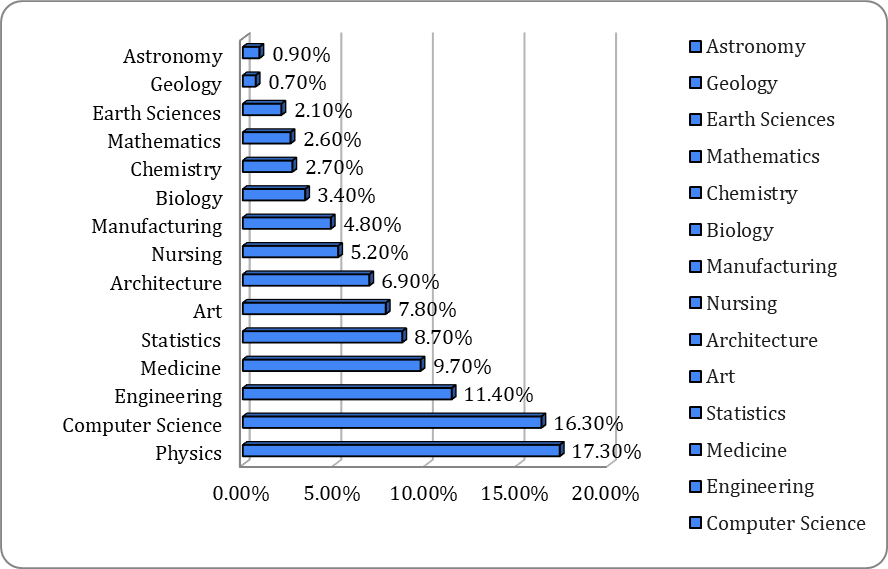
, This should go beyond conventional educational objectives and include reforms ranging from the student admission process to organized educational quality. The use of mixed reality (MR) in education in Peru is more common in Physics (15%), Computer Science, and Engineering (around 12%), while disciplines such as Astronomy, Geology, and Earth Sciences have much lower adoption rates (less than 2%). This suggests that technological and scientific areas benefit more from MR, while other fields are still lagging behind in its use (Figure 3).
Figure 3
Current state of MR use in education in Peru
49
Conclusion
To effectively implement these technologies in Latin America, several factors need to be considered: investment in infrastructure, healthcare personnel training, and adaptation to local needs
49
. MR has enormous potential to enhance both medical education and patient treatment
50
, especially compared to Europe and North America, where significant increases in surgical efficiency have been observed. There is a weighted mean difference of 12.31 in skill training capacity
51
along with improvements in educational quality, as the average time of surgical procedures has been reduced to 97.62±35.59 minutes, compared to traditional cadaver-based teaching methods, which have an average time of 121.34±12.17 minutes
52
53
. Despite financial and infrastructural challenges, lessons learned from other regions can guide the successful integration of mixed reality into the Latin American medical field, adapting to its unique context
54
55
(figura 4).
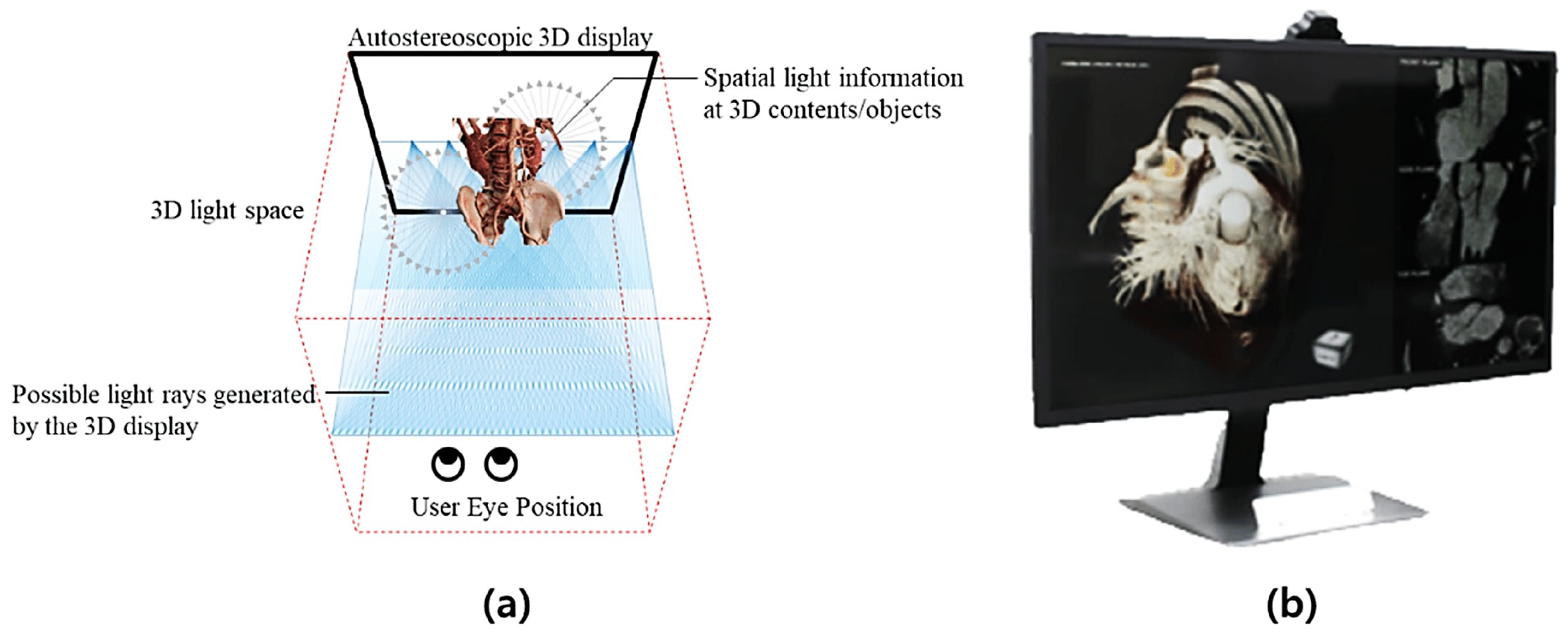
Figure 4
(a) Concept of 3D light field visualization based on eye-tracking, illustrating the generation and modeling of directional light rays.
(b) 3D visualization prototype for medical applications: 3D cardiac computed tomography navigator. Obtained under the CC BY 4.0 license
56
.