ORIGINAL PAPER
REVISTA DE LA FACULTAD DE MEDICINA HUMANA 2020 - Universidad Ricardo PalmaDOI 10.25176/RFMH.v20i4.2873
THE COMPARISON OF APACHE II AND BISAP SCALES IN THE PROGNOSIS OF ACUTE PANCREATITIS IN A HOSPITAL IN PERU
COMPARACIÓN DE LAS ESCALAS APACHE II Y BISAP EN EL PRONÓSTICO DE PANCREATITIS AGUDA EN UN HOSPITAL DEL PERÚ
Omar V. García-Revilla1,2, Lucy E. Correa-López2,3, Richard I. Rubio-Ramos2,3, Maria Loo-Valverde2,3
1Servicio de Medicina Interna y Unidad de Cuidados Intensivos, Hospital María Auxiliadora, Lima-Perú.
2Facultad de Medicina, Universidad Ricardo Palma, Lima - Perú.
3Instituto de Investigación de Ciencias Biomédicas, Universidad Ricardo Palma, Lima – Perú.
Introduction: Acute pancreatitis continues to be a disease with significant morbidity and mortality. Clinical criteria diagnose it, and the inflammatory process can lead to organ failure. Objective: This study compared the APACHE II and BISAP scales in organ failure development in patients with acute pancreatitis from a public hospital in Peru. Methods: A diagnostic test validation study was carried out. The medical records of patients hospitalized with the diagnosis of acute pancreatitis in the Internal Medicine service and the Intensive Care Unit were evaluated. The APACHE II and BISAP scales were applied, the ROC curve, sensitivity, specificity, positive and negative predictive value were calculated. SPSSv23 was used for statistical analysis. Results: 146 patient records that met the inclusion criteria were evaluated. An area under the curve of 0.957 was obtained for BISAP and 0.996 for APACHE II. It had a sensitivity and specificity for APACHE II of 83% and 99%, for BISAP of 66% and 99%. The positive and negative predictive value for APACHE II is 83% and 99%, and for BISAP 80% and 98%. Conclusion: The APACHE II scale was superior to detect organ failure. It was determined that both scales have high specificity, the sensitivity being more significant in the BISAP scale.
Keywords: Acute pancreatitis; Organ failure
RESUMEN
Introducción: La pancreatitis aguda continúa siendo una enfermedad con morbilidad y mortalidad significativas. Se diagnostica mediante criterios clínicos y el proceso inflamatorio puede llegar hasta una falla de órganos. Objetivo: Comparar las escalas de APACHE II y BISAP en el desarrollo de falla orgánica en pacientes con pancreatitis aguda de un hospital público del Perú. Métodos: Se realizó un estudio de validación de prueba diagnóstica. Se evaluaron las historias clínicas de pacientes que estuvieron hospitalizados con el diagnóstico de pancreatitis aguda en el Servicio de Medicina Interna y la Unidad de Cuidados Intensivos. Se aplicó las escalas APACHE II y BISAP, se calcularon curva ROC, sensibilidad, especificidad y valores predictivo positivo y negativo. Para el análisis estadístico se utilizó el SPSSv23. Resultados: Se evaluaron 146 historias de pacientes que cumplían con los criterios de inclusión. Se obtuvo un área bajo la curva de 0.96 para BISAP y 0.99 para APACHE II; con una sensibilidad y especificidad para APACHE II de 83% y 99%, para BISAP de 66% y 99%. El valor predictivo positivo y negativo para APACHE II es 83% y 99% y para BISAP 80% y 98%. Conclusion: La escala de APACHE II fue superior para detectar falla de órganos. Se determinó que ambas escalas poseen alta especificidad, siendo mayor la sensibilidad en la escala BISAP.
Palabras Clave: Pancreatitis aguda; Falla de órganos
In 2015 in the United States, pancreatitis was the third cause of the most frequent hospital admissions, presenting a worldwide incidence that ranges from 4.9 - 73.4 x 100,000 inhabitants(1). Most patients present mild symptoms, and severe conditions can present up to a mortality rate of 20%(2). Organ failure is the main cause and determinant of severity and early mortality, while late deaths are due to secondary infections, including infected pancreatic necrosis and sepsis(3).
In a study carried out in Mexico, there was 80% mild pancreatitis and a mortality rate of severe pancreatitis of 25% to 30%(4). In another study, biliary etiology was the most frequent (66%), followed by alcoholic (15%)(5). It has been described that the incidence varies according to alcohol consumption and the presence of gallstones(6).
In Peru, there are few studies on this pathology; the Ministry of Health published a study in which the incidence was 28 cases per 100 000 inhabitants(7). Other authors showed that the most frequent etiology was biliary, reaching 80-100% in some centers,(8) the second cause was alcohol, followed by dyslipidemias, and others. The ability to predict the severity and mortality of pancreatitis will help the clinician screen patients with increased morbidity and mortality risk. Several severity rating scales are used, such as APACHE II, BISAP, and RANSON. These can be useful to institute appropriate and timely therapeutic strategies, providing information on the patient's status upon admission and in the first 24 or 48 hours, depending on the scale(9,10).
Due to those mentioned above, this study’s objective was to compare the APACHE II and BISAP scales in the prognosis of organ failure in hospitalized patients with acute pancreatitis in a public hospital in Peru.
METHODS
Design and study area study
A diagnostic test validation was carried out and analytical, comparing the PACHE II and BISAP scales’ predictive power in the development of organ failure in acute pancreatitis, considering the new Atlanta classification of the Service of Internal Medicine and Intensive Care Unit of the Hospital María Auxiliadora in 2017, Lima-Peru.
Population and sample
The medical records of patients with a diagnosis of acute pancreatitis, over 18 years of age, hospitalized were reviewed and included, pregnant patients, a history of chronic pancreatitis. Patients seen in the outpatient clinic, and with another associated pathology were excluded acute pancreatitis. It conditions a state of sepsis or increases their hospital stay, such as chronic renal failure, heart disease, COPD, HIV, oncological diseases, and patients who requested their voluntary withdrawal or the datasheet was incomplete.
Variables and Instruments
Concerning the APACHE II scale, several authors take the value of 8 as the cut-off point. Gompertz(11) carried out a study where he raised the cut-off point requirement from 8 to a cut-off point of 12, obtaining the more certain prediction of complications and mortality. Therefore, this work was decided to take a score greater than 12 to develop organic failure. Likewise, for the BISAP scale, the value of 3 was taken to determine the development of organ failure and the prognosis of the disease(12).
Statistic analysis
The SPSS version 23.0 program was used to process the collected data. The ROC curve, sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of both scales were calculated to evaluate organ failure risk.
Ethical aspects
This study complies with current regulations on clinical and bioethical research. The authorization was obtained from the Institutional Ethics and Research Committee of the María Auxiliadora Hospital and the Research Institute’s approval in Biomedical Sciences of the Ricardo Palma University. The medical records were consulted, preserving the confidentiality and privacy of the patients. The present work does not evaluate the therapeutic intervention, nor does it present images or personal data that allow patients to be identified.
RESULTS
We included 146 patients diagnosed with acute pancreatitis who met the inclusion criteria. Table 1 shows demographic, clinical characteristics, and laboratory data. The average age of 44.2 years was observed; it was more frequent in females with 67.1%. The average hospitalization days were 6 days(2,17). Similarly, in the background, 17 patients (11.6%) with Type 2 Diabetes Mellitus were evidenced, and 5 patients (3.4%) had cholecystectomy before acute pancreatitis.
TablE 1. Frecuencia de las características clínicas, demográficas y datos de laboratorio
| Variables | Number / Mean | Percentage / Interval |
| Age (years) | 44,3 | 41,7 - 46.9 |
| Days of hospitalization | 6,4 | 5,6 - 7.2 |
| Gender | ||
| Female | 98 | 67.1 % |
| Male | 48 | 32.8% |
| Diabetes Type 2 | 17 | 11.6 % |
| Previous cholecystectomy | 5 | 3.4% |
| Previous acute pancreatitis | 10 | 6.8% |
| Etiology | ||
| Biliary | 131 | 89.7% |
| Alcohol | 9 | 6.16% |
| Post ERCP | 2 | 1.4% |
| Dyslipidemias | 3 | 2.1% |
| Others | 1 | 0.7% |
| Laboratory | ||
| Hematocrit % | 36 | 34,6 - 39,3 |
| Leukocytes /ul | 11247 | 9658.5-12258.6 |
| Amylase /ul | 1594 | 1414,5 - 1775 |
| Lipase /ul | 1183 | 1002,0 - 1365,7 |
The distribution according to etiology of acute pancreatitis was: mainly biliary in 131 patients (89.7%), followed by alcohol consumption in 9 patients (6 %), post-ERCP acute pancreatitis (second and third day) in 2 patients (1.4%), dyslipidemia in 3 patients (2.1%) and 1 patient (0.7%) due to idiopathic causes.
The mean hematocrit was 36% within the laboratory tests, and for leukocytes, it was approximately 13000 / ul. The average amylase and lipase were 1594 / ul and 1183 / ul, respectively.
The degrees of severity and organ failure of the APACHE II and BISAP scales were evaluated and are shown in Table 2. For the APACHE II scale, a score greater than or equal to 12 was considered for the detection of organ failure, obtaining 6 patients who had this diagnosis while for the BISAP scale, the cut-off point was 3, obtaining 4 patients with organ failure and two other patients were found below this cut-off.
Table 2. Grades of severity and organ failure according to the APACHE II and BISAP.
| Scales | Number (Percentage) | Organic Failure (Number) |
| APACHE II | 3.11 (2.5-3.6) | 0 |
| < 8 | 133 (91%) | 0 |
| 8 | 2 (1.4%) | 0 |
| 9 | 3 (2.1%) | 0 |
| 10 | 1 (0.7%) | 0 |
| 11 | 1 (0.7%) | 0 |
| >=12 | 6 (4.1%) | 6 |
| BISAP | ||
| 0 | 87 (59%) | 0 |
| 1 | 43 (29%) | 0 |
| 2 | 11 (7.5%) | 2 |
| 3 | 3 (2.1%) | 2 |
| 4 | 2 (1.4%) | 2 |
| 5 | 0 (0%) | 0 |
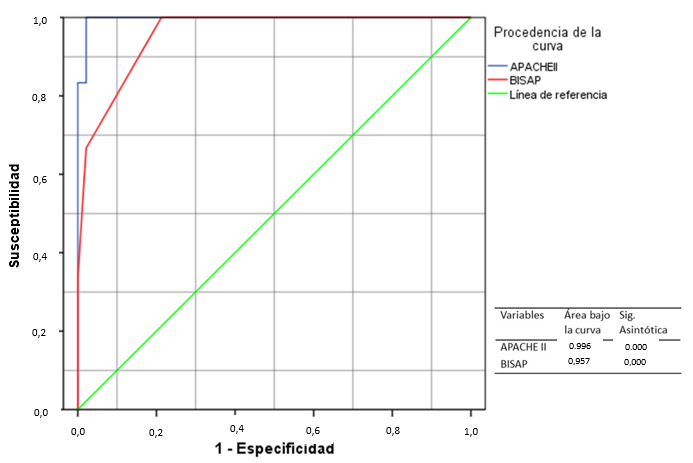
An area under the curve of 0.996 for the APACHE II scale and 0.957 for the BISAP scale, both with a p = 0.000. Figure 1. The sensitivity and specificity for APACHE II were 83% and 99%, while for BISAP, it was 66% and 99%. Table 3.
The days of hospitalization of patients with acute pancreatitis evaluated with the APACHE II and BISAP scales are represented in Table 4.
Table 3. Assessment of the APACHE scales II and BISAP
| Assessment of Tests | APACHE II | BISAP |
| Sensitivity | 83% | 66% |
| Specificity | 99% | 99% |
| Positive Predictive Value | 83% | 80% |
| Negative Predictive Value | 99% | 98% |
Table 4. Days of hospitalization for the APACHE II and BISAP scales
| BISAP SCORE | APACHE II SCORE | |||||||||||||||
| 0 | 1 | 2 | 3 | 4 | Total | <8 | 8 | 9 | 10 | 11 | >=12 | Total | ||||
Days of Hospitalization |
2 | 3 | 0 | 0 | 0 | 0 | 3 | Days of Hospitalization |
2 | 3 | 0 | 0 | 0 | 0 | 0 | 3 |
| 3 | 25 | 3 | 0 | 0 | 0 | 28 | 3 | 28 | 0 | 0 | 0 | 0 | 0 | 28 | ||
| 4 | 21 | 10 | 0 | 0 | 0 | 31 | 4 | 31 | 0 | 0 | 0 | 0 | 0 | 31 | ||
| 5 | 17 | 5 | 1 | 0 | 0 | 23 | 5 | 23 | 0 | 0 | 0 | 0 | 0 | 23 | ||
| 6 | 8 | 6 | 0 | 0 | 0 | 14 | 6 | 13 | 0 | 1 | 0 | 0 | 0 | 14 | ||
| 7 | 6 | 8 | 3 | 1 | 0 | 18 | 7 | 14 | 2 | 1 | 0 | 0 | 1 | 18 | ||
| 8 | 0 | 4 | 2 | 0 | 0 | 5 | 8 | 3 | 0 | 1 | 0 | 0 | 1 | 5 | ||
| 9 | 3 | 3 | 0 | 0 | 0 | 6 | 9 | 5 | 0 | 0 | 1 | 0 | 0 | 6 | ||
| 10 | 1 | 1 | 1 | 0 | 0 | 3 | 10 | 3 | 0 | 0 | 0 | 0 | 0 | 3 | ||
| 11 | 0 | 1 | 2 | 0 | 0 | 3 | 11 | 3 | 0 | 0 | 0 | 0 | 0 | 3 | ||
| 12 | 1 | 1 | 1 | 0 | 0 | 3 | 12 | 3 | 0 | 0 | 0 | 0 | 0 | 3 | ||
| 13 | 0 | 1 | 1 | 0 | 0 | 1 | 13 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | ||
| 15 | 0 | 0 | 0 | 0 | 1 | 2 | 15 | 0 | 0 | 0 | 0 | 1 | 1 | 2 | ||
| 17 | 0 | 1 | 0 | 0 | 0 | 1 | 17 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | ||
| 18 | 1 | 0 | 0 | 0 | 0 | 1 | 18 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | ||
| 20 | 1 | 0 | 0 | 0 | 1 | 2 | 20 | 1 | 0 | 0 | 0 | 0 | 1 | 2 | ||
| 25 | 0 | 0 | 0 | 1 | 0 | 1 | 25 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | ||
| 27 | 0 | 0 | 0 | 1 | 0 | 1 | 27 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | ||
| Total | 87 | 44 | 13 | 6 | 6 | 146 | 133 | 2 | 3 | 1 | 1 | 6 | 146 | |||
DISCUSSION
Acute pancreatitis presents an unpredictable clinical course from patients with few symptoms to patients with high mortality; leading to a search for highly effective severity scales to predict severity and mortality that are accessible, easy to use and cheap for vigorous therapeutic intervention(13).
This study found 98 female patients (67.1%) and 48 male (32.8%) with an average age of 44.25 years with values within a range of 41.65- 46.85, similar results were found by other authors regarding these characteristics of the population(14,15).
According to the etiology of pancreatitis, biliary, and alcoholic predominate in 89.7% and 6% respectively, our results are similar or reported by other investigations, of 75% and 7% respectively(16,17).
In the present validation study, organ failure in acute pancreatitis was considered according to the new Atlanta 2012 classification. Regarding the severity indexes, the majority of acute pancreatitis were mild. In the case of the BISAP scale, about 89% presented a score of 0 or 1, with a score of 3, 4 patients were classified with organ failure, no patients with a score of 5. In the APACHE II scale, the cut-off point of 8 was taken as a cut-off point for this research to classify it as a mild condition, with 91% of the patients being in this category. On the other hand, a value of 12 was taken to qualify it as a severe condition, 6 patients with this score presented organ failure. No deaths were recorded. These findings are similar to those found by Aguilar Gaibor in 2016 in Ecuador, who reported 85% of cases of mild acute pancreatitis and 14.2% of severe cases(9).
It is essential to validate these scales to detect organ failure early and start with the appropriate treatment, which will be different for the severity of the condition; It can be seen that the BISAP scale (99%) and APACHE II (99%) have high specificity for acute pancreatitis. However, the APACHE II scale (83%) has greater sensitivity than the BISAP scale (66%) to detect organ failure in acute pancreatitis patients. In the same way, Alvarado, in 2017, Peru carried out the study "Utility of the BISAP and APACHE II scores as predictors of severity of acute pancreatitis," where he demonstrated that the APACHE II scale was a better predictor than the BISAP scale for organ failure. In this study, the value of 8 for the APACHE II scale and 2 for the BISAPscale was taken to develop organ failure(18).
In our work, it was observed that the negative predictive value was high for both scales close to 100%, in addition to the positive predictive value, their results were similar, presenting the APACHE II scale with a minimal difference, showing that the probability of detecting failure of organs in acute pancreatitis having a score equal to or greater than 12 is higher than having a score greater than or equal to 3 on the BISAP scale. The results were similar in the Gompertz study; where most patients have mild symptoms of this disease, they conclude that the BISAP score ≥ 3 has a PPV: 88.33% and NPV: 98.36%(11). However, in his study, Alvarado found for the BISAP <2 scales a PPV: 36.36% and NPV: 91.26%; for the APACHE II scale> 9, he found a PPV: 55.17% and an NPV: 95.33%(18). The difference in the various studies results is due to the cut-off point used in the scale.
Both scales studied have a similar area under the curve (APACHE II: 0.996, BISAP: 0.957 both with a p = 0.000), the APACHE II scale being the one with the most significant power to detect the prognosis of this disease. The area under the curve of the BISAP scale is comparable with the results of other studies such as Barcia (0.918)(17), Gompertz (0,98)(11), Aguilar (0,94)(9). The BISAP scale is suitable for predicting organ failure in patients with acute pancreatitis.
Most of the patients had mild acute pancreatitis, and this is correlated with a short hospital stay. However, the patients who developed a severe picture of acute pancreatitis had a prolonged hospital stay, related to organ failure. This is consistent with the result in the Gompertz study(11).
The study’s main limitation is the low frequency of severe acute pancreatitis, making the predictive power for severity limited. Still, it has a high negative predictive value to rule out organ failure. However, failure prediction should be used with caution in clinical practice, always paying attention to other clinical signs that patients may present.
A multicenter study must be carried out in the future perspective, with greater statistical power to confirm our results.
CONCLUSION
In our study, the APACHE II scale was superior in predicting and detecting organ failure. It was determined that both scales have high specificity; however, the APACHE II scale presented greater sensitivity than the BISAP scale. The severity of acute pancreatitis is correlated with a hospital stay.
Author Contributions: The authors participated in the genesis of the idea, project design, data collection and interpretation, analysis of results and preparation of the manuscript of this research work.
Financing: This research has not received specific aid from public sector agencies, commercial sector or non-profit entities.
Conflicts of interest: The authors declare no conflicts of interest in the publication of this article.
Received: November 15, 2019
Approved: August 15, 2020
Correspondence: Omar Víctor García Revilla
Address: Urb. La Libertad Mz. E Lt 26 Surco.
Phone: +51944407928
Email: omarvictor_m200@hotmail.com
BIBLIOGRAPHIC REFERENCES