INTRODUCTION
Primitive neuroectodermal tumors (PNET) are a family of malignant neoplasms composed of small, round cells, which are derived from the neural crest. They can be classified according to their tissue of origin into three groups: 1) Central PNET (cPNET), originating in the central nervous system, such as medulloblastoma; 2) Neuroblastoma, originating from the autonomic system ganglia; and 3) Peripheral PNET (pPNET), which arises in peripheral nerves and manifests in soft tissues
1
,
2
. Additionally, within peripheral PNETs, the following are included: Ewing’s sarcoma (ES), peripheral neuroepithelioma of the bone and soft tissues, Askin's tumor (peripheral neuroepithelioma located in the thoracic and pulmonary region), melanotic neuroectodermal tumor (or malignant melanoma), ectomesenchymoma, and peripheral medulloepithelioma
2
.
The third group, composed of pPNETs, is more common in adolescents and young adults, with a slight male predominance, and represents 4% of malignant neoplasms in childhood and adolescence
3
. The real incidence of pPNETs is difficult to estimate due to its rarity, although it is proposed to be 2.9 per million inhabitants per year
4
. According to the World Health Organization, the Ewing’s sarcoma family of tumors includes: pPNET, classic ES, and extraskeletal ES. These tumors present specific chromosomal abnormalities, mainly the translocation t(11,22)(q24,12)
5
. ES and pPNET represent a spectrum of neuroectodermal differentiation, ranging from the least differentiated (ES) to the most neural differentiation (pPNET)
6
It is worth mentioning that the WHO, in the 2013 classification of tumors, removed PNET as a synonym for ES
7
.
The objective is to report the case of a 32-year-old female patient with an inguinal mass whose immunohistochemical profile was compatible with PNET, treated with chemotherapy and induction thalidomide.
CASE REPORT
A 32-year-old female patient, born and residing in Lima (capital of Peru), with a family history of a mother deceased from biliary tract neoplasia, and a personal history of pancreatitis in 2022 and laparoscopic cholecystectomy in 2023. The duration of the illness was one month, with a sudden onset and progressive course, characterized by the growth of a hard mass on the inner aspect of the right thigh, limiting thigh flexion due to pain.
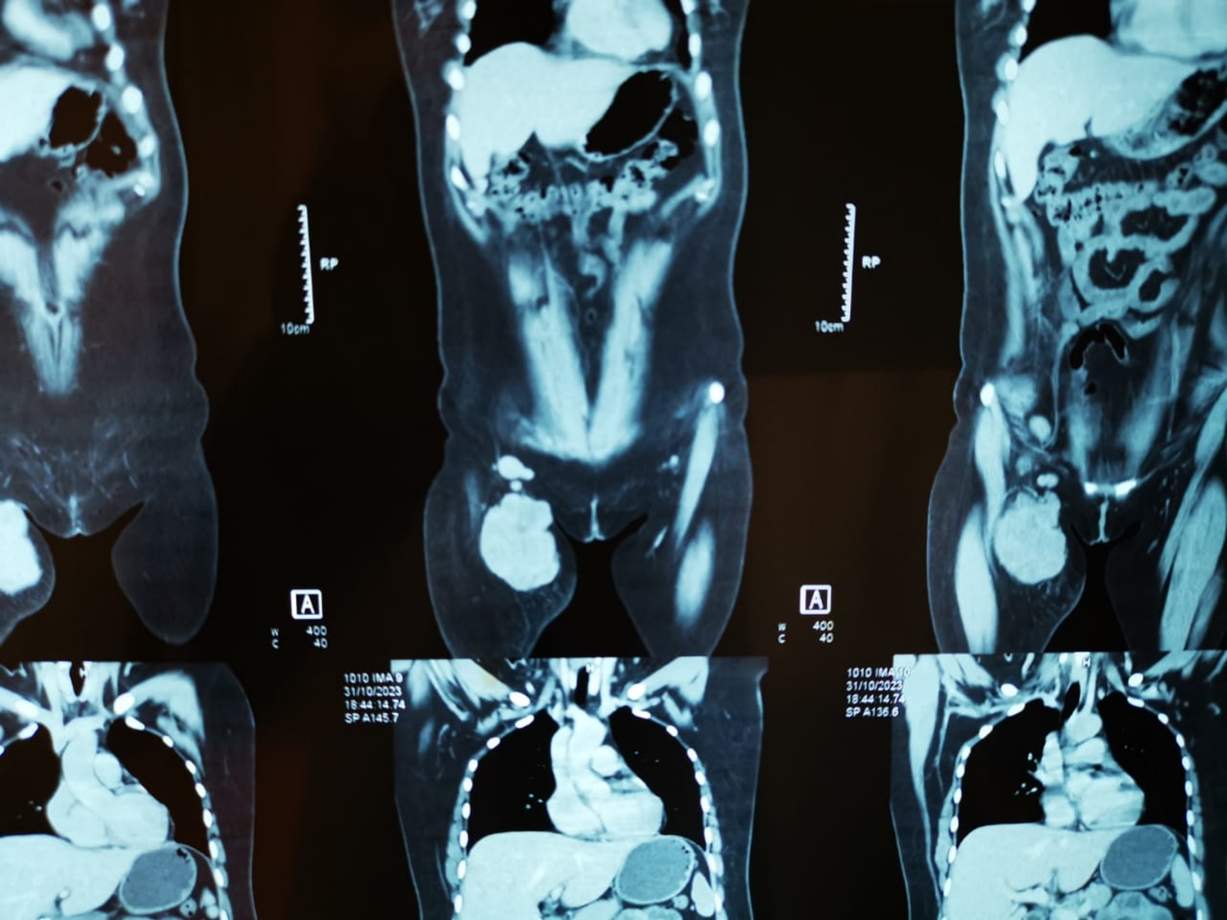
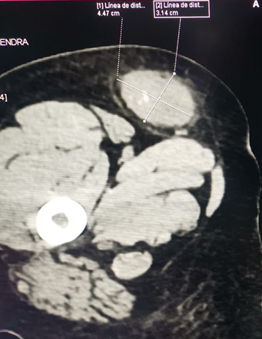
The imaging results showed a neoplastic lesion with heterogeneous contrast uptake (approximately 9 cm x 5 cm), increased fat density, deep inguinal adenopathies, without vascular, muscular, or bone involvement (figure 1A).
Figure 1
1A: Magnetic resonance imaging shows a large expansive mass approximately 9 x 5 cm in the right groin with lymph nodes involvement.
1B: Multislice spiral computed tomography post-induction chemotherapy, showing the tumor reduced to approximately 4 x 3 cm.
A tru-cut biopsy of the tumor lesion was performed, and the histopathological study using hematoxylin-eosin staining revealed a neoplasm of round cells with small, hyperchromatic, monomorphic nuclei, a high mitotic index, and areas of necrosis.
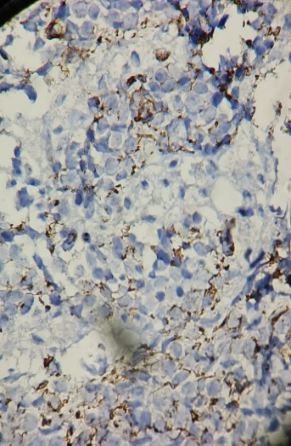
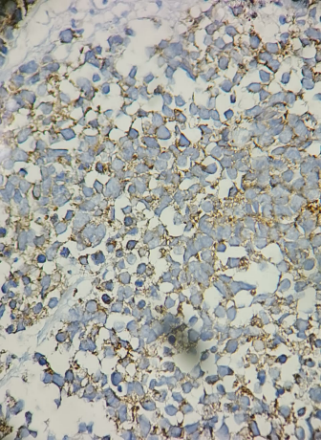
The immunohistochemical study showed the following findings: Pan-keratin negative, desmin negative, CD45 negative, CD99 negative, S100 negative, chromogranin negative, Fili-1 negative, ALK-1 negative, PGAF negative, TDT negative, synaptophysin positive, neurofilament positive in some neoplastic cells, Ki-67: 70%, and SOX-11 positive (figure 2). Conclusion: Peripheral Primitive Neuroectodermal Tumor (pPNET).
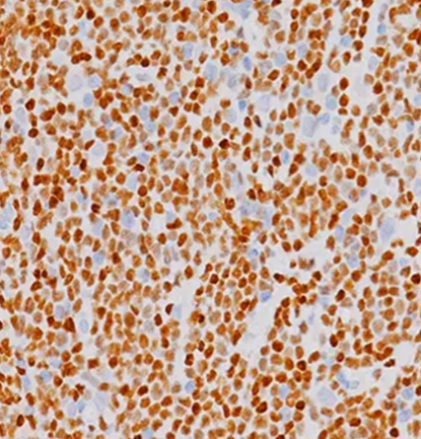
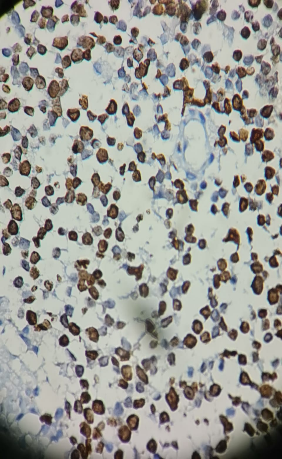
Figura 2
2A: Neurofilament positive in some cells; 2B: Synaptophysin positive; 2C: SOX-11 positive; 2D: Ki67 70%. 32-year-old patient diagnosed with Peripheral Primitive Neuroectodermal Tumor (pPNET).
Induction chemotherapy was initiated with four courses of carboplatin-etoposide every 21 days. Additionally, thalidomide was administered for 80 days at 100 mg once daily, along with acetylsalicylic acid 100 mg once daily to prevent venous thromboembolism, a known adverse effect of thalidomide.
After four sessions of induction chemotherapy (carboplatin-etoposide-thalidomide), the tumor mass reduced by 60%, as seen in the follow-up CT scan, showing a decrease in size to 4 x 3 cm (Figure 1B). The patient subsequently underwent surgical resection: a compartmentectomy of the anterior thigh region with a wide resection of the inguinal area, including regional lymph nodes. The macroscopic examination revealed the first surgical specimen measured 12 x 7.5 x 4.5 cm, with a yellowish-brown, adipose appearance and soft consistency. Upon sectioning, a fleshy, salmon-colored lesion with solid yellowish-white areas measuring 3.5 x 2.5 x 1 cm was observed, with clear surgical margins. Out of the nine lymph nodes examined, seven showed neoplastic involvement.
Postoperatively, the patient received adjuvant radiotherapy with 6 Mv photons using 3D technique on the proximal third of the right thigh, with a total dose of 46 Gy in 23 sessions plus a 20 Gy boost in the surgical bed. The patient is currently completing maintenance chemotherapy.
DISCUSsioN
The significance of this case lies in the rare presentation of pPNET in the inguinal region, as well as the multidisciplinary approach to its treatment, which included induction chemotherapy and thalidomide.
Peripheral Primitive Neuroectodermal Tumors (pPNETs) are extra-cranial tumors that can develop in any part of the bone or soft tissues. In the latest review, the most common location was the abdominopelvic region (46%), followed by the thoracopulmonary region (28%), extremities (10%), paravertebral (7.9%), and head and neck (7.9%)
8
.
For diagnosis, at least two positive neuronal markers and/or Homer-Wright rosettes are required
9
; PNETs are typically positive on immunohistochemistry for antigens such as CD99, 12E7, E2, 013, and HBA71, all of which are products of the MIC 2 gene, as well as synaptophysin, NSE, PGP9.5, vimentin, S100, and neurofilament, indicating neuroectodermal differentiation and supporting the diagnosis of pPNET
10
. It is also important to request a karyotype, as the most common mutation associated with SE-PNET is t(11;22), with some known variants such as t(21;22), t(7;22), and t(1;16)
11
. In the immunohistochemical profile, 90% to 100% of patients with pPNET are positive for CD99, which is a specific marker
8
.
In the latest review, the median age at diagnosis was 25 years (5 to 73 years), with a mean tumor size of 12.6 cm (1-30 cm). Lymph node metastasis was present in 19% of patients, and distant metastasis occurred in 18%, with bones and lungs being the most common sites of metastasis
8
.
The treatment of these tumors is multidisciplinary, including ablative surgery, chemotherapy, and adjuvant radiotherapy. Complete surgical excision is the cornerstone of treatment, although induction chemotherapy with postponed surgery remains an option. Zimmermann et al. support the need for neoadjuvant chemotherapy, as well as mandatory adjuvant chemotherapy and radiotherapy, due to the high percentage of patients with local recurrence and postoperative distant metastasis
12
.
Thalidomide is an oral sedative that was withdrawn from the market in the 1960s due to its teratogenic effects. However, it possesses immunomodulatory properties, and it is currently being used or tested in clinical trials for over 40 different diseases
13
. In oncology, thalidomide has demonstrated significant effects: an antitumor effect by inducing TNF-α degradation, antiangiogenic effects by inhibiting tumor angiogenesis through the blockade of VEGF (a potent angiogenic factor secreted by cancer cells in response to hypoxia), and antiproliferative and pro-apoptotic activity in tumor cells
13-15
.
Regarding its use in pPNET, research is still limited. One reported case involved a young patient with pulmonary pPNET who did not respond to VAC-IE chemotherapy (intensive vincristine + ifosfamide + etoposide + cyclophosphamide + doxorubicin) or second-line gemcitabine + cisplatin. Eventually, three cycles of temozolomide + irinotecan plus thalidomide were administered, resulting in symptom relief
16
. During follow-up, the patient received a daily dose of 200 mg thalidomide for 21 days, maintaining stable condition
16
. Initial CT showed a lesion measuring 88 mm x 82 mm, while follow-up CT revealed a drastic reduction in tumor size, suggesting that thalidomide may be a viable option for maintenance therapy in pPNET
16
.
Pramanik et al. concluded that patients with PNET did not benefit from metronomic chemotherapy that included daily celecoxib and thalidomide with alternating periods of etoposide and cyclophosphamide in pediatric patients with non-hematopoietic extracranial solid malignancies that progressed after at least two lines of chemotherapy
17
. These are the only studies to date that have observed thalidomide use in pPNET, although it has been more extensively studied in neuroblastoma.
In our patient, the lesion was located in the inguinal area, measuring 3.5 x 2.5 x 1 cm with lymph node involvement. Imaging studies showed no distant metastasis, and the immunohistochemical profile was negative for CD99 but positive for synaptophysin and neurofilament, identifying it as an inguinal PNET that responded well to induction chemotherapy with carboplatin-etoposide and thalidomide, followed by surgery, adjuvant radiotherapy, and maintenance chemotherapy.
CONCLUSIONS
In this patient, the multidisciplinary treatment for pPNET benefited from the use of chemotherapy and thalidomide during the induction phase, which resulted in a 60% tumor reduction, followed by compartmentectomy with regional lymphadenectomy, adjuvant radiotherapy, and maintenance chemotherapy.