CLINICAL CASE
REVISTA DE LA FACULTAD DE MEDICINA HUMANA 2020 - Universidad Ricardo PalmaDOI 10.25176/RFMH.v20i3.2206
SURGICAL REPAIR OF STERNUM CHONDROSARCOMA IN A 58-YEAR-OLD MALE PATIENT: CASE REPORT
CONDROSARCOMA DE ESTERNON EN PACIENTE MASCULINO DE 58 AÑOS: REPORTE DE CASO
José Alberto González-Ramírez1,2,a, Wendy Reyna González3,b, Angel Rivera-Doroteo
3,c, Pablo Aldahir Montalvo-Ramirez3,c
1Centro Médico Nacional 20 de noviembre, Ciudad de México-México.
2Centro Médico Pensiones, Mérida-México.
3Facultad de Medicina y Cirugía, Universidad Autónoma Benito Juárez de Oaxaca, Oaxaca de Juárez-México.
aSurgical oncologist.
bMedical surgeon.
cMedical student.
Sternum chondrosarcoma is an infrequent malignant neoplasm which occurs mainly in adults over 50 years old. Grade 1 chondrosarcoma is the most frequent among the heterogenous group of tumors that fall into this classification, however, it is most frequently presented in the pelvic region, in long bones of the appendicular skeleton and in the costal region. The fact that it presents in the sternal region compromises the constitution of nearby organs. Due to radiotherapy and chemotherapy having a scarce therapeutic effect, we proceeded with surgical intervention where a wide resection of the sternal chondrosarcoma and liver metastasectomy was performed, subsequently, the chest wall was rebuilt using titanium plates and microsurgical right dorsal muscle flap. The final result was favorable. We present a conventional chondrosarcoma (grade 1) case at the xyphoid process level with liver metastasis.
Key words: Chondrosarcoma; Sternotomy; Bone neoplasms; Thoracic surgery (source: MeSH NLM).
RESUMEN
El condrosarcoma de esternón es una neoplasia maligna poco frecuente que se presenta mayormente en adultos mayores de 50 años. El condrosarcoma grado 1 es el más frecuente dentro del grupo heterogéneo de tumores que entran en esta clasificación, sin embargo, tiene una presentación más frecuente en la región pélvica, en huesos largos del esqueleto apendicular y en la región costal. El hecho de presentarse en la región esternal puede comprometer la constitución de órganos cercanos. Debido a que la radioterapia y la quimioterapia tienen un escaso efecto terapéutico se procedió con la intervención quirúrgica donde se realizó la resección amplia del condrosarcoma esternal y la metastasectomía hepática, posteriormente se reconstruyó la pared torácica mediante placas de titanio y un colgajo microquirúrgico de músculo dorsal ancho derecho. El resultado final fue favorable. Se presenta el caso de un condrosarcoma convencional (grado 1) a nivel del apéndice xifoides con metastásis a hígado.
Palabras Clave: Condrosarcoma; Esternotomía; Neoplasias óseas; Cirugía torácica (fuente: DeCS BIREME).
Chondrosarcoma is the third malignant neoplasm of chondroid and skeletal lineage, that presents more frequently in elderly adults. The central or conventional chondrosarcoma type in this case has a greater incidence in appendicular skeletal regions especially in large bones such as the femur and humerus, although it can also present itself within axial skeleton such as pelvis and costal margin. Its histological similarity with chondroma makes it a difficult diagnosis, however, in its development at the sternum level the use of magnetic resonance imaging (MRI) and computerized axial tomography (CAT) are of great importance.
CASE REPORT
Male patient of 58 years of age admitted to the hospital in 2017 presenting increase in volume at the xyphoid process, through X-rays we observed right upper external thoracic increase. The ultrasound showed a 10 cm tumor of the xyphoid process, not painful, lobulated, without visceromegalies and normal capillary refill. Patient had a maternal grandfather with prostate cancer, maternal grandmother had cervicouterine cancer, brother with renal adenocarcinoma, denies allergies and transfusions, had laparoscopic cholecystectomy in 2016. Tobacco abuse suspended since 2013 and occasional alcohol consumption.
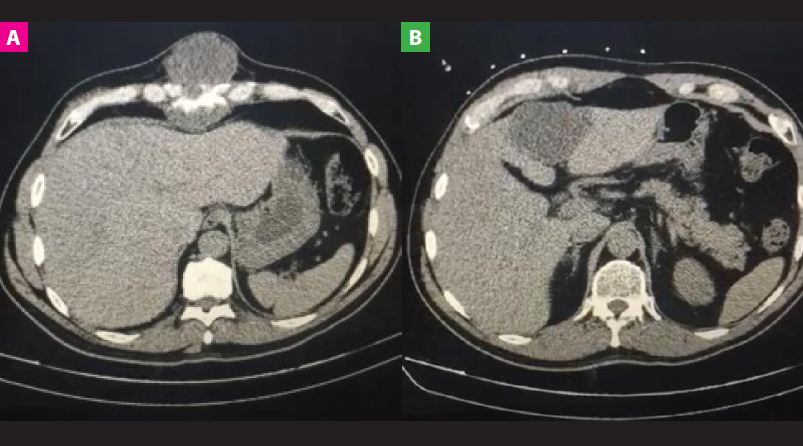
He was admitted in 2018 with a sternum chondrosarcoma diagnosis with probable metastases to the liver, a thoracic and abdominal CAT scan was done and showed a neoformative lesion in the xyphoid process ( Fig 1A), and in the liver segments II and IV (Fig 1B). Through sternum biopsy, a cartilaginous neoplasia was observed and the anatomopathological diagnosis reported low grade chondrosarcoma (grade 1).
A tomographic scan was performed for the marking and localization of the area to be biopsied through a puncture in the right costal region covered with gauze and adhesive tape. A tomographic guided biopsy was also performed in the liver for suspected metastasis.
IPatient is admitted for wide resection of sternum chondrosarcoma (Fig 2C), reconstruction of the thoracic wall with titanium plate and microsurgical right dorsal muscle flap, hepatic metastasectomy through the non-anatomical resection of segments II, III and IVa (Fig 2D) and the reconstruction of pericardial defect with Dual Proceed surgical dressing and the defect is repaired with prolene mesh, 3 titanium rods, 6 clips and omentum above.
The flap is placed over the muscle, the skin is covered with Mepitel One, Melgisorb and non-compressive bandage. It was managed with antibiotics, mainly meropenem and linezolid during hospitalization with outpatient follow-up.

Fig . Computerized axial tomography (CAT) images and surgical resection
A: Thoracic and abdominal CAT scan show a neoformative lesion at the sternum level.
B: Abdomen CAT scan shows hepatic metastasis.
C: Block resection of the sternum chondrosarcoma. D: Non-anatomical resection of hepatic segments II, III y IVa.
DISCUSSION
Chondrosarcoma is the third primary bone malignant neoplasia, 12% presents in the costal region, and is frequently between the second and fifth decades of life. 90% originates de novo and has a predominance for the male gender(1). Primary central or conventional chondrosarcoma represents approximately 20% of primary malignant bone neoplasia, with femur, pelvis, humerus and ribs being the most frequent and presenting in elderly age(2,3).
The metastatic potential of conventional chondrosarcomas is low due to its slow growth that difficults a prompt diagnosis. From the clinical and radiological point of view, its presentation in children is rare and has a predilection for the appendicular skeleton and affects lymph nodes. The factors related to a higher metastatic possibility are histological grade 3, pelvic area localization, local recurrence, size larger than 10 cm and over 60 years of age (4).
Cartilaginous sternum tumors are all malignant regardless of its histologic characteristics (1).
Chondrosarcomas are a diverse group of malignant neoplasms composed of cells of cartilaginous phenotype, which show a lobulated histological pattern that can present myxoid changes, calcification and ossification. It is a central, intramedullary, malignant cartilaginous neoplasia of greyish-blue color, hyaline aspect and nodular pattern. It may contain yellow-whitish calcified areas or cystic myxoid areas. It may have cortex erosion, cortical destruction and extend to adjacent target tissues, especially flat bones. They are hypercellular in comparison to chondromas and show a variable atypia. Grade 1 chondrosarcoma has moderate cellularity, hyperchromatic large nuclei and binucleated cells, due to its diagnostic difficulty, it is primordial to consider its localization and histological characteristics of the tumor(1).
They are of cartilaginous nature, lobulated appearance, translucid hyaline nodules similar to cartilage, and intense mineralization. It may be of myxomatous and bland consistency, in which it may present necrosis and/or hemorrhage. The presence of hemorrhagic, friable, grey tissue with sarcomatous appearance is indicative of histological high grade chondrosarcoma(4). In chondrosarcomas the tumor fills the medullary cavity and encompasses the normal medulla in trabeculae islets, they are hypercellular with moderate atypia, difficult to differentiate from chondroma. Atypia, hypercellularity and myxoid changes can also be seen normally in an enchondroma. Chondrosarcoma has neovascularization, which leads to tumoral lesion from a predominantly diffusion-dependent metabolism to a mainly perfusion-dependent one(6).
They are classified in 1,2 and 3 according to its nuclear size, stain pattern, mitotic activity and cellularity grade. Grade 1 is the most differentiated and of best prognosis (2). Primary chondrosarcomas arise from bone cells and secondary from preexisting benign cartilaginous lesions such as chondromas or the portion of an osteochondroma(3).
Within the clinical presentation can include insidious dull and intermittent pain. It can be progressive and last months or years and there is an increase in local volume (4,6).
Radiolucent lesions are present in conventional radiology, upon mineralizing they show spotted opacities due to calcification of cartilaginous nodules. Cortical destruction and soft tissue lesion are found on flat bones(1). A chondroid lineage lesion can exhibit a very versatile morphology regarding its aggressiveness. It presents poorly defined margins, endosteal erosion in more than 2/3 of its cortical thickness, cortical permeation, lobulated edges and characteristic calcified matrix(6). The presence of interior calcifications is characteristic of a cartilaginous lesion, the presence of endosteal erosion is important because these are lesions with a high grade of capturing radiopharmaceuticals
The computerized tomography allows a high sensitivity and specificity based on the criteria of cortical permeation/erosion, osteolysis/sclerosis of the mineral matrix, periosteal reaction and the topographical definition. Magnetic resonance imaging allows us to incorporate the evaluation of the bone marrow alteration, the mineralized matrix, peri pulmonary edema and the dynamic evolution of the enhancement pattern with paramagnetic contrast (6).
The imaging study of chondroid tumors guides us with respect to its aggressiveness and its biological conduct, in addition to allowing to characterize the tumoral topography and the size of the extension. The latter is the most important element to determine the prognosis and radiology is important here with a greater emphasis on magnetic resonance which possesses a greater utility level.(6).
Radiotherapy has a limited therapeutic role and chemotherapy has not shown any benefits. Oncological resection surgery is programmed removing the tumor en bloc in the thoracoabdominal area. Chondrosarcomas are considered radioresistant due to its low mitotic potential. The local recurrence rate is 4% in resected cases and 73% due to an incomplete resection(2). In surgery, we must first consider an en bloc tumor resection, always keeping free safety margins and always performing a complete thoracic cavity exploration, in addition to the resection of adjacent structures, in case it is indicated(7).
LThe intralesional resection technique along with adjuvant therapy with electrocauterization, use of phenol, and the defect can be filled with a bone graft or with methyl methacrylate. The use of surgical sponges around the tumor zone avoids dissemination and possible seeding of sarcomatous cells, in addition, the use of bone cement offers immediate stability, facilitating the postoperative radiologic evolution and eliminating residual tumoral cells through polymerization, wires and other fixation devices can be used.
The appendicular skeleton lesions possess a better diagnosis than the axial skeleton, Recurrence can occur 5 to 10 years after surgery and mainly occurs in those with higher histological grade and due to an inadequate resection(4).
LThe reconstruction of skeletal defects can be performed with a biological mesh from porcine dermis and titanium fixation. The technique is based on reestablishing the thoracic continuity in patients with tumors that must be resected for their cure. The need for a defect reconstruction has a direct relation with the zone and size of the en bloc resection, this point is important in case of partial or complete sternum excision, especially in the manubrium and when three or more ribs are removed(7),as is presented in this case.
Thoracic reconstruction can be performed safely and successfully using musculo-cutaneous flaps or prosthetic material (8). SWe performed a thoracic wall reconstruction through complete sternum extraction, then placed a biological mesh with partial or radical surgical management, which allows the eradication of tumoral cells. The reconstruction can be performed with placement of porcine dermis mesh, stabilizing the thoracic wall with a titanium sternal fixation system. The major pectoral muscle flaps are released in the midline of the body, the prosthesis is covered, and a left Blake drain is placed, the skin is attached and the Pleurovac is connected.
EAmong the materials conventionally used in thoracic reconstruction, methyl methacrylate is a good tool, situated between 2 layers of the Marlex mesh, and used as a prosthesis, allowing an adequate adaptability, resistant to infection and in posterior imaging studies, reducing vision obstruction, which can be clearly observed in tomography as in magnetic resonance imaging. The prolene mesh has been useful in keeping the thoracic wall stable and offer support to flaps in the closing of defects with wounds in an unfavorable environment(8).
The most indicated prosthetic material in reconstructions are the titanium plates that allow to adequately preserve sternum irrigation, providing a greater margin of healing assurance. The material indicated for reconstructions must be durable, adaptable and permeable to X-rays, with minimal inflammatory reactions, resistant to infection. The titanium bars present a design which can be used without removing the periosteum, which allows it to maximize blood supply to the bone (5).
LThe positive surgical margins are essential to reduce the incidence of local relapse and distant metastases. There should be a protocol regarding these tumors in order to obtain better oncological and functional results. The identification of prognostic factors and the survival knowledge of these patients are important at the moment of treatment and surgical strategy selection(3).
CONCLUSION
Magnetic resonance imaging and computerized tomography are fundamental tools in the diagnosis of chondrosarcoma, however, surgical resection with positive edges could be deemed necessary to prevent local or metastatic recurrence. Above all, the reconstruction with titanium plates has proven to be an effective technique which is continuously evolving providing a better prognosis for the patient, due to its adaptability and the practicability it presents in surgical procedure as well as in rehabilitation. Despite being a pathological presentation that has a low incidence in the population, the differential diagnosis analysis and the surgical procedure are of great utility as support for the medical professional in identical cases as well as in those where sternotomy is imminent.
Acknowledgments:We thank the Universidad Autónoma Benito Juárez de Oaxaca for providing the foundation for the drafting of this scientific article.
Author contributions: The authors participated in the genesis of the idea and the manuscript preparation of this current work.
Financing: Financing.
Conflict of interests: The authors declare no conflicto of interests.
Received: August 16, 2019
Approved:April 05, 2020
Correspondence: Wendy Reyna González.
address: Exhacienda de Aguilera SN, Camino a San Felipe del Agua, Colonia Reforma,
Oaxaca de Juárez, Oaxaca-México, CP: 68020.
Telephone numbeR: 9511865302
Email: draqueencitawen@gmail.com
BIBLIOGRAPHY