ARTÍCULO ORIGINAL
REVISTA DE LA FACULTAD DE MEDICINA HUMANA 2021 - Universidad Ricardo PalmaDOI 10.25176/RFMH.v21i2.3721
REGIONAL DISTRIBUTION OF MORTALITY BY COVID-19 IN PERU
DISTRIBUCIÓN REGIONAL DE MORTALIDAD POR COVID-19 EN PERÚ
Maria Gracia Flores López(1,a), Alonso Soto Tarazona(1,2,b), Jhony A. De La Cruz-Vargas(1,2,c)
1 Facultad de Medicina Humana. Universidad Ricardo Palma. Lima, Perú.
2 Instituto de Investigación de Ciencias Biomédicas (INICIB) Universidad Ricardo Palma. Lima, Perú.
a Internal Medicine.
b PhD in Health Sciences.
c PhD en Medicine.
Objectives: Compare the death rate from COVID-19 at the national level by regions and departments from March to September 2020. Methods: Quantitative, observational, cross-sectional, ecological and retrospective study. The data was extracted from the National Death System (SINADEF) in Microsoft Excel 2016 and imported into Stata. The variables were described as frequencies and percentages. Mortality was obtained by dividing the total deaths over the total population according to the last census. An adjusted exploratory analysis was performed using robust regression methods to evaluate the association between mortality by department and regions adjusted for age and sex of the deceased. P <0.05 was considered significant. Results: 32535 deaths were reported, 69.84% were male and the median was 67. The mortality rate in the Costa region 145 deaths were calculated (n = 24,276), followed by Sierra with 51 (n = 4434) and Selva with 63 (n = 2545). There were significant differences in mortality according to the region, in the comparison of the coast with the Sierra region a beta coefficient of -96.28 was found (p <0.001 IC -123.76 -68.77), while in the comparison with the Selva it was determined a coefficient of -50.38 (p 0.01 95% CI -91.47 -9.29). No significant association was found between the mortality rate and the average age or sex of the deceased by department. Conclusion: The death rate from COVID-19 at the national level was 101 per 100 000 inhabitants. The mortality rate found was higher on the Costa region than in the Sierra and Selva, regardless of the proportion of men, women or age.
Keywords: Mortality, Coronavirus infections, COVID-19. (Source: MeSH – NLM)
RESUMEN
Objetivos: Comparar la tasa de mortalidad por COVID-19 a nivel nacional por regiones y departamentos desde marzo a septiembre del 2020. Métodos: Estudio cuantitativo, observacional, transversal, ecológico y retrospectivo. La data fue extraída del Sistema Nacional de Defunciones (SINADEF) en Microsoft Excel 2016 y se importó a Stata. Se obtuvo la mortalidad dividiendo el total de muertes sobre la población total de acuerdo al último censo. Se utilizó frecuencias y porcentajes, se realizó un análisis exploratorio ajustado con métodos de regresión robusta para evaluar la asociación entre mortalidad por departamento y regiones ajustado a edad y sexo. Se consideró significativo p< 0.05. Resultados: Se reportaron 32535 fallecidos, el 69.84% fueron varones y la mediana de edad fue 67. La mortalidad por mil habitantes, en la región Costa se calculó en 145 muertes (n=24276), seguido de Sierra con 51 (n=4434) y Selva con 63 (n=2545). Existieron diferencias significativas de mortalidad de acuerdo a la región, en la comparación de la costa con la sierra se halló un coeficiente beta de -96.28 (p <0.001 IC -123.76 -68.77), mientras que en la comparación con la selva se determinó un coeficiente de -50.38 (p 0.01 IC 95% -91.47 -9.29). No se encontró asociación significativa entre la mortalidad y la edad o el sexo de los fallecidos por departamento. Conclusión: La tasa de mortalidad por COVID-19 en Perú fue de 101 por 100000 habitantes, fue mayor en la costa que en la sierra y la selva independientemente de la proporción de varones, mujeres o la edad.
Palabras Claves: Mortalidad, Infecciones por coronavirus, COVID-19. (Fuente: DeCS - BIREME).
Currently, COVID-19 is considered a public-health problem. In December 2019, it was reported that a number of patients in China showed a severe acute respiratory syndrome caused by the new coronavirus and it was categorized as a pandemic on March 11th of the same year.(1) In spite of the diffusion of contagion prevention measures such as physical distance, usage of masks and hand washing, according to WHO (World-wide Organization of the Health), until September 2020 just 1 million people passed away at a world-wide level due to infection caused by the respiratory pathogen.(2) The disease has a high impact on mortality and morbidity because the later sequelae of the acute condition on people who manage to overcome the affection are unknown, but they could cause disability, alterations in functionality and connection to the social environment.(3)
COVID-19 arrived in Peru in a more delayed form in comparison with European countries. The first confirmed case was declared on March 6, and from there multiple measures were taken such as the establishment of a sanitary emergency situation, obligatory total immobilization, promotion of hygiene measures and closure of borders and airports. In spite of everything, the Ministry of Health (MINSA) registered around 780 000 confirmed cases until September.(4)
Due to the alarming amount of infected people and the high mortality in Peru in comparison with other countries, both developed and developing ones, e.g., in Latin America, Prieto Silva et al. made a comparison between Colombia, Chile and Argentina. Until the end of July the greatest number of deaths was found in Colombia with 10711(5), whereas in Peru at the same time, there were already 19614 deaths and its lethality was 4,5% superior to the continental average of 3,9%(6). For this reason, the comparison of mortality in different regions of this country is relevant, bearing in mind the multiple influential factors it presents such as microclimates, geographical contrast, the explosion of social conflicts that facilitates the agglomeration, different preponderant types of industry in every region and a high biodiversity that cause a variable impact of the virus in the population. Also, some studies indicate there is a difference in the deceases related to altitude.(7)
Without a specific treatment and in the absence of a vaccine that can be massively applied in Peru, it’s likely that a second wave of contagions will appear, just like it already has in other latitudes, and it could be as lethal as the first one. It is important to know the epidemiologic differences between regions to recognize the zones of vulnerability with respect to COVID-19, which according to Friston et al. it is also necessary to find the correct epidemiologic model, estimate its magnitude(8) and consequently, optimize the alertness, improve the decision-making and offer a better sanitary response.
Due to all the reasons given above, the objective of this investigation was to compare the rate of mortality by COVID-19 at national level, by region and by department between March and September 2020.
METHODS
Design and study area
A quantitative, analytical, observational, cross-sectional, ecological and retrospective study was made in the context of the national sanitary emergency of COVID-19.
Population and sample
All the patients that passed away in Peruvian territory due to COVID-19 infection between March and September 2020 that were found on the free access secondary data source, collected and updated by the SINADEF (National System of deaths in Peru) in Microsoft Excel 2016 format, available in: https://www.datosabiertos.gob.pe/dataset/fallecidos-por-covid-19-ministerio-de-salud-minsa. There were 32535 deceased people that fulfilled the requirements so this was the definitive population.
Procedures and variables
Mortality by COVID-19 was considered as the dependent variable, whereas the independent variables were sex, age and region of death for every person. The conceptual definition of region of death contemplates Costa, Sierra and Selva, where Costa includes the departments located in the Peruvian coast, Sierra includes the departments located in the mountainous zone of The Andes with great altitude (greater to 1500 masl) and Selva includes the departments of the Amazon river, with low to moderate altitude (smaller to 1500 masl).
Statistical Analysis
The Stata program was used, where the numerical variables were described as averages and standard deviations, whereas the categorical variables were expressed as frequencies and percentages. The rate of mortality was obtained by dividing the total amount of deaths by region or department by the total population, according to the published data of the last national census provided by the INEI (National Institute of Statistic), available in: http://censo2017.inei.gob.pe/resultados-definitivos-de-los-censos-nacionales-2017/.
The death rate between regions was compared using the test of Kruskall Wallis. Then the relation between the region mortality and the gender of the deceased people was compared using the test of Mann-Whitney. Subsequently, in order to evaluate the relation of the numerical variables for the department with the valuations of mortality, the Spearman's rank correlation coefficient was used. Lastly, an adjusted exploratory analysis was performed using methods of robust regression in order to evaluate the relation between mortality by department and region adjusted to the age and sex of the deceased. A value of p < 0.05 was considered significant.
Ethical aspects
The public information base does not collect personal information. The study was registered with the Instituto de Investigación en Ciencias Biomédicas (INICIB) and approved by the committee of ethics of the Universidad Ricardo Palma.
RESULTS
During the period from March to September 2020, 32535 deaths occurred that fulfilled the inclusion criteria. 69,8% (n=22722) of deaths were men and 30,1% (n= 9813) were women, the median and average age were 67,00 and 65,89 respectively, with an interquartile range from 57 to 76 years (25%-75%). In addition, it was observed that the youngest deceased person was 27 years old and the eldest one was 108 years old.
Graphic 1 shows the number of deceased people during the 28 analyzed weeks: the distribution fluctuates between 0.04% (n 14) and 6.2% (n 2031) on the first and twelfth week respectively, being the latter one the biggest peak registered.
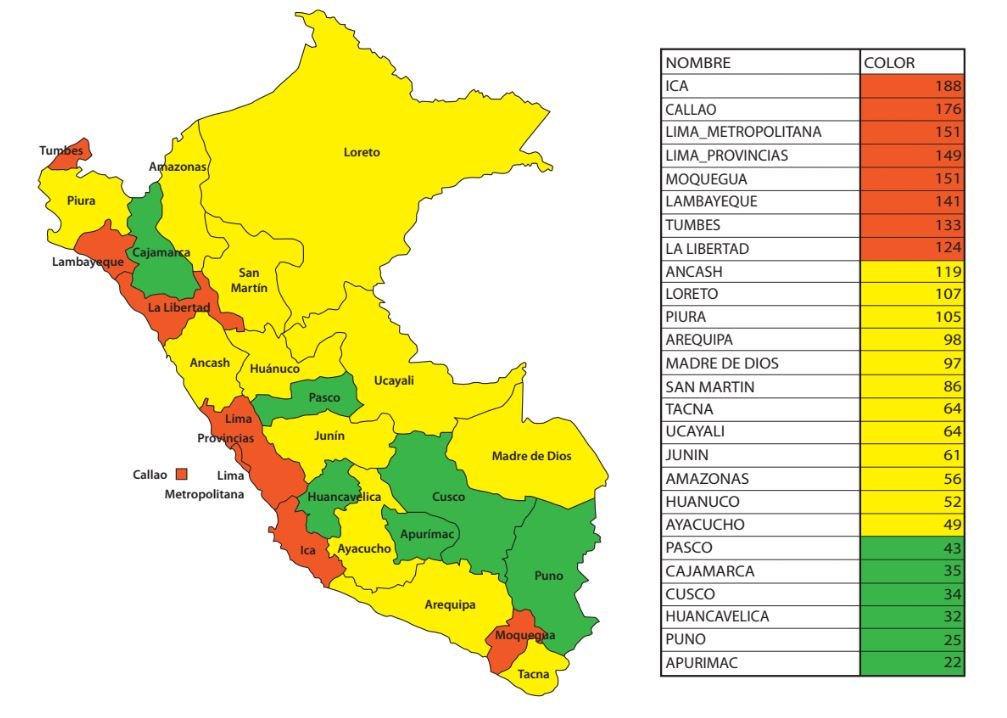
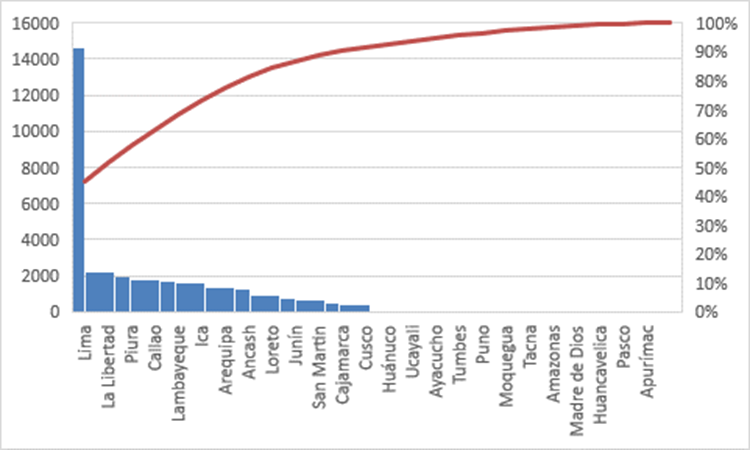
Graphic 2shows the death rate in each department for every 100000 inhabitants, indicating that the biggest one is located on Ica with 188 deaths, followed by Callao with 176 and Lima in 170. The lowest mortality was found in Apurímac with 22 and Puno with 25 deaths per 100000 inhabitants. The highest number of deaths was registered in Lima with more than 14000 deceased, followed by La Libertad, Piura, Callao and Lambayeque (graphic 3).
The average age by department was 65,47 years with a standard deviation of 1,80 and a coefficient of variation of 2,7%. This value was smaller in Ucayali with an average of 60,94 and greater in Ayacucho with an average of 68,10.
Regarding sex, the average of men by department was 69% with a standard deviation of 4% and a coefficient of variation of 5,8% was found in 0.04 and 0.05%.
The average mortality by department was 89 per 100000 inhabitants, with a standard deviation of 50 and a coefficient of variation of 56.
Table 1 summarizes the data of the deceased and the population of each region. Results show that the median death rate by province in Costa was about 129,56 by 100000 inhabitants, with an interquartile range from 90 to 162. The Sierra region got a median death rate of 35,22 by each 100000 inhabitants, with an interquartile range from 15 to 43. Finally, the Selva region got a median of 51,45 by each 100 000 inhabitants, with an interquartile range from 24 to 68.
Table 1. Percentage and mortality rate according to region.
|
Region |
Deaths |
Population/strong> |
Mortality rate per 100000 inhabitants |
|
Costa |
24276 |
16660544 |
145 |
|
Sierra |
4434 |
8661877 |
51 |
|
Selva |
2545 |
4010456 |
63 |
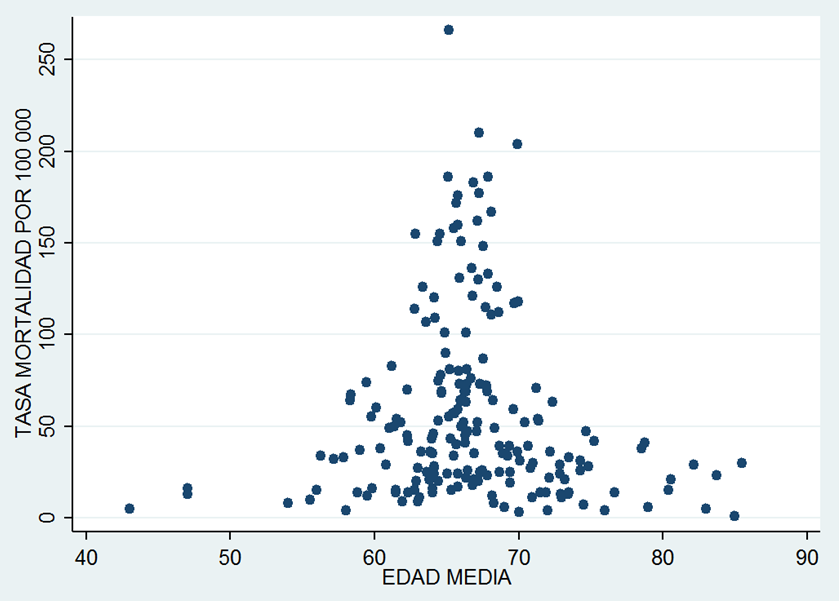
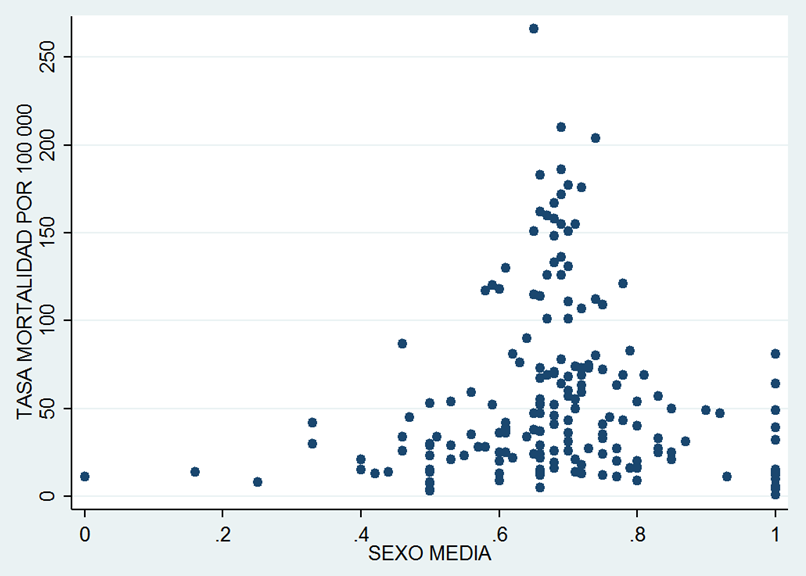
On the other hand, the relation between the age of the deceased and the rates of mortality was evaluated using the Spearman's rank correlation coefficient, obtaining a nonsignificant value of rho (rho= -0.01; p= 0,93). Also, no significant relation was found with respect to sex, expressed as a percentage of men (rho = -0.15; p = 0.47). Graphic 4 and graphic 5 show the dispersion diagrams associated.
Finally, a robust linear regression was performed and (table 2) shows the rate of mortality adjusted to sex and age by using the Costa region as reference. Even though significant differences in mortality by region existed, neither the age nor the sex of the deceased contributed to mortality.
Table 2. Robust linear regression exploratory model of mortality by region adjusted for age and sex of the deceased.
|
Mortality rate per 100000 habitants |
Beta coefficient |
Standard error |
p value |
IC 95% |
|
|
Sierra* |
-96.28 |
13.18 |
<0.001 |
-123.79 |
-68.77 |
|
Selva* |
-50.38 |
19.69 |
0.01 |
-91.47 |
-9.29 |
|
Age |
-0.01 |
0.02 |
0.72 |
-0.06 |
0.04 |
|
Percentage of deceased males |
-0.90 |
1.40 |
0.52 |
-3.83 |
2.03 |
DISCUSSION
During the first 28 weeks of the sanitary emergency in Peru, a global rate of mortality of 101 by 100000 inhabitants was registered. Huamaní’s work(9) indicates that Chile and Peru lead with more than 270 by million, but the study only considers deaths until June.
With respect to the sex variable, it was obtained that most of the deaths occurred in men (69,84%). This coincides with Di Stadio et al.(10), who indicated that the greatest number of deceased men by COVID-19 was in a proportion from 3 to 1 over women. However, Xiaochen et al.(11) indicated that 50,9% of the deceased in a hospital of Wuhan were men, a much smaller difference than the one previously described. Casas Rojo et al.(12) described a prevalence of women, only when the age was superior to 90 years.
With respect to the age variable, the median was consistently greater than 60 years. Muñoz Torres et al.(13) reported a greater mortality on people older than 80 in Mexico, a country with sociodemographic characteristics similar to Peru. Moreover, in Spain, Casas Rojo et al.(12) obtained that the median was of 69,4 where 58,4% of the total of population was constituted by the age group of people older than 65 years.
With respect to the greatest number of deceased by department it must be emphasized that they belong to the coastal region, being one of the most inhabited in Peru, whereas the lowest number of deaths were in Apurímac. This is compatible with the conclusion of Bezerra Sousa et al.(14) who indicated that the metropolis cities of Brazil are the ones that show a wide increase in relation to the number of cases.
The highest death rate was found in Ica, then Callao and Lima. By contrast, the lowest rate of mortality was in Apurímac. Regarding Ica as the most affected department, the last census(15) of 2017 shows a reduction of natality in this department during the past few years, that is to say, an increase of the population older than 30 years. That epidemiologic transition could partly explain this situation. In addition to that, it is shown that a 5% are afro-descendant, although it is a variable that is not evaluated in the present study, it is a relatively large sector and according to Williamson et al.(16), this characteristic is associated with a greater possibility of death. Coupled with that, it must be considered that it is an eminently agro-industrial department which could have reduced the probability of isolation among the workers. Another point are the comorbidities like risk factors associated to this group of the population. INEI (National Institute of Statistic and Computer science) reported that Ica is one of the departments with the greatest load of nontransmissible diseases, with almost 40% in general, and it’s superior to the average of Peru with 39,4%. By contrast, Ica and Lima are the departments with the smallest number of unmet basic needs and situation of low poverty compared to other departaments(17). However, for the smaller mortality on the Sierra and Selva, Accinelli et al.(18) analyzed that the increase of 500 meters over the sea level diminishes the rate of cases by 22% and the deaths by 40%, attributing this difference to the hypobaric hypoxia and to the physiological adaptations that it would generate.
On the other hand, no significant relation between age and mortality was found. This coincides with Fernández Niño et al.(19) who evaluated Colombian data and concluded that age is not associated to many mortality patterns since not every comorbidity increases with the age group and these are decisive variables in the disease evolution. No association between the death rate and the sex of the deceased was found either, most likely due to the multiple racial differences of every studied region, among other factors like coexisting pathologies.
Our study found significant differences in mortality by regions. Living in the Costa is a risk factor for greater mortality, followed by the Selva and then the Sierra. This agrees with the study of Matiram Pun et al.(20) where several factors are mentioned like the induced hypoxia of high altitude that can diminish the expression of angiotensin 2 converting enzyme receptor, as well as the high levels of radiation and their relation with superior vitamin D concentrations that would show antiviral benefits. Another cause is the agglomeration and consequent population density in regions with cities more urban than rural. The work of García de León(21) refers to the greater possibility of death by COVID-19 to a greater development situation of the region, as well as the relation between the urban population and the number of deaths, which is compatible with our result. On the other hand, Ypanaqué and Martins(22) analyzed the geographical and accessibility aspects in relation to the sanitary attention, with which they showed that the Costa region, excluding Lima Metropolitana, was constituted as the first region without health insurance with 26,6% of its population. This could also contribute to the lack of access to diagnostic tests.
The limitations of the study are mainly the possible subregister of the deaths reported by SINADEF, substantially smaller to those of the INEI. Before the arrival of the disease, it only registered 75% of deaths, and the situation worsened in some departments like Amazonas, Pasco, Cajamarca and Loreto(23). Another relevant point is the excess of deaths. The Economist(24) reports that during one of the worse peaks in mortality, there were 3,7 reported deaths per 100000 people whereas the excess for the same date was of 12 deceased. Also, some data was incomplete and it would have been important to consider how people were diagnosed or if they suffered of comorbidities that could trigger the outcome. Because of that, social, geographic and climatologic determinants of the Peruvian territory that would influence the observed difference of mortality by COVID-19 by regions must be explored. Conducting studies considering associated variables like poverty, sanitation, race and population density must be encouraged. It is also important to count with more exhaustive data of deaths that includes additional information like diagnosis method or preexisting clinical conditions and finally emphasize control, active search of cases and opportune hospitalization in coastal departments where the greatest frequency of mortality have appeared.
CONCLUSION
The rate of mortality in all Peru was of 101 by 100000 inhabitants until September of 2020 and significant differences between the rate of mortality by regions exist, where the Costa region displayed the greatest mortality, followed by Selva and finally Sierra. It was identified that the greatest number of deceased were men older than 60 years and no differences in the rate of mortality by department in relation to the sex or age of the deceased were found.
Authorship Contributions: The authors participated in the generation, writing and final approval of the original article, as well as in data collection.
Financing: The research was self-financed.
Conflicts of interest: There were no conflicts of interest.
Received: January 30, 2021.
Approved: February 25, 2021.
Correspondence: Maria Gracia Flores López.
Adress: Jirón Villarreal, urbanización Sima #192 La Perla.
Phone: 968 292 762
E-mail: mariagraciaflores97@hotmail.com
BIBLIOGRAPHIC REFERENCES