CLINICAL CASE
REVISTA DE LA FACULTAD DE MEDICINA HUMANA 2024 - Universidad Ricardo Palma10.25176/RFMH.v24i1.6468
TOXIC MEGACOLON. CASE REPORT
MEGACOLON TÓXICO: A PROPÓSITO DE UN CASO
Roger Sernaque Mechato
 1,2,a,b
1,2,a,b
Stephanie Tahnne Castillo Arias
 1,c
1,c
Silvana Ñaupari Jara
 1,d
1,d
Flor Milagros Mendoza Barreto
 1,e
1,e
1 Hospital Santa Rosa Lima Perú
2 Universidad Continental
a Medical internist
b Head of the Department of Medicine
c Gastroenterologist
d Family and Community Physician
e Master in Public Health
ABSTRACT
Toxic megacolon is a fatal disease, most commonly occurring as a complication of inflammatory bowel
disease, infections, and intestinal ischemia. It is characterized by the presence of bloody diarrhea,
abdominal distension, signs of systemic toxicity, and segmental colonic dilation is observed in imaging
studies. For the diagnosis, according to the Jalan criteria, colonic dilation of more than 6 cm is taken
into account, three of the following: fever, tachycardia, leukocytosis or anemia, and any of the
following criteria: hypotension, hypovolemia, electrolyte disorder and altered mental status. This
article presents the case of a female patient who was admitted with abdominal pain and chronic diarrhea
with an imaging study showing dilation of the entire colonic framework. The corresponding studies were
carried out which indicated that she had a toxic megacolon due to colitis. ulcerative, receives medical
treatment with favorable evolution, is discharged and readmitted for septic shock, studies are performed
and Clostridium difficile infection is identified, antibiotic treatment is started but the evolution is
unfavorable, which caused the death of the patient. The present case represents the high mortality of
this disease.
Keywords: Toxic megacolon, ulcerative colitis, Clostridium difficile, shock (source: MeSH – NLM)
RESUMEN
El megacolon tóxico es una enfermedad mortal, que se presenta, con mayor frecuencia, como una
complicación de la inflamación intestinal, infecciones e isquemia intestinal. Se caracteriza por la
presencia de diarrea sanguinolenta, distensión abdominal, signos de toxicidad sistémica y, en estudios
de imagen, se observa dilatación colónica segmentaria. Para el diagnóstico, según los criterios de
Jalan, se tiene en cuenta la dilatación colónica más de 6 cm, tres de los siguientes: fiebre,
taquicardia, leucocitosis o anemia, y cualquiera de los siguientes criterios: hipotensión, hipovolemia,
trastorno electrolítico y estado mental alterado. En este artículo, se presenta el caso de una paciente
mujer que ingresa por cuadro de dolor abdominal y diarrea crónica con estudio de imagen, en la que se
visualiza dilatación de todo el marco colónico. Se realizan los estudios correspondientes y se
diagnostica megacolon tóxico por colitis ulcerativa, por lo que recibe tratamiento médico con evolución
favorable. Es dado de alta y reingresa por shock séptico, se realizan estudios y se identifica infección
por Clostridium difficile. Se inicia tratamiento antibiótico, pero presenta evolución desfavorable, lo
que ocasionó el fallecimiento de la paciente. El presente caso representa la alta mortalidad de esta
enfermedad.
Palabras clave: Megacolon tóxico, colitis ulcerativa, Clostridium difficile, shock (fuente: DeCS
- BIREME)
INTRODUCTION
Toxic megacolon was first described in 1930 as colonic dilation associated with sepsis, but in 1950
Marshak defined it as segmental or total colonic distention greater than 6 cm concomitant with acute
colitis and systemic symptoms(1).
The term "toxic megacolon" implies a rare but severe and life-threatening complication of inflammation
of the colon; it is characterized by total or segmental colonic distension greater than 6 cm, which is
not caused by obstruction or other types of colonic dilation such as Ogilvie syndrome or Hirschsprung
disease, associated with signs of systemic toxicity and inflammatory, ischemic or infectious etiology of
the colon (2 - 4).
The most common cause of toxic Megacolon was inflammatory bowel disease (51.6%), followed by septicemia
(10.2%) and intestinal infections (4.1%). Some studies report that in inflammatory bowel disease, the
incidence is higher in patients with ulcerative colitis (UC) by 8-10%, compared to Crohn's disease (CD)
with 2.3%. Among the infectious causes, the most common is Clostridium difficile infection(5).
The diagnosis of toxic megacolon according to Jalan et al includes: (a) radiographic evidence of colonic
dilation of more than 6 cm, especially in the transverse colon; (b) three of the following: fever (>
38.6 °C), tachycardia (> 120 beats/min), leukocytosis (> 10.5 × 103/μl), or anemia; and (c) any of the
following: hypotension, hypovolemia, altered mental status, or electrolyte disorders(6).
Common nonspecific laboratory abnormalities associated with toxic megacolon include leukocytosis with
prominent neutrophilia, especially in cases of C. difficile colitis, anemia due to gastrointestinal
blood loss, metabolic alkalosis secondary to volume depletion, hypokalemia, hypoalbuminemia, and
elevated inflammatory markers, including Sedimentation rate and C Reactive Protein(7).
The main objective of treatment is to reduce inflammation, improve colonic motility, and prevent colonic
perforation. It begins with hydration, management of hydroelectrolyte disorders, antibiotic therapy, and
treating the cause of the toxic megacolon. Indications for surgery are colonic perforation, necrosis or
total ischemia, abdominal compartment syndrome, clinical signs of peritonitis, and organ failure(7).
The aim of this article is to present a case of rare toxic megacolon at the Hospital Santa Rosa.
CASE PRESENTATION
A 64-year-old female patient from Lima with a history of hypothyroidism, osteoporosis, and depression
with regular medication of levothyroxine 0.1 mg per day. She was admitted as an emergency due to a
clinical condition lasting more than 2 months, characterized by liquid stools without mucus without
blood (4 times a day), with diffuse abdominal pain. Four days before admission, he presented nausea,
vomiting with abdominal distention, early fullness and fever.
Vital functions on admission: BP: 110/70, HR: 85 beats per minute, RR: 18, T: 37°C, STO2: 98%.
On physical examination: in poor general condition, hydration and nutrition. Abdomen: distended, soft,
depressible, increased fluid sounds, diffuse tenderness, no visceromegaly palpable. An abdominal
ultrasound was performed where signs of colitis associated with an inflammatory process in the left
iliac fossa and free fluid in the 38cc cavity were observed. Hydropic vesicle. Moderate diffuse hepatic
steatosis.
Patient with medical management presents unfavorable evolution and increased pain and abdominal
distension. An abdominal tomography was performed: diffuse concentric parietal thickening of up to 5 mm
from the cecum to the sigmoid/rectum, with marked adjacent fatty striation, as well as loss of the usual
haustra. Likewise, the presence of parietal fat density is observed at the level of the cecum and
ileocecal valve. The caliber reaches 42 mm, with some hydro-aerial levels. Omental fat streaks. Little
free fluid at the perihepatic level, in the parietocolic gutters and in the pelvis (fig. 1). Suggestive
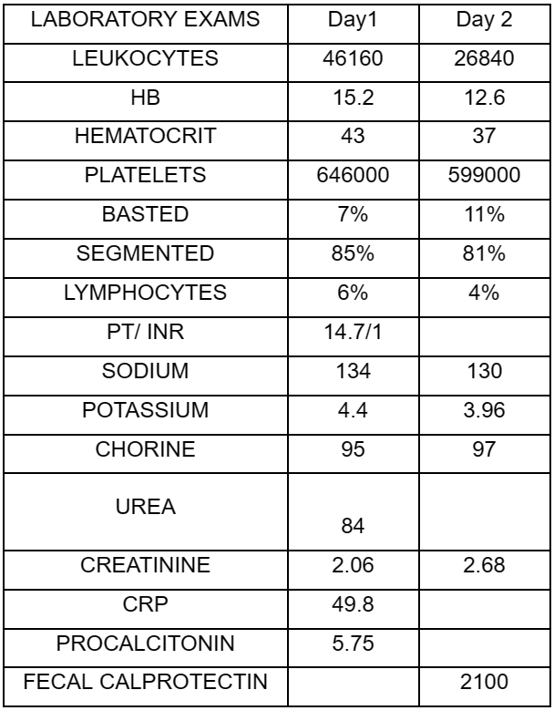
of toxic megacolon. Auxiliary examinations are requested (Table 1).
According to imaging and laboratory results (Table 1), the diagnosis of toxic megacolon is confirmed.
Patient receives antibiotic treatment with meropenem, intravenous hydration and due to high suspicion of
inflammatory bowel disease, especially ulcerative colitis, it is decided to start intravenous
corticosteroid therapy: hydrocortisone 100 mg every 8 hours. After 2 weeks of evolution, the patient
showed clinical improvement, decreased liquid stools and oral tolerance. Medical discharge with oral
corticosteroids and azathioprine is indicated.
Patient returned after 7 days due to increased frequency of liquid stools and disorder of consciousness,
entering the trauma shock unit with blood pressure: 70/40, heart rate: 140 beats per minute, STO2: 95%.
She is stabilized, evaluated by gastroenterology, who requests toxin dosage for Clostridium difficile,
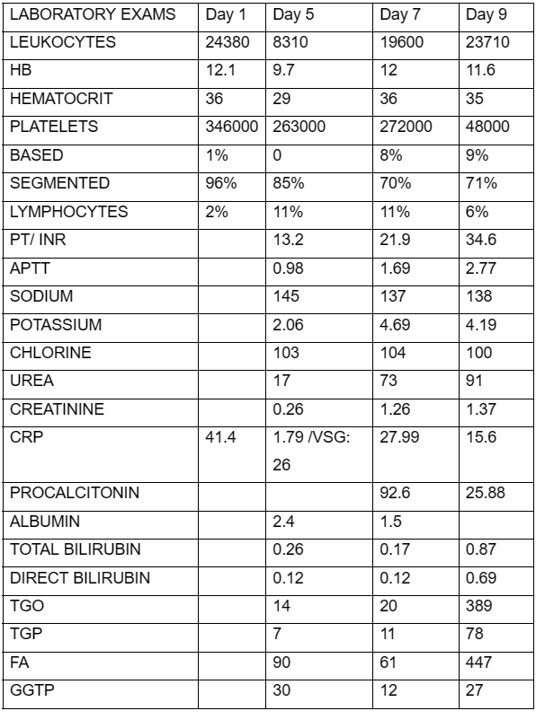
stool culture and, depending on the evolution, the possibility of video colonoscopy. Table 2 details the
laboratory tests.
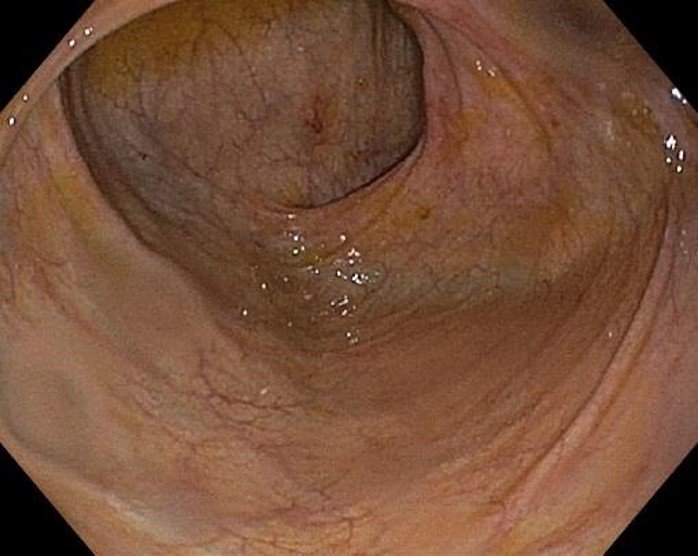
Stable patient with evident clinical improvement. A complete colonoscopy is performed where all segments
of the colon are visualized: mucosa with erythema and areas of slight friability, preserved vascular
pattern, dilation of the lumen and decrease in haustra, colonic decompression is performed and a biopsy
is taken of all segments. Rectum: slightly friable erythematous congestive mucosa with erosions,
biopsies are taken. The procedure ends without complications.
Colonoscopy (Figure 2) showed pancolitis and proctitis suggestive of ulcerative colitis, as well as
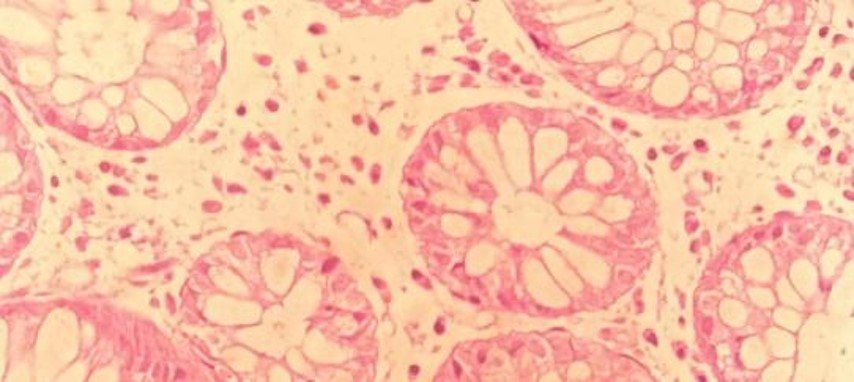
small external hemorrhoids. Regarding the biopsy, the report indicated moderate non-active chronic
colitis, absence of intraepithelial lymphocytes and presence of lymphoid accumulations in the lamina
propria without alteration in the colonic architecture and a mild non-active chronic proctitis. After
analyzing the results of the auxiliary examinations, the definitive diagnosis of ulcerative colitis
causing toxic megacolon was made.
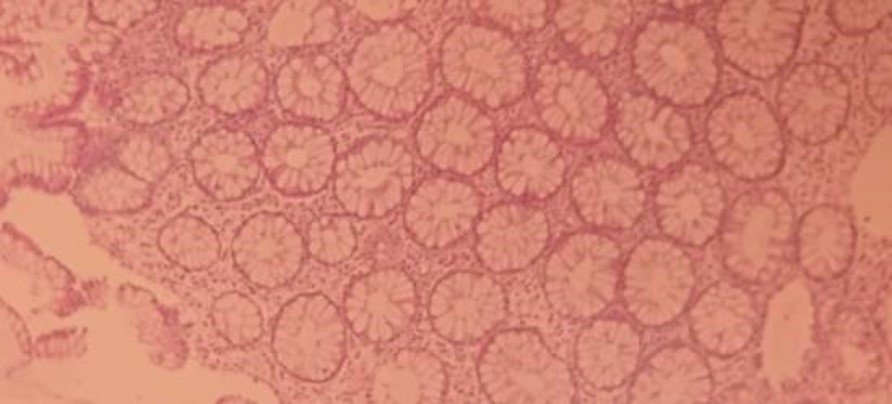
Pathological anatomy result: Non-active moderate degree chronic colitis, absence of intraepithelial lymphocytes, presence of lymphoid accumulations in the lamina propria, no architectural alteration is observed. Chronic proctitis, mild non-active degree (Figure 3).
Clostridium difficile toxin result was positive, vancomycin + metronidazole was indicated,
intravenously, monitored in the intensive care unit. The patient had an unfavorable evolution and died
from septic shock on the 9th day of hospitalization.
DISCUSSION
Toxic megacolon is a potentially fatal disease, it occurs as a complication of inflammatory bowel
disease, specifically ulcerative colitis and, less frequently CD(5, 9). However, there are other
etiological factors of both inflammatory and infectious causes; such as bacterial colitis due to C.
difficile, Salmonella(10), Shigella(11) and
Campylobacter(12) as well as viral infections due to
cytomegalovirus and parasitic infections due to Entamoeba. Other etiological factors include ischemic
colitis, Behçet's disease, and malignant diseases such as colon lymphoma and Kaposi's sarcoma.
In a recent retrospective study by Ausch et al, over a 20-year period, 70 patients with surgically
treated toxic megacolon were identified, of which ulcerative colitis was identified as the main cause of
disease (46%), followed by colitis. infectious (34%) and ischemic colitis (11%); One case (2%) of toxic
megacolon complicating CD was documented(13). According to Magallanes et
al, in their retrospective
observational study, ulcerative colitis and pseudomembranous colitis were presented as the cause in
30.8% each, followed by neutropenic colitis in 23.1% and Crohn's disease represented only 7.7%(15)
Our patient had endoscopic and laboratory criteria corresponding to ulcerative colitis that was
complicated by toxic megacolon due to clostridium difficile infection. Among the risk factors that
increase mortality according to the study by Greenstein et al(14), are
female sex, age over 40 years,
hypoalbuminemia, acidosis and high blood urea nitrogen levels, like Doshi et al(4) where agrees that
female sex, white race, average age of 60 years, coagulopathy, iron deficiency anemia and renal failure
are strong predictors of in-hospital mortality. All of the aforementioned risk factors were present in
the patient, such as age over 40 years, female sex, hypoalbuminemia and acidosis, which caused a torpid
evolution.
The clinical characteristics of toxic megacolon are intense bloody diarrhea associated with hypotension,
tachycardia, fever, diffuse abdominal pain with distention, and decreased bowel sounds(7).
The presented case met the following diagnostic criteria for TM include (a) radiographic evidence of
colonic dilation of more than 6 cm, especially in the transverse colon; (b) three of the following:
fever (> 38.6 °C), tachycardia (> 120 beats/min), leukocytosis (> 10.5 × 103/μl), or anemia; and (c) any
of the following: hypotension, hypovolemia, altered mental status, or electrolyte disorders.(7)
Abdominal X-ray images allow evaluation of colonic dilation plus 6cm of the transverse colon, air-fluid
levels, absent/distorted colonic haustral pattern. Contrast-enhanced computed tomography evaluates the
extent of involvement (submucosal edema of the colon, pseudopolyps, haustral pattern, dilation),
adjacent inflammation (mesenteric fat), and other associated features (ascites, abscesses, small bowel
involvement) that is, it can better identify complications of toxic megacolon and facilitate subsequent
treatment, there are no specific characteristics that suggest the underlying cause (8)
An endoscopic study has a high risk, especially if a complete colonoscopy is to be performed, because it
can cause perforation of the colon. If the cause is not clear, proctoscopy or sigmoidoscopy can be
performed without bowel preparation, it is safer compared to complete colonoscopy. It is useful to
diagnose inflammatory bowel disease or infection. During the procedure, air should not be insufflated
and as much air as possible should be aspirated to achieve temporary decompression. Only a few biopsies
should be taken(4).
The treatment of toxic megacolon is multidisciplinary, general measures include fluid replacement,
correction of hydroelectrolyte imbalance, particularly hypokalemia, which aggravates colonic
dysmotility, colonic decompression, administration of antibiotics decreases bacterial translocation,
antibiotics should be included in against gram-negative intestinal germs, enterococci. Early enteral
nutrition if the patient shows signs of clinical improvement to promote intestinal motility and treat
the cause of toxic megacolon(4, 7, 16)
Timely medical treatment reduces the need for surgical management by 50%; However, surgical intervention
may be necessary in up to 80% of patients, mainly if the cause is secondary to C. difficile.(16) It has
been reported that patients who survive an episode of toxic megacolon, after responding to treatment
doctor have a poor survival prognosis of six to twelve months; They may present recurrence in more than
18% and recurrence may require colectomy(17).
Indications for surgical management are progressive colonic dilation, peritonitis, perforation, bleeding
or deterioration of clinical status or lack of response within 48-72 hours despite appropriate medical
treatment. Subtotal colectomy, according to a series of studies, has a long-term success rate of 71.1%,
while segmental resection has a 48.4% success rate(4, 18).
In Magallon's observational study, they had 13
patients with toxic megacolon, of which 11 patients (84.6%) underwent subtotal colectomy with terminal
ileostomy and mortality was 61.5%, which corresponds to 8 of 13 patients(15).
In the case presented, it is important to emphasize that it is one of the first cases reported in our
Institution, where the patient presented the clinical, laboratory and imaging characteristics of toxic
megacolon with clinical evolution favorable to initial medical management and corticosteroids since
ulcerative colitis was considered. As a cause, he is discharged and re-admitted in septic shock. Taking
into account the use of broad-spectrum antibiotics, it is decided to request studies for Clostridium
difficile, which come back positive, he receives antibiotic treatment, however, he has an unfavorable
clinical evolution. which does not allow surgical management to be considered due to the patient's
torpid evolution. During the patient's second hospitalization, the high mortality rate due to the
recurrence of toxic megacolon was not considered, which could be considered indicative of surgical
management.
CONCLUSIONS
Toxic megacolon is a disease with high mortality that is characterized by bloody diarrhea associated
with abdominal distension, signs of systemic toxicity, and in imaging studies the characteristic feature
is colonic dilation of more than 6 cm. It is important to diagnose in a timely manner and initiate
medical treatment to reduce the morbidity and mortality of these patients.
Authorship contributions:
The authors participated in the conceptualization, research, methodology, resources and
writing of the original draft.
Financing:
Self-financed
Declaration of conflict of interest:
The authors declare that they have no conflict of interest.
Recevied:
November 14, 2023
Approved:
March 2, 2024
Correspondence author:
Roger Antonio Sernaque Mechato
Address:
Av. Simón Bolívar, cuadra 8 s/n. Pueblo Libre
Phone:
998995740
E-mail:
internistagg@gmail.com
Article published by the Journal of the faculty of Human Medicine of the Ricardo Palma University. It is an open access article, distributed under the terms of the Creatvie Commons license: Creative Commons Attribution 4.0 International, CC BY 4.0 (https://creativecommons.org/licenses/by/1.0/), that allows non-commercial use, distribution and reproduction in any medium, provided that the original work is duly cited. For commercial use, please contact revista.medicina@urp.edu.pe.