ORIGINAL ARTICLE
10.25176/RFMH.v25i4.6754
Epidemiological surveillance of dengue during the COVID-19 pandemic in the Lambayeque Region, Peru (2019–2020)
Vigilancia epidemiológica del dengue durante la pandemia por COVID-19 en la región Lambayeque, Perú (2019–2020)
1Hospital Regional de Lambayeque. Lambayeque, Peru.
2Health Technology Assessment Center, Instituto Nacional de Salud. Lima, Peru.
3Universidad Católica Santo Toribio De Mogrovejo. Chiclayo, Peru.
4Ministry of Health. Lima, Peru.
ᵃ MD, Radiology resident
ᵇ MD
c MD, Epidemiologist
ABSTRACT
Introduction: Dengue is a public health problem Objectives: To analyze the notification and investigation times of dengue cases and their relationship with the COVID-19 pandemic. Methods: : A cross-sectional descriptive study based on complete records from Noti.SP and SISCOVID in Lambayeque (2019–2020). Dengue surveillance times before and during the pandemic were compared, as well as their association with COVID-19 cases, using the Mann–Whitney test and Spearman correlation. Results: Between 2019 and 2020, a total of 1,598 dengue cases were reported in Chiclayo, Lambayeque, and Ferreñafe, with the highest number in 2019 (957 cases). In 2020, cases dropped to 641, with Ferreñafe showing a significant decrease from 784 to eight cases. A total of 78.8% were confirmed, and severe cases increased from one to thirteen. The median notification time increased in Chiclayo (from four to six days) and Ferreñafe (from four to 8.5 days), with no significant change in Lambayeque (p = 0.398). Investigation time also increased during the pandemic, especially in Ferreñafe (from two to 6.5 days), while it slightly decreased in Lambayeque. A positive and significant correlation was found between delayed dengue notification and COVID-19 cases (p = 0.042), and no district reached an optimal notification time, either before or during the pandemic. Conclusion: The COVID-19 pandemic negatively affected dengue surveillance, increasing notification and investigation times and causing geographical changes in case distribution.
Keywords:
Oral health, dental caries, morbidity, observational study, Peru (Source: MeSH NLM).
RESUMEN
Introducción: El: El dengue es un problema sanitario Objetivos: Determinar el tratamiento farmacológico y otros factores asociados a EHGNA en pacientes con DMT2 Métodos: Estudio descriptivo transversal basado en registros completos de noti.sp y SISCOVID en Lambayeque (2019–2020). Se compararon los tiempos de vigilancia del dengue antes y durante la pandemia, y su relación con casos de COVID-19, usando pruebas de Mann-Whitney y correlación de Spearman Resultados: : Entre 2019 y 2020 se notificaron 1 598 casos de dengue en Chiclayo, Lambayeque y Ferreñafe, con mayor número en 2019 (957 casos). En 2020, los casos se redujeron a 641, destacando Ferreñafe con una caída de 784 a ocho casos. El 78,8% fueron confirmados y los casos graves aumentaron de uno a trece. La mediana del tiempo de notificación se elevó en Chiclayo (de cuatro a seis días) y Ferreñafe (de cuatro a 8,5 días), sin cambio significativo en Lambayeque (p=0,398). El tiempo de investigación también aumentó durante la pandemia, especialmente en Ferreñafe (de dos a 6,5 días), mientras que en Lambayeque se redujo levemente. Se encontró una correlación positiva y significativa entre el retraso en la notificación de dengue y los casos de COVID-19 (p=0,042), y ningún distrito alcanzó un tiempo óptimo de notificación, ni antes ni durante la pandemia Conclusión: La pandemia por COVID-19 afectó negativamente la vigilancia del dengue, con aumentos en los tiempos de notificación e investigación y cambios geográficos en la distribución de casos.
Palabras claves:
Salud bucal, caries dental, morbilidad, estudio observacional, Perú (Fuente. DeCS BIREME).
INTRODUCTION
Infectious diseases have the potential to spread rapidly, causing significant losses in health, the economy, and social well-being. Epidemiological surveillance is a fundamental tool for the timely detection of infectious diseases with epidemic potential, allowing for the early implementation of containment measures at the local level, with the aim of reducing their impact on public health
1
➤
1. Steele L, Orefuwa E, Dickmann P. Drivers of earlier infectious disease outbreak detection: a systematic literature review. Int J Infect Dis. 2016;53:15-20. doi:10.1016/j.ijid.2016.10.005.
,
2
➤
2.ifschitz V, Sanchez L. Epidemias: un recorrido por experiencias previas. 1ª ed. Argentina: Hospital José Ramón Vidal; 2021 [cited 2023 Oct 10]. Available from: https://www.researchgate.net/publication/354073154_EPIDEMIAS_UN_RECORRIDO_POR_EXPERIENCIAS_PREVIAS.
,
3
➤
3. Hidalgo García M. Las enfermedades infecciosas el gran desafío de seguridad en el siglo XXI. Cuad Estrateg. 2019;(203):37-80. Available from: https://dialnet.unirioja.es/servlet/articulo?codigo=7269522.
.
In recent decades, the emergence and re-emergence of arboviruses have posed a considerable threat to global health. Arboviruses, known as arthropod-borne viruses, are primarily transmitted by mosquitoes. Among the most common are dengue virus, yellow fever virus, West Nile virus, Chikungunya virus, and more recently, Zika virus
4
➤
4.Espinal M, Andrus J, Jauregui B, Hull S, Morens D, Santos J, et al. Arbovirosis emergentes y reemergentes transmitidas por Aedes en la Región de las Américas: implicaciones en materia de políticas de salud. Pan Am J Public Health [Internet]. 2019;43:1-8 [cited 2023 Aug 17]. Available from: https://iris.paho.org/handle/10665.2/50939
,
5
➤
5.Jones R, Kulkarni M, Davidson T, Talbot B, Sander B, González C, et al. Arbovirus vectors of epidemiological concern in the Americas: A scoping review of entomological studies on Zika, dengue and chikungunya virus vectors. PLoS One [Internet]. 2020 [cited 2023 Aug 17];15(2):1-17. Available from: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0220753.
,
6
➤
6. 6. Marquetti M, Bisset A, Martínez Y. Vigilancia de Aedes aegypti y el dengue en tiempo de COVID-19. Rev Cubana Hig Epidemiol [Internet]. 2023 [cited 2023 Dec 12];60:e1382. Available from: http://scielo.sld.cu/scielo.php?script=sci_abstract&pid=S1561-30032023000100017&lng=en&nrm=iso&tlng=es.
,
7
➤
7. 7. Organización Panamericana de la Salud [Internet]. Módulo de principios de epidemiología para el control de enfermedades (MOPECE). OPS; 2011 [cited 2023 Oct 10]. Available from: https://www3.paho.org/hq/index.php?option=com_content&view=article&id=9161:2013-mopece-training-modules-epidemiology&Itemid=0&lang=es#gsc.tab=0
.
Developing countries have faced recurrent arbovirus outbreaks, often worsened by delays in case detection and implementation of control measures. Factors such as unplanned urban growth, overcrowding, deficiencies in water and sanitation systems, climate change, and migration contribute to the complexity and increasing incidence of these diseases
7
➤
7. 7. Organización Panamericana de la Salud [Internet]. Módulo de principios de epidemiología para el control de enfermedades (MOPECE). OPS; 2011 [cited 2023 Oct 10]. Available from: https://www3.paho.org/hq/index.php?option=com_content&view=article&id=9161:2013-mopece-training-modules-epidemiology&Itemid=0&lang=es#gsc.tab=0
.
In Peru, approximately 20 million people live in areas at risk for arbovirus transmission
8
➤
8. 8. Centro Nacional de Epidemiología, Prevención y Control de Enfermedades. Sala situacional del dengue [Internet]. Perú: CDC MINSA; 2021 [cited 2023 Oct 10]. Available from: https://www.dge.gob.pe/portalnuevo/.
,
9
➤
9. 9. Cuba H. La pandemia en el Perú [Internet]. Lima: Fondo Editorial Comunicacional Colegio Médico del Perú; 2021 [cited 2023 Oct 10]. Available from: https://www.cmp.org.pe/wp-content/uploads/2021/05/La-Pandemia-CUBA-corregida-vale.pdf.
.
Over the past five years, there has been a sustained and alarming increase in dengue incidence, despite ongoing control efforts. This trend may be related to reduced effectiveness of surveillance and control measures, possibly due to the prioritization of resources toward managing the COVID-19 pandemic, which may have impacted the response to other communicable diseases, such as those caused by arboviruses
10
➤
10. Wu Q, Dong S, Li X, Yi B, Hu H, Guo Z, et al. Effects of COVID-19 non-pharmacological interventions on dengue infection: a systematic review and meta-analysis. Front Cell Infect Microbiol [Internet]. 2022 [cited 2023 Dec 10];12:892508. doi:10.3389/fcimb.2022.892508.
,
11
➤
11. Vasquez-Chavesta A, Morán-Mariños C, Rodrigo-Gallardo P, Toro-Huamanchumo CJ. COVID-19 and dengue: pushing the Peruvian health care system over the edge. Travel Med Infect Dis [Internet]. 2020 [cited 2020 Dec 10];36:101803. doi:10.1016/j.tmaid.2020.101808.
.
This study aims to analyze the notification and epidemiological investigation times of dengue cases in the Lambayeque region during 2019 and 2020, and to evaluate their correlation with the number of COVID-19 cases.
METHODS
Study design and area
A cross-sectional descriptive study was conducted using data from the epidemiological notification system of the Lambayeque Regional Health Office (noti.sp) and the COVID-19 Surveillance System (SISCOVID). The study area was the Lambayeque region, located on the northern coast of Peru, which presents climatic and demographic conditions conducive to arbovirus transmission.
Population and sample
All records of dengue cases reported in the noti.sp system and COVID-19 cases recorded in the SISCOVID system for the periods before and during the pandemic were considered. No sampling criteria were applied, as all available data provided by the epidemiology office of the Lambayeque Regional Health Office were included.
Variables and instruments
Variables included notification and investigation times for dengue cases, as well as the number of confirmed COVID-19 cases per epidemiological week. These variables were obtained from the mentioned institutional databases. Surveillance times were defined as the number of days between the onset of symptoms and case notification, and between notification and the epidemiological investigation.
Procedures
Database information was cleaned and structured before analysis to ensure the integrity and consistency of variables. Two analysis periods were identified: before and during the pandemic, defined based on the official declaration of the public health emergency. For each period, dengue surveillance times were estimated as the days between symptom onset and notification, and between notification and the epidemiological investigation. Additionally, weekly data on confirmed COVID-19 cases were integrated to explore their possible association with variations in dengue surveillance times.
Statistical analysis
Measures of central tendency and dispersion were calculated to describe notification and investigation times. Since the data did not follow a normal distribution, the non-parametric Mann-Whitney test was used to compare medians between the two periods. Spearman’s correlation coefficients were also estimated to assess the relationship between dengue surveillance times and the number of COVID-19 cases. Statistical analysis was performed using Stata version 16. For geospatial visualization of cases, Q-GIS software was used to map their distribution in the Lambayeque region.
Ethical considerations
The research protocol was reviewed and approved by the Research Ethics Committee of the Universidad Católica Santo Toribio de Mogrovejo and by the Ministry of Health (MINSA, by its Spanish acronym), ensuring compliance with ethical principles for research using secondary data.
RESULTS
Between 2019 and 2020, a total of 1,598 dengue cases were reported in the provinces of Chiclayo, Lambayeque, and Ferreñafe, with a higher prevalence in 2019, during which 957 cases were reported. The province of Ferreñafe accounted for the highest proportion of reported cases in 2019 (81.9%), whereas in 2020 only eight cases were reported in this province. Overall, 78.8% of cases were confirmed through clinical criteria and laboratory tests, with 695 confirmed cases in 2019 and 565 in 2020.
More than 4% of cases in both years presented warning signs. One severe case was identified in 2019 and thirteen in 2020. The highest proportion of cases occurred among adults and older adults. The average age was 36.3 years in 2019 and 36.4 years in 2020 (Table 1).
| Characteristics | 2019, n (%) | 2020, n (%) |
|---|---|---|
| Sex | Male: 436 (45,6%) Female: 521 (54,4%) |
Male: 322 (50,2%) Female: 319 (49,8%) |
| Age, mean ± SD | 36,3 ± 21,1 | 36,4 ± 20,6 |
| Province | Chiclayo: 135 (14,1%) Ferreñafe: 784 (81,9%) Lambayeque: 38 (4,0%) |
Chiclayo: 431 (67,2%) Ferreñafe: 8 (1,3%) Lambayeque: 202 (31,5%) |
| Case Type | Probable: 75 (7,8%) Confirmed: 695 (72,6%) Descarded: 187 (19,5%) |
Probable: 10 (1,6%) Confirmed: 565 (88,1%) Descarded: 66 (10,3%) |
| Type of dengue | Without warning signs: 912 (95,3%) With warning signs: 44 (4,6%) Severe: 1 (0,1%) |
Without warning signs: 613 (95,6%) With warning signs: 15 (2,3%) Severe: 13 (2,0%) |
| Age group | Children: 130 (13,8%) Adolescents: 81 (8,5%) Young adults: 192 (20,1%) Adults: 397 (41,5%) Older adults: 157 (16,4%) |
Children: 73 (11,4%) Adolescents: 62 (9,7%) Young adults: 141 (22%) Adults: 269 (42,0%) Older adults: 96 (15,0%) |
SD: Standard deviation
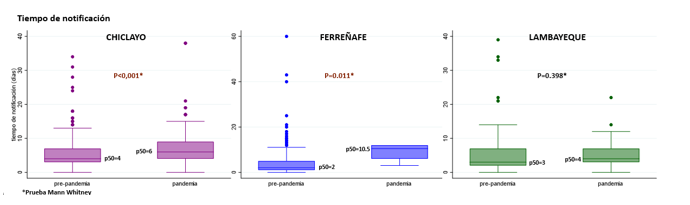
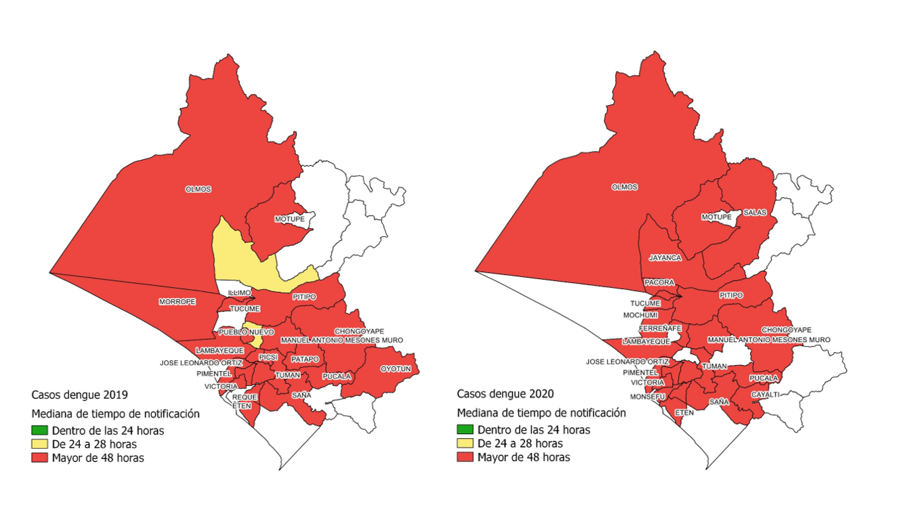
Regarding notification time, significant differences were observed between the periods before and during the coronavirus disease 2019 (COVID-19) pandemic. In the province of Chiclayo, the median notification time increased from four to six days during the pandemic. In Ferreñafe, despite the marked decrease in the number of cases, the median notification time rose to 8.5 days. In contrast, in Lambayeque, although an increase in the average notification time was recorded, it was not statistically significant (p-value = 0.398) (Figure 1).
Figure 1
Dengue notification time in the provinces of Chiclayo, Ferreñafe, and Lambayeque during 2019 and 2020.
With respect to investigation time, defined as the number of days between symptom onset and the date of epidemiological investigation, variations were also observed between both periods. In Chiclayo and Ferreñafe, the median investigation time increased during the pandemic, with Ferreñafe showing the largest increase—from two to 6.5 days. In contrast, a decrease was observed in Lambayeque (Figure 2).
Figure 2
Dengue investigation time in the provinces of Chiclayo, Ferreñafe, and Lambayeque during 2019 and 2020.
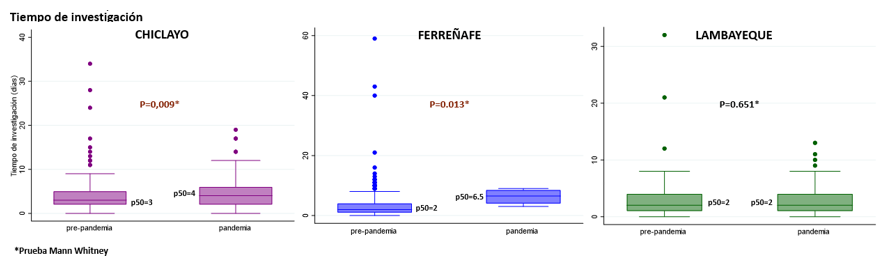
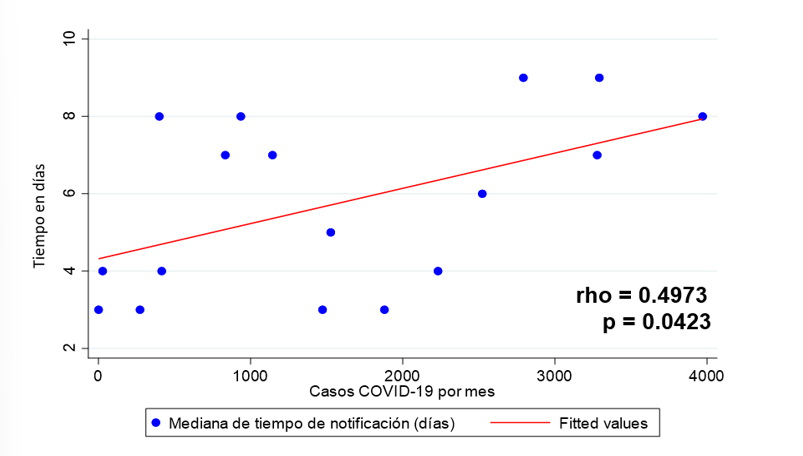
Figure 3 shows a scatter plot between dengue notification time and the number of COVID-19 cases. A statistically significant positive correlation was identified (p-value = 0.042), suggesting that as the number of COVID-19 cases increased, delays in dengue case notification also increased.
Figure 3
Scatter plot of dengue notification time and COVID-19 cases in the provinces of Chiclayo, Ferreñafe, and Lambayeque during 2019 and 2020.
During the pandemic period, there was an increase in the number of districts where the median investigation time exceeded 48 hours, as shown in Figure 4. Likewise, notification time was notably affected, with more districts experiencing delays in reaching an optimal time. Figure 5 shows that no district achieved an optimal notification time, either before or during the pandemic, highlighting the need to strengthen surveillance processes and health response to concurrent communicable diseases.
Figure 4
Geographic distribution of the median epidemiological investigation time for dengue cases in the districts of the Lambayeque region during 2019 and 2020.
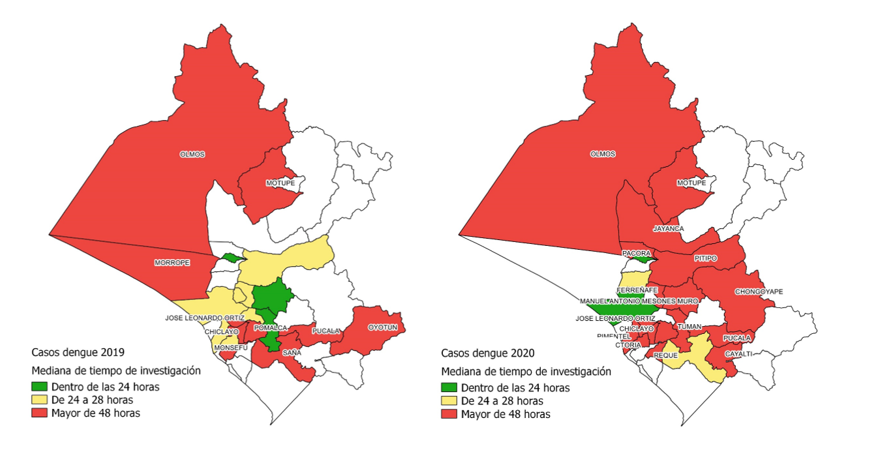
Figura 5
Geographic distribution of the median notification time for dengue cases in the districts of the Lambayeque region during 2019 and 2020.
DISCUSSION
In the Lambayeque region, a 19% decrease in reported dengue cases was observed between 2019 and 2020—a trend also reported in other endemic regions of Peru
12
➤
12. 12. Lorenz C, Días A, Correa C, Reis L, Chiaravalloti-Neto F, Alves A, et al. Have measures against COVID-19 helped to reduce dengue cases in Brazil? Travel Med Infect Dis [Internet]. 2020 [cited 2023 Oct 10];37:101734. doi:10.1016/j.tmaid.2020.101827.
. However, significant changes were identified in the geographical distribution of cases during 2020, highlighting an increase in the provinces of Chiclayo and Lambayeque, despite the overall decrease in the total number of diagnosed cases during the pandemic. This reduction was mainly due to an 80% decrease in reported cases in Ferreñafe. The literature suggests that these differences may have a multifactorial origin, including changes in the availability of health services, modifications in health-seeking behavior, and variations in epidemiological surveillance practices. Nevertheless, it is important to note that this study did not explore these factors in depth, which represents one of its limitations. Although an increase in the median notification time for dengue cases in 2020 was documented—reaching 10.5 days—more detailed analysis is needed to fully understand its impact on disease incidence and management.
At the regional level, in the Americas, a reduction in the incidence of arboviral diseases has been reported, with approximately 500,000 fewer cases between 2019 and 2021, attributed to social distancing and lockdown measures implemented in response to the COVID-19 pandemic
13
➤
13. 13. Organización Panamericana de la Salud [Internet]. Actualización epidemiológica semanal para dengue, chikunguña y zika en 2022. 2023 [cited 2023 Oct 10]. Available from: https://www.paho.org/es/documentos/actualizacion-epidemiologica-dengue-chikunguna-zika-10-junio-2023.
. Similarly, in Germany, a significant decline in cases of vector-borne diseases such as dengue and malaria was reported, with reductions of 75.1% and 73.0%, respectively, compared to expected cases. These decreases have been attributed to non-pharmaceutical interventions such as travel restrictions and border closures, which limited the importation of non-endemic infectious diseases into that country
14
➤
14. 14. Ullrich A, Schranz M, Rexroth U, Hamouda O, Schaade L, Diercke M, et al. Impact of the COVID-19 pandemic and associated non-pharmaceutical interventions on other notifiable infectious diseases in Germany: an analysis of national surveillance data during week 1-2016 - week 32-2020. Lancet Reg Health Eur [Internet]. 2021 [cited 2024 Apr 10];6:100103. doi:10.1016/j.lanepe.2021.100103.
.
In the present study, a significant disruption in the timeliness of dengue case notification was observed, particularly in the province of Ferreñafe. Differences in notification times were identified before and during the pandemic in the provinces of Chiclayo and Ferreñafe, along with a statistically significant correlation between increased dengue case notification time and the rising number of COVID-19 cases. This pattern could be related to an overload on the surveillance system and the prioritization of resources toward pandemic response. The association between delays in dengue case notification and the rise in COVID-19 incidence suggests additional pressure on health services during this period. These findings reinforce the need to strengthen surveillance and notification systems to effectively address concurrent epidemics.
Similar situations have been observed in Brazil and Mexico, where a decrease in dengue incidence coincided with a rise in COVID-19 cases
15
➤
15. 15. Mejía H, Apestegui B, Arteaga F. Incidencia del virus de dengue en Perú, a lo largo de la pandemia de COVID-19. Gac Médica Boliv [Internet]. 2023 [cited 2023 Oct 10];46(1):23-26. Available from: http://www.scielo.org.bo/scielo.php?script=sci_arttext&pid=S1012-29662023000100023.
,
16
➤
16. 16. Moctezuma-Paz A, Flores-Legorreta J, Benítez-Ganzález G, Solís-Chávez P. Dengue en tiempos de COVID-19. Rev Med Inst Mex Seguro Soc [Internet]. 2021 [cited 2023 Oct 10];59(6):463-464. Available from: https://pubmed.ncbi.nlm.nih.gov/34904817/.
, suggesting underreporting or delays in dengue case detection due to the redeployment of epidemiological surveillance teams during the pandemic
17
➤
17. 17. Godoy-Zendejas P, Villa-Manzano A, Robles-Cruz J, Yáñez-Ortega R, Saldate-Meza Y. Efecto de la pandemia SARS-CoV-2 (COVID-19) sobre las enfermedades por vectores en México. Sal Jal [Internet]. 2023 [cited 2023 Dec 10];10(3):134-7. Available from: https://www.medigraphic.com/cgi-bin/new/resumen.cgi?IDARTICULO=113302&idP=10493.
,
18
➤
18. 18. Nakandakari M, Marín-Macedo H, Seminario-Vilca X. Dengue con signos de alarma y leptospirosis en un paciente pediátrico con Covid-19. Rev Fac Med Hum [Internet]. 2021 [cited 2023 Oct 10];21(2):438-44. Available from: https://www.scielo.org.pe/scielo.php?pid=S2308-05312021000200438&script=sci_abstract.
. These results highlight the need to improve the efficiency of epidemiological surveillance and establish effective communication strategies to ensure early detection and better control of dengue outbreaks
19
➤
19. 19. Bergero P, Guisoni N. Modelo matemático de coinfección de dengue y COVID-19: una primera aproximación. Rev Argent Salud Publica [Internet]. 2021 [cited 2023 Oct 10];13:e000. Available from: https://www.scielo.org.pe/scielo.php?pid=S2308-05312021000200438&script=sci_abstract.
.
Additionally, the discussion can be enriched by comparing these findings to a global study
20
➤
20. 20. Liang Y, Dai X. The global incidence and trends of three common flavivirus infections (Dengue, yellow fever, and Zika) from 2011 to 2021. Front Microbiol. 2024;15:1458166. doi: 10.3389/fmicb.2024.1458166.
that analyzed trends in flavivirus infection incidence across 204 countries and reported an annual age-standardized incidence rate decrease of 8.4% between 2016 and 2019, followed by stabilization between 2019 and 2021—a period coinciding with the COVID-19 pandemic. These data support the hypothesis that non-pharmaceutical interventions implemented during the pandemic may have influenced the reduction in arbovirus transmission across various regions.
Among the limitations of this study is the use of secondary data from administrative records, which may be subject to underreporting, data entry errors, or incomplete variables. Moreover, contextual variables were not included, nor were individual factors related to access to healthcare, risk perception, or coverage of vector control activities evaluated, limiting the causal interpretation of the findings. On the other hand, a strength of this study lies in the inclusion of all reported cases in the Lambayeque region over a two-year period, providing a comprehensive perspective on dengue surveillance behavior before and during the COVID-19 pandemic. Furthermore, the temporal and geospatial analysis allowed for the identification of relevant patterns to guide targeted interventions and strengthen the health system’s capacity to respond to concurrent public health emergencies.
CONCLUSION
This study describes variations in the dynamics of dengue case notification and investigation in the Lambayeque region between 2019 and 2020, a period during which the COVID-19 pandemic also occurred. Changes were observed in the geographical distribution of cases, an overall reduction in the number of notifications, and an increase in surveillance times in certain provinces. Furthermore, a correlation was identified between the increase in COVID-19 cases and delays in dengue case notification.
This study provides a comprehensive overview of dengue dynamics in Lambayeque and highlights the coexistence of epidemic outbreaks, as well as the need to strengthen epidemiological surveillance systems in complex scenarios. Adapting public health strategies is crucial to respond to future threats posed by vector-borne diseases.
The reduction in reported cases should be interpreted with caution, as it does not always reflect lower transmission. Factors such as limited access to healthcare services, changes in health-seeking behavior, and deficiencies in reporting systems may contribute to underreporting. Therefore, it is essential to keep surveillance systems and preventive measures active, even in contexts of an apparent decline in cases.
Additional Information
Authorship contributions: KAZCH: conceptualization, investigation, and writing – original draft. JESF: conceptualization, investigation, and writing – original draft. ERPS: conceptualization, investigation, writing – original draft, formal analysis, and writing – review and editing. All authors approved the final version for publication. Conflict of interest statement: The authors declare no conflicts of interest. Funding: Self-funded. Received: August 5, 2024 Approved: March 28, 2025
Author Correspondence Data
Correspondence author: CJorge Enrique Silva Fiestas E-mail: jorgesilvafiestas@gmail.com
Article published by the Journal of the Faculty of Human Medicine of the Ricardo Palma University. This is an open-access article, distributed under the terms of the Creative Commons License: Creative Commons Attribution 4.0 International, CC BY 4.0 , which permits non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited. For commercial use, please contact revista.medicina@urp.edu.pe.
BIBLIOGRAPHIC REFERENCES
1
Steele L, Orefuwa E, Dickmann P.
Drivers of earlier infectious disease outbreak detection: a systematic literature review. Int J Infect Dis. 2016;53:15-20.
2
Ifschitz V, Sanchez L.
Epidemias: un recorrido por experiencias previas. 1ª ed. Argentina: Hospital José Ramón Vidal; 2021.
3
Hidalgo García M.
Las enfermedades infecciosas el gran desafío de seguridad en el siglo XXI. Cuad Estrateg. 2019;(203):37-80.
4
Espinal M, Andrus J, Jauregui B, Hull S, Morens D, Santos J, et al.
Arbovirosis emergentes y reemergentes transmitidas por Aedes en la Región de las Américas: implicaciones en materia de políticas de salud. Pan Am J Public Health. 2019;43:1-8.
5
Jones R, Kulkarni M, Davidson T, Talbot B, Sander B, González C, et al.
Arbovirus vectors of epidemiological concern in the Americas: A scoping review of entomological studies on Zika, dengue and chikungunya virus vectors. PLoS One. 2020;15(2):1-17.
6
Marquetti M, Bisset A, Martínez Y.
Vigilancia de Aedes aegypti y el dengue en tiempo de COVID-19. Rev Cubana Hig Epidemiol. 2023;60:e1382.
7
Organización Panamericana de la Salud.
Módulo de principios de epidemiología para el control de enfermedades (MOPECE). OPS; 2011.
8
Centro Nacional de Epidemiología, Prevención y Control de Enfermedades.
Sala situacional del dengue. Perú: CDC MINSA; 2021.
9
Cuba H.
La pandemia en el Perú. Lima: Fondo Editorial Comunicacional Colegio Médico del Perú; 2021.
10
Wu Q, Dong S, Li X, Yi B, Hu H, Guo Z, et al.
Effects of COVID-19 non-pharmacological interventions on dengue infection: a systematic review and meta-analysis. Front Cell Infect Microbiol. 2022;12:892508.
11
Vasquez-Chavesta A, Morán-Mariños C, Rodrigo-Gallardo P, Toro-Huamanchumo CJ.
COVID-19 and dengue: pushing the Peruvian health care system over the edge. Travel Med Infect Dis [Internet]. 2020 [citado el 10 de diciembre de 2020];36:101803. doi:10.1016/j.tmaid.2020.101808.
12
Lorenz C, Días A, Correa C, Reis L, Chiaravalloti-Neto F, Alves A, et al.
Have measures against COVID-19 helped to reduce dengue cases in Brazil? Travel Med Infect Dis [Internet]. 2020 [citado el 10 octubre de 2023];37:101734. doi:10.1016/j.tmaid.2020.101827.
13
Organización Panamericana de la Salud [Internet].
Actualización epidemiológica semanal para dengue, chikunguña y zika en 2022. 2023 [citado el 10 octubre de 2023].
14
Ullrich A, Schranz M, Rexroth U, Hamouda O, Schaade L, Diercke M, et al.
Impact of the COVID-19 pandemic and associated non-pharmaceutical interventions on other notifiable infectious diseases in Germany: an analysis of national surveillance data during week 1-2016 - week 32-2020. Lancet Reg Health Eur [Internet]. 2021 [citado el 10 de abril de 2024];6:100103. doi:10.1016/j.lanepe.2021.100103.
15
Mejía H, Apestegui B, Arteaga F.
Incidencia del virus de dengue en Perú, a lo largo de la pandemia de COVID-19. Gac Médica Boliv [Internet]. 2023 [citado el 10 de octubre de 2023];46(1):23-26.
16
Moctezuma-Paz A, Flores-Legorreta J, Benítez-Ganzález G, Solís-Chávez P.
Dengue en tiempos de COVID-19. Rev Med Inst Mex Seguro Soc [Internet]. 2021 [citado el 10 de octubre de 2023];59(6):463-464.
17
Godoy-Zendejas P, Villa-Manzano A, Robles-Cruz J, Yáñez-Ortega R, Saldate-Meza Y.
Efecto de la pandemia SARS-CoV-2 (COVID-19) sobre las enfermedades por vectores en México. Sal Jal [Internet]. 2023 [citado el 10 de diciembre de 2023];10(3):134-7.
18
Nakandakari M, Marín-Macedo H, Seminario-Vilca X.
Dengue con signos de alarma y leptospirosis en un paciente pediátrico con Covid-19. Rev Fac Med Hum [Internet]. 2021 [citado el 10 de octubre de 2023];21(2):438-44.
19
Bergero P, Guisoni N.
Modelo matemático de coinfección de dengue y COVID-19: una primera aproximación. Rev Argent Salud Publica [Internet]. 2021 [citado el 10 de octubre de 2023];13:e000.
20
Liang Y, Dai X.
The global incidence and trends of three common flavivirus infections (Dengue, yellow fever, and Zika) from 2011 to 2021. Front Microbiol. 2024;15:1458166. doi: 10.3389/fmicb.2024.1458166.