Introduction
Actinic keratosis is a premalignant dermatological condition characterized by its potential to progress to squamous cell carcinoma
1
. These lesions appear in areas with a significant history of sun exposure and can be mistaken for other commonly observed lesions caused by the same trigger factor
2, 3
. To date, there is a significant and precise lack of data to describe its epidemiological behavior
4
. However, it is presumed to be more common than previously thought in coastal areas where operational and labor environments are linked to chronic sun exposure
5
.
Although its pathogenesis and physiopathology are not precisely known, ultraviolet exposure has been reported to induce changes in regulatory signaling pathways at the keratinocyte level in the epidermal layer, creating an oncogenic environment that stimulates replication, differentiation, and tumor migration
1, 5
. Therefore, early detection and timely management are essential to prevent progression to carcinoma. To date, there is no treatment with an adequate benefit-risk balance, as therapies focused on the lesion or the lesion territory frequently cause discomfort and side effects that affect the quality of life or result in morbidity
1, 3
.
Photodynamic therapy is considered one of the most effective therapeutic tools, as it can act on lesions that are not visible during physical examination, generating reactive oxygen species that eliminate abnormal cells
6, 7, 8
. However, there is still divergence regarding the quality of the available evidence
9, 10
,especially since very few studies have specifically attempted to answer the therapeutic efficacy of photodynamic therapy in actinic keratosis, despite advancements in certain technical aspects
4
. Given the relevance of this topic, particularly the lack of Spanish-language evidence that synthesizes literature for the understanding and potential management of this disease, the objective of this review is to analyze the most recent evidence on the therapeutic efficacy of photodynamic therapy in the management of actinic keratosis.
.
Methodology
A bibliographic search was designed and reproduced using the search terms photodynamic therapy and actinic keratosis, along with synonyms, which were combined with the operators AND and OR in the PubMed, Scopus, and MEDLINE databases. Any full-text article evaluating the efficacy and safety of photodynamic therapy in the management of actinic keratosis was included, prioritizing original studies, systematic reviews, and meta-analyses. Articles published up to 2023 were included. A total of five articles with potentially relevant clinical evidence were identified. Additionally, references were included for the discussion of basic theoretical aspects of the disease and future perspectives. The estimates and findings were expressed in their original measures, whether frequencies, percentages, confidence intervals (CI), mean differences (MD), relative risk (RR), odds ratios (OR), or hazard ratios (HR).
Physiopathological and therapeutic aspects of actinic keratosis
As mentioned earlier, actinic keratosis is a neoplasm resulting from the abnormal proliferation of epidermal keratinocytes
11
. Actinic keratosis lesions can present progressively but slowly and are characterized by small erythematous papules, sometimes pigmented, in areas with greater sun exposure
1, 12
.The surrounding skin often presents telangiectasias, skin discoloration, solar elastosis, and dermal atrophy. However, according to the natural history phases of the disease, these lesions can resolve spontaneously, persist benignly, or, in the worst-case scenario, progress to malignancy
13
. Nevertheless, it has been described that in cases where spontaneous regression occurs, there may be reappearance later
14
.
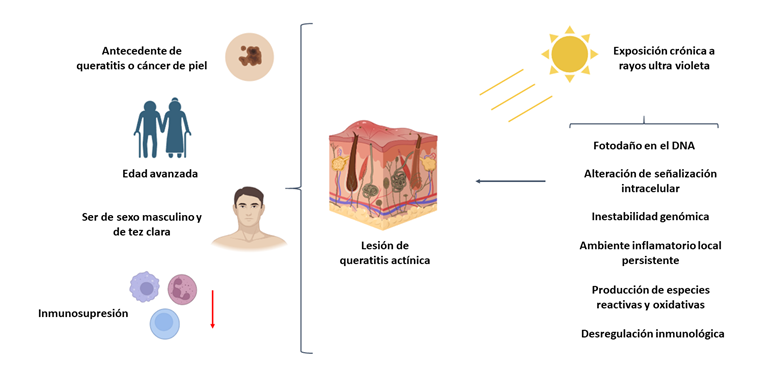
This behavior can be greatly influenced by some reported potential risk factors that may contribute to the persistence or progression of the lesions, such as advanced age (over 60-65 years), male sex, fair skin, immunosuppression, a history of actinic keratosis or skin cancer, and the main associated factor: chronic sun exposure, which is related to residing in a tropical region where higher temperatures are recorded compared to other areas with varied climates
14,15
. At the cellular and molecular levels, it has been proposed that, secondary to ultraviolet exposure, three mechanisms are triggered that can lead to genomic and cellular instability, resulting in the appearance of lesions and/or malignancy
16,17
.
Initially, ultraviolet rays cause photodamage to deoxyribonucleic acid (DNA), which, after significant exposure and alteration of cellular dynamics, leads to mutations in the p53 tumor suppressor gene and associated proteins, resulting in failure of the regulatory mechanisms of cell death, with consequent genomic instability and abnormal replication and/or differentiation
3
. Additionally, ultraviolet rays, acting on the cellular phospholipid membrane, interact with arachidonic acid, leading to the release of prostaglandins through lytic processes, creating a chronic inflammatory environment
1
. Moreover, alterations in intracellular signaling have been described, due to the deregulation of reactive oxygen species metabolism, platelet-activating factor, and trans-urocanic acid, leading to cellular damage
3
. All of this produces a local immunological disorder that causes immunosuppression, which, combined with other physiopathological mechanisms, stimulates a pro-tumoral environment (figure 1).
Figure 1
Cellular and molecular mechanisms and risk factors associated with the pathogenesis and pathophysiology of actinic keratosis. Source: Own elaboration.
Based on the information above, certain therapies have been proposed
Such as cryotherapy, resection or excision, for the removal of lesions directly in the affected area
18, 19, 20
. Among the treatments applied directly to the site of the lesions, dermabrasion, laser, chemical peeling, photodynamic therapy, and topical medication (using 5-Fluorouracil, sodium diclofenac, or imiquimod) can be used. Of these, dynamic phototherapy aims to apply a photosensitizer to a specific area, which, after controlled light exposure, generates reactive oxygen species that selectively destroy abnormal cells
1, 19, 20
. However, among the disadvantages described is pain production, which requires a prolonged waiting time in specialized centers. This is where the variation of daylight dynamic phototherapy comes into play. This therapy has evolved in recent years for this condition
16, 18, 19
. However, how much evidence is there, and what is its quality?
Evolution of photodynamic therapy in the management of actinic keratosis: How effective and safe is it?
Considering that the number of non-melanoma skin cancer cases has increased globally in recent years
21
, it is necessary to have high-quality clinical evidence applicable to real-world practice.
In 2012, in a Cochrane review conducted by Gupta et al.
22
, evidence was systematized on interventions for actinic keratosis, including 83 randomized controlled trials with a sample of 10,036 subjects. Firstly, the authors highlighted a methodological deficit among the studies, with a high risk of reporting bias. Secondly, regarding outcomes, in the case of lesion clearance, site-directed treatments: 3% diclofenac plus 2.5% hyaluronic acid (RR 2.46; 95% CI: 1.66 - 3.66), 0.5% 5-fluorouracil (RR 8.86; 95% CI: 3.67 – 21.44), 5% imiquimod (RR 7.70; 95% CI: 4.63 – 12.79), and 0.025%-0.05% ingenol mebutate (RR 4.50; 95% CI: 2.61 – 7.74) showed superiority compared to placebo. Regarding photodynamic therapy, it was evidenced that, in the case of individual lesion resolution, the combined use of aminolevulinic acid and methyl aminolevulinate as photosensitizers with phototherapy increased the likelihood of lesion resolution by 5.22 (95% CI: 2.88 – 13.43) and 3.56 (95% CI: 3.17 – 6.28) times. However, a significant number of patients (n=261/4000) experienced adverse effects, leading to withdrawal. Still, up to that point, phototherapy was concluded to be the most effective therapy in terms of resolution and cosmetic outcomes compared to other therapies
22
.
In 2021, Galitzer et al.
23
published the results of the first randomized study, which included 15 patients with actinic keratosis, aiming to determine the efficacy and safety of dynamic phototherapy. They used 10% levulinic acid gel, red light, and adapalene prior to treatment. The therapy was implemented as follows: the use of 0.1% adapalene gel twice daily for one week before dynamic phototherapy application. The control group was exposed to dynamic phototherapy only. After eight weeks, it was found that 12 subjects in the intervention group achieved 50% to 100% lesion resolution, compared to 10 subjects in the control group. Additionally, the median lesion reduction time was 72% shorter compared to the control group (p=0.01); both groups had good tolerability, and patients reported high satisfaction. It was concluded that the proposed scheme was effective and safe for the management of actinic keratosis
23
.
A year later, Kiss et al.
24
shared the results
of a case series composed of 10 patients who underwent a single session of photodynamic therapy combined with aminolevulinic acid. The researchers observed a complete response in three individuals and partial response in the rest. Overall, tolerability was good, with local adverse events reported in only four patients.
Recently, in 2023, Salman et al. (25) conducted the most up-to-date meta-analysis evaluating the safety and efficacy of the combination of cryotherapy and dynamic phototherapy with imiquimod for actinic keratosis, including five studies. The global analysis showed that the combination of cryotherapy and imiquimod increased the probability of lesion resolution by up to 5.2 times (95% CI: 1.56 – 24.1; p=0.01), compared to other regimens. Additionally, combining imiquimod with photodynamic therapy increased lesion resolution by 5% compared to using either therapy alone
25
. Up to this point, these regimens were considered the most effective therapies for managing actinic keratosis.
Until Anvery et al.
10
published the results of a randomized controlled trial comparing the use of photodynamic therapy combined with aminolevulinic acid without incubation versus with one-hour incubation for actinic keratosis. The authors included 27 subjects (n=13 in the intervention group versus n=14 in the control group) and evaluated outcomes at one week and eight weeks. After follow-up, it was shown that the intervention group had a higher percentage of lesion resolution compared to the control group (49.5% versus 34.9%, p=0.002). Additionally, less pain was reported in the intervention group (p=0.03). However, there was no statistically significant difference in the average dermal irritation score, days to return to work, or patient satisfaction. Interestingly, 19 adverse events were reported in the intervention group, compared to 14 in the control group. Still, the authors concluded that the use of phototherapy with aminolevulinic acid without incubation could be more effective than therapy with incubation
10
.
This analysis shows an evolution from isolated photodynamic therapy to certain combinations, which demonstrate heterogeneous results. However, in addition to methodological limitations, the evidence is limited. Therefore, the synthesis of evidence should be analyzed and interpreted with caution, as the measurement and combination of therapies are highly divergent, and the results can be magnified.
Future perspectives
According to Cramer & Stockfleth
26
, actinic keratosis will become a more important pathological entity than currently thought, as climate and demographic transitions will increase sun exposure and the populations exposed, which could become the most frequent in situ skin carcinoma worldwide
26
. This should spark interest among researchers in skin cancer, not just dermatologists, but other health professionals and related individuals, to consider the clinical and translational evaluation of actinic keratosis
27
28
, where there is a significant lack of primary data, especially in Latin America and the Caribbean. Considering genomic and genetic population variability, it is imperative to conduct studies taking into account variables specific to each sociodemographic and health context to contribute to the search for answers that allow the implementation of strategies based on precision medicine
29
.
Current therapies are very diverse it is worth noting that the study population has been very similar, which prevents attempts to extrapolate results to communities with different anthropological, social, and clinical characteristics, as the natural history of the disease is unknown in certain populations. Based on these results, it is even possible to design and implement health policies and plans to create or modify roadmaps for screening, diagnosis, and timely treatment. In low- and middle-income countries, such as those in Latin America and the Caribbean
30
, it is necessary to promote this type of research to contribute to achieving global health goals and the global cancer agenda, in addition to promoting the development of science and technology in skin cancer and topics of interest in technology.
Conclusions
Although the evidence on the use of dynamic phototherapy and its various combined regimens for the management of actinic keratosis is limited and heterogeneous, there is a trend toward a potential benefit compared to other therapies, mainly due to lesion resolution, favorable patient satisfaction, and low or no pain perception, with a good benefit-risk balance, given by few adverse events.