Introducción
Non-compaction cardiomyopathy (NCC) is considered a separate entity from other cardiomyopathies
1
. The prevalence of non-compaction cardiomyopathy in children is 0.14%, with an unknown incidence
2
due to diagnostic difficulties, as many cases are initially identified as dilated cardiomyopathy.
Currently, it is believed that NCC results from a halt in normal heart embryogenesis, specifically in the compaction process. The etiology of the disease remains limited by genetic heterogeneity, with an incomplete understanding of myocardial trabeculation and compaction regulation
3
. NCC can affect the left ventricle, though more rarely, it may impact the right ventricle or both
4
.
The first case was described in 1932 from autopsy findings of a newborn with other cardiac abnormalities, but it wasn’t until 1984 that NCC was formally identified
4
. NCC in neonates and infants occurs in 2-7% of cases, with fetal prevalence likely higher, at 6%-11%, as many do not survive to birth
5
. Fetal echocardiography, using two-dimensional and M-mode imaging, is the recommended diagnostic approach, providing treatment guidance and determining myocardial maturity at birth
5
. Color Doppler allows detection of intertrabecular perfusion in the ventricular cavities, and currently, fetal NCC can be detected in both ventricles
6
. Diagnostic criteria have been established for echocardiographic image scoring, including those by Jenni et al.
7
, which consider the appearance of compacted and non-compacted layers, increased trabeculations in the lateral wall and apex of the left ventricle, synchronous movement of trabeculations with the myocardium, perfusion of intertrabecular recesses, and abnormal ventricular function. Diagnosing NCC in pediatric patients can be challenging and is sometimes confused with other cardiac pathologies, often creating false expectations for parents, as the medical recommendation for progressive NCC is heart transplantation.
This study aimed to assess the anatomical development of NCC in patients under one year old, evaluated through echocardiography. The findings from this study could help evaluate prognosis and guide future management decisions for these patients.
4
5
8
.
This study aimed to assess the anatomical development of NCC in patients under one year old, evaluated through echocardiography. The findings from this study could help evaluate prognosis and guide future management decisions for these patients.
METHODS
Study Design and Area
This retrospective cohort study included all patients hospitalized in the Pediatric Special Care Unit at Hospital Nacional Edgardo Rebagliati Martins (HNERM) - EsSalud, from 2017 to 2021 with an echocardiographic diagnosis of NCC confirmed based on Jenni’s criteria
7
.
Medical records were reviewed using Jenni’s diagnostic criteria
7
, recording data in centimeters for measurements of non-compacted (NC) myocardium represented by trabeculae, and compacted (C) myocardium. The NC/C ratio was calculated, with a diagnostic threshold of >2 as per Jenni. Ejection fraction (EF) and presence of recesses were evaluated, and the number of trabeculae was recorded, with modifications to values considered for interpretation.
The study applied the Jenni diagnostic method, referencing Passerini's article
9
which reports a sensitivity and specificity of 86% and 99% respectively for the NC/C myocardium ratio.
Statistical Analysis: Data were entered into SPSS software version 26. For each of Jenni's criteria, maximum, minimum, and average values with standard deviation were calculated. Echocardiographic follow-up values were subsequently calculated at 6, 12, 18, 24, 30, and 36 months (NC/C ratio, ejection fraction, and number of trabeculae). Finally, the mean and standard deviation were calculated for the non-compacted/compacted myocardium ratio, ejection fraction, and the number of trabeculae at diagnosis and at 6, 12, 18, 24, 30, and 36 months.
Aspectos éticos: En los aspectos éticos de la investigación, se solicitó autorización del comité de ética de la institución Carta N° 354-GRPR-ESSALUD-2024, se respetaron los principios éticos de Helsinki..
Ethical Considerations
Authorization was obtained from the institution’s ethics committee (Letter No. 354-GRPR-ESSALUD-2024), adhering to the ethical principles of the Declaration of Helsinki.
RESULTS
Frequency and percentages were calculated for descriptive data and patient evolution, while means and standard deviations were calculated for echocardiographic measurements, based on the 7 patients diagnosed with NCC.
Table 1. Descriptive data of studied patients
|
Frecuency |
Percentage |
|
Age at Diagnosis |
| Neonatal |
4 |
57.14 |
| Infant |
3 |
42.85 |
| Characteristics |
| Heart Failure |
6 |
85.70% |
| Arrhythmias |
3 |
42.80% |
|
Associated Heart Disease
|
3 |
42.80% |
| Biventricular Involvement |
2 |
28.57% |
| Reduced Ejection Fraction |
2 |
28.57% |
| Withdrawal |
1 |
14.30% |
| Remained in the Study |
3 |
42.80% |
| Mortality Rate |
3 |
42.80% |
A total of 7 patients with an echocardiographic diagnosis of non-compacted myocardium (NCM) confirmed by Jenni's criteria were analyzed. The patients were diagnosed within the first year of life: 4 patients (57.14%) in the neonatal stage and 3 patients (42.85%) during early infancy. Six patients (85.70%) experienced heart failure, 3 (42.80%) had arrhythmias, and 3 (42.80%) had associated heart diseases. Two patients (28.57%) presented with biventricular involvement, and ejection fraction was reduced in 2 patients (28.57%). One patient (14.3%) with a diagnosis of dysmorphic syndrome and neurological complications discontinued follow-up at two months of age. Three patients (42.8%) passed away: the first at 3 days, the second at 5 months, and the last at 1 year and 11 months.
Table 2. Jenni's Criteria - Admission Diagnosis of Non-Compacted Cardiomyopathy. 2017-2021
| Jenni Criteria and EF |
Minimum value |
Maximum value |
Mean X |
standard deviation |
| Number of trabeculae |
3 |
4 |
3.5 |
0.9 |
| Trabeculae size (cm) |
0.468 |
1.090 |
0.760 |
0.208 |
| Compact myocardium size (cm) |
0.190 |
0.350 |
0.260 |
0.055 |
| NC/C myocardium ratio |
2.460 |
4.500 |
3.480 |
0.980 |
| Ejection fraction (%) |
20.00 |
80.00 |
59.00 |
23.50 |
NC: Non-compacted myocardium, C: Compact myocardium
Table 2 describes the myocardial characteristics of the initial echocardiogram for the study patients, initially including 7 individuals. It shows a mean trabeculae count of 3.5, an average trabeculae size of 0.76 cm, and compact myocardium size of 0.26 cm, with a mean NC/C ratio of 3.48 and an average ejection fraction (EF) of 59%, calculated for 6 patients.
Table 3. Echocardiographic follow-up of patients diagnosed with non-compacted cardiomyopathy, 2017-2021
|
NC/C Ratio* |
Ejection fraction (EF) |
Number of Trabeculae |
| Patient |
Dx | 6 m | 12 m | 18 m | 24 m | 30 m | 36 m |
Dx | 6 m | 12 m | 18 m | 24 m | 30 m | 36 m |
Dx | 6 m | 12 m | 18 m | 24 m | 30 m | 36 m |
| 1 |
3.8 | 1.2 | 1.2 | 1.2 | 1.2 | 1.2 | 1.2 |
80 | 67 | 53 | 51 | 53 | 51 | 51 |
4 | 2 | 2 | 2 | 2 | 2 | 2 |
| 2 |
3.8 | 3.1 | 2.6 | 2.8 | 2.3 | 2.6 | 2.6 |
20 | 47 | 54 | 42 | 37 | 64 | 58 |
8 | 8 | 8 | 8 | 8 | 8 | 8 |
| 3 |
2.1 | 2.0 | 2.8 | 1.2 | 1.4 | 1.4 | 1.4 |
64 | 53 | 48 | 48 | 68 | 68 | 68 |
4 | 4 | 4 | 4 | 4 | 4 | 4 |
*NC Non-compacted myocardium,
C: Compact myocardium
In Table 3, the anatomical changes observed during the follow-up of the 3 patients who remained in the study show that the NC/C ratio remained high in only one patient, while ejection fraction (EF) improved in all patients. The number of trabeculae decreased in only one patient.
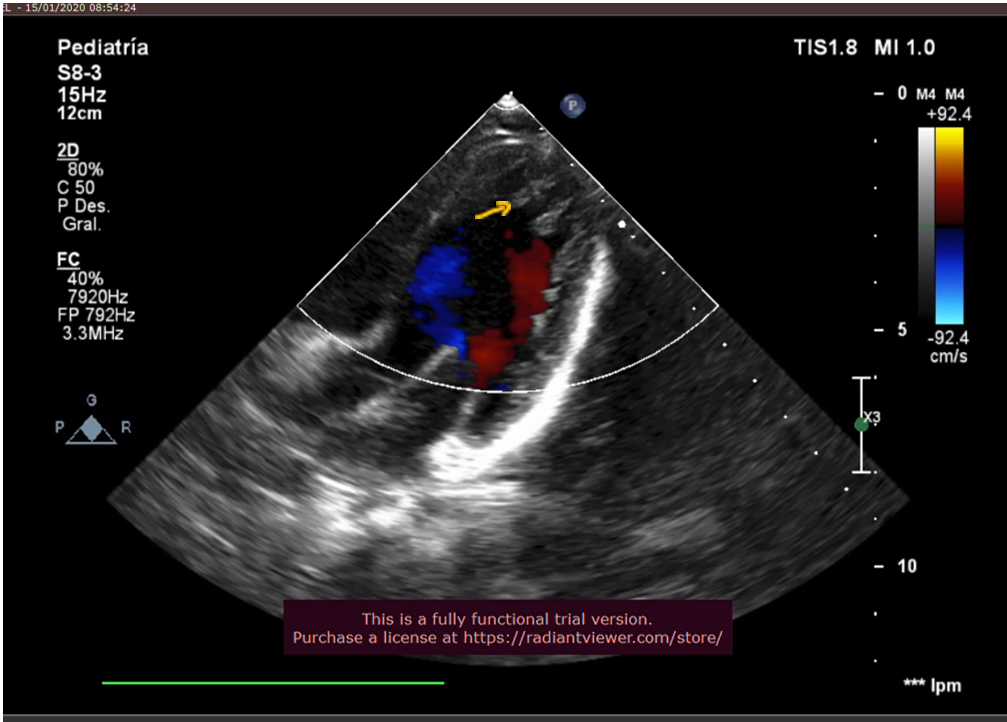
Figure 1
The yellow arrow indicates the trabeculae of the non-compacted myocardium.
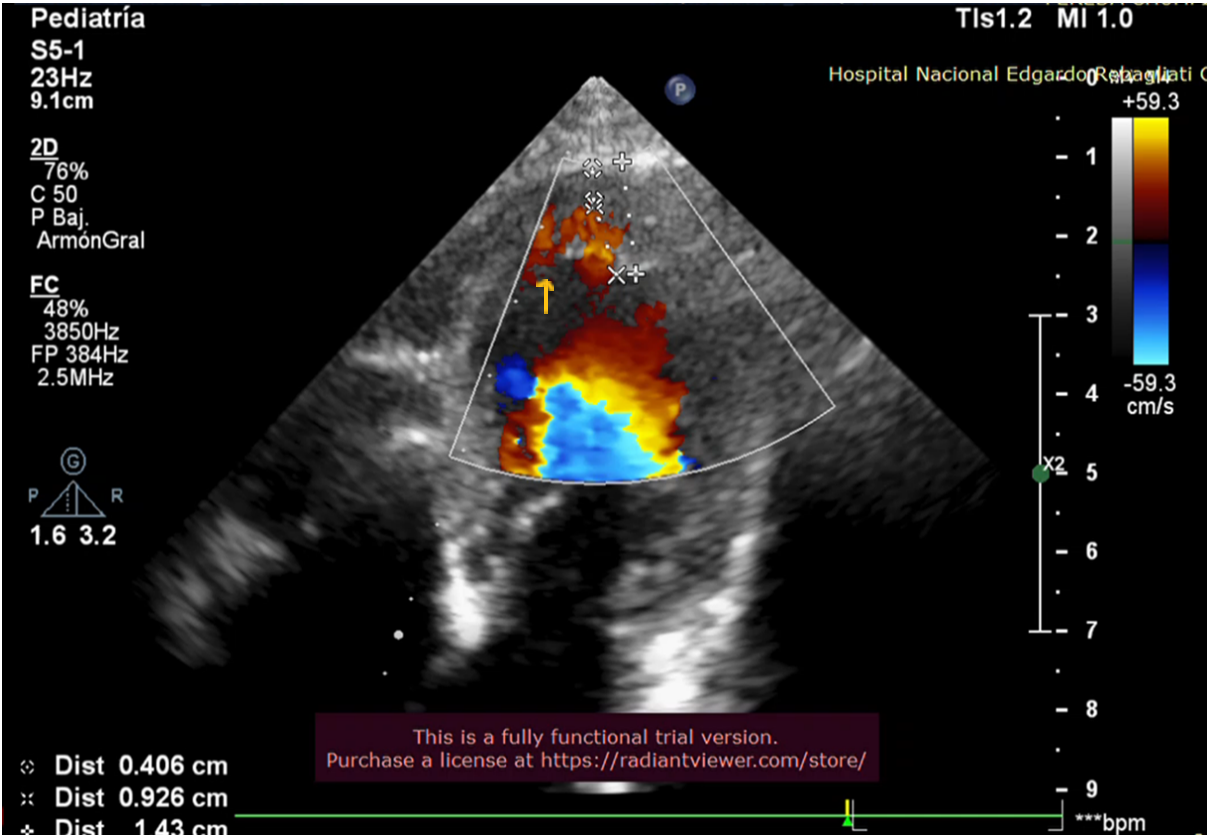
Figure 2
The yellow arrow indicates the presence of blood in the recesses.
Discussion
Non-compaction cardiomyopathy is a rare disease in pediatric patients, with limited understanding of its etiopathogenesis. It is suggested to have a genetic-familial origin, affecting myocardial maturation during fetal development
8
. Little is known about this condition in the neonatal stage or its progression in these patients
10
.
This study, conducted on 7 patients diagnosed with NCC, showed that myocardial maturation was completed after birth, with only one of the studied patients maintaining the diagnostic criteria for NCC.
In our study, 2 patients (28.57%) had involvement of both ventricles and eventually died. One case was associated with isolated supraventricular extrasystoles and congenital heart disease, and the other with genetic alteration (Down syndrome) and congenital heart disease. According to the literature reviewed by Dhar et al.
11
, biventricular involvement in NCC is rare, with only isolated cases reported.
In our study, EF was compromised in 2 patients (20% and 43%, respectively), who presented signs of heart failure associated with Wolff-Parkinson-White (WPW) syndrome. One of these patients also had neurodevelopmental delays and discontinued follow-up at 2 months of age.
Initially, the mean EF was 55%, decreasing to 47% at 18 months and subsequently rising to 59% by 36 months. The evolution of EF in the affected patients improved, normalizing between 18 and 30 months of age. These results align with findings reported by Menon
12
.
Regarding the follow-up of trabeculae, their number remained stable, though they decreased in size. The NC/C myocardium ratio normalized in two patients, one by 6 months of age, who did not have EF impairment, and another by 18 months, who also showed normalized EF. Only one patient retained the NCC diagnostic criteria at 36 months of follow-up but exhibited improved EF. Maurizio Mongiovi
5
notes that there is a possibility of improvement and sometimes normalization of left ventricular function in all forms of dilated cardiomyopathies, including NCC.
In this study, 3 patients (42.80%) passed away. One died early in the neonatal stage at 3 days old due to cardiogenic shock. There were two late deaths: one at 5 months associated with acyanotic heart disease and isolated supraventricular extrasystoles, and the second at 1 year and 11 months in a patient with Down syndrome and acyanotic heart disease. The literature indicates that the combination of heart disease and arrhythmias with NCC carries a high risk and poor prognosis
13
.
All study patients received a standardized medication regimen, consisting of pediatric doses of Carvedilol and antiplatelet doses of Acetylsalicylic Acid from diagnosis.
Limitations and Strengths
The limitations of this study include the high mortality rate within the patient group, reaching 42.80%, which reduced the number of patients available for follow-up.
Conclusion
Anatomical changes in patients diagnosed with non-compaction cardiomyopathy may progress to myocardial maturation and improvement in ventricular function.