Association between hematological parameters and metabolically unhealthy phenotypes in children and adolescents.
Asociación entre parámetros hematológicos y fenotipos metabólicamente poco saludables en niños y adolescentes
DOI:
https://doi.org/10.25176/RFMH.v23i3.5603Keywords:
adolescents, children, hematological indices, neutrophils, metabolically unhealthy phenotypesAbstract
Objective. Metabolic syndrome has been associated with changes in the composition of circulating blood cells. Hematologic indices can be used to identify the subjects at risk of metabolically unhealthy phenotype (MUP). This study investigated whether hematological indices can serve as biomarkers to distinguish metabolically healthy phenotype (MHP) from MUP in children and adolescents.
Methods. Two hundred ninety-two children and adolescents were enrolled in a cross-sectional study. The MUP was diagnosed using consensus-based criteria proposed by Damanhoury et al. Group comparisons were performed using one-way ANOVA. To examine if sex, age group, nutritional status, puberty, hematological parameters, and insulin resistance were associated with MUP, we used multiadjusted logistic regression analysis with metabolic status as the dependent variable.
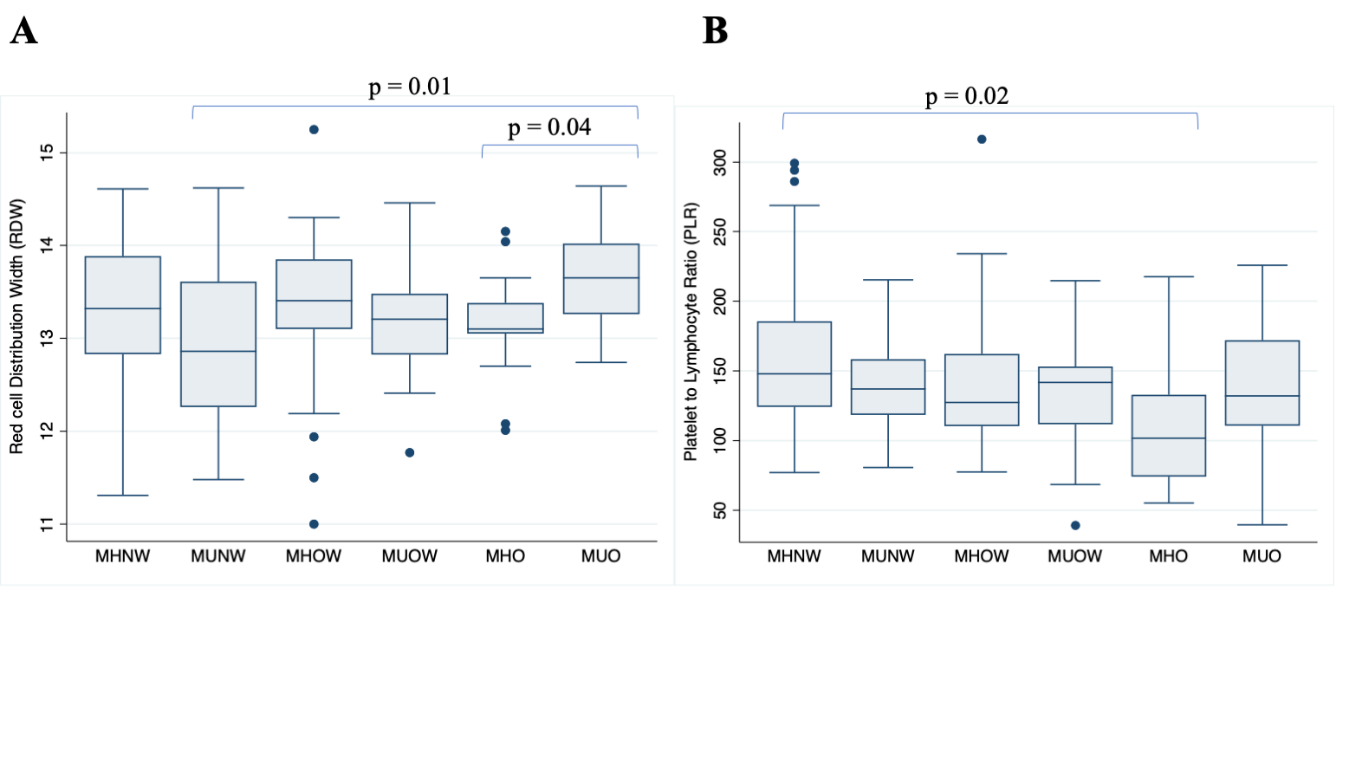
Results. The subject's age mean was 11 years (SD: 2.61). RDW values were significantly lower in children with metabolically unhealthy normal weight (MUNW) compared to children with metabolically unhealthy obesity (MUO) (12.33 ± 0.90 vs. 13.67 ± 0.52; p = 0.01), and in metabolically healthy obesity (MHO) compared to MUO (13.15 ± 0.53 vs. 13.67 ± 0.52; p = 0.04). In adolescents, the PLR was higher for the MHNW group, with a mean value of 152.60 (SD 62.97) compared to 111.16 (SD 44.12) for the MHO group. After adjusting for age, nutritional status, and puberty, hematological indices were not associated with MUP.
Conclusions. The study demonstrates that hematological indices are not independently associated with the metabolically unhealthy phenotype. Hematologic indices are unlikely to represent reliable biomarkers of MU phenotype in the pediatric population.
Downloads
References
Genovesi S, Antolini L, Orlando A, et al. Cardiovascular Risk Factors Associated With the Metabolically Healthy Obese (MHO) Phenotype Compared to the Metabolically Unhealthy Obese (MUO) Phenotype in Children. Front Endocrinol (Lausana). 2020;11:27. Doi: 10.3389/fendo.2020.00027.
Chiesa C, Pacifico L, Xi B, et al. Editorial: Metabolically Healthy and Unhealthy Obese Children and Adolescents. Front Endocrinol (Lausana). 2020;11:613703. Doi: 10.3389/fendo.2020.613703.
Makki K, Froguel P, Wolowczuk I. Adipose tissue in obesity-related inflammation and insulin resistance: cells, cytokines, and chemokines. ISRN Inflamm. 2013;2013:139239. Doi: 10.1155/2013/139239.
Aleksandrova K, Mozaffarian D, Pischon T. Addressing the Perfect Storm: Biomarcadores en Obesidad y Fisiopatología del Riesgo Cardiometabólico. Clin Chem. 2018;64(1):142-53. Doi: 10.1373/clinchem.2017.275172.
Aydin M, Yilmaz A, Donma MM, et al. Neutrophil/lymphocyte ratio in obese adolescents. North Clin Istanb. 2015;2(2):87-91. Doi: 10.14744/nci.2015.25238.
Aygun AD, Gungor S, Ustundag B, et al. Proinflammatory cytokines and leptin are increased in serum of prepubertal obese children. Mediators Inflamm. 2005;2005(3):180-3. Doi: 10.1155/MI.2005.180.
Zaldivar F, McMurray RG, Nemet D, et al. Body fat and circulating leukocytes in children. Int J Obes (Lond). 2006;30(6):906-11. Doi: 10.1038/sj.ijo.0803227.
Phillips CM, Perry IJ. ¿Determina la inflamación el estado de salud metabólica en adultos obesos y no obesos? J Clin Endocrinol Metab. 2013;98(10):E1610-9. Doi: 10.1210/jc.2013-2038.
Zhang SS, Yang XJ, Ma QH, et al. Leukocyte related parameters in older adults with metabolically healthy and unhealthy overweight or obesity. Sci Rep. 2021;11(1):4652. Doi: 10.1038/s41598-021-84367-7.
Marra A, Bondesan A, Caroli D, et al. The neutrophil to lymphocyte ratio (NLR) positively correlates with the presence and severity of metabolic syndrome in obese adults, but not in obese children/adolescents. BMC Endocr Disord. 2023;23(1):121. Doi: 10.1186/s12902-023-01369-4.
Fujita B, Strodthoff D, Fritzenwanger M, et al. Altered red blood cell distribution width in overweight adolescents and its association with markers of inflammation. Obesidad pediátrica. 2013;8(5):385-91. Doi: 10.1111/j.2047-6310.2012.00111.x.
Huang LL, Dou DM, Liu N, et al. Association of erythrocyte parameters with metabolic syndrome in the Pearl River Delta region of China: a cross sectional study. BMJ Open. 2018;8(1):e019792. Doi: 10.1136/bmjopen-2017-019792.
Osadnik T, Bujak K, Osadnik K, et al. Novel inflammatory biomarkers may reflect subclinical inflammation in young healthy adults with obesity. Endokrynol Pol. 2019;70(2):135-42. Doi: 10.5603/EP.a2019.0002.
Marginean CO, Melit LE, Ghiga DV, et al. Estado inflamatorio temprano relacionado con la obesidad pediátrica. Front Pediatr. 2019;7:241. Doi: 10.3389/fped.2019.00241.
Singer K, Lumeng CN. El inicio de la inflamación metabólica en la obesidad infantil. J Clin Invest. 2017;127(1):65-73. Doi: 10.1172/JCI88882.
Laufer Perl M, Havakuk O, Finkelstein A, et al. High red blood cell distribution width is associated with the metabolic syndrome. Hemorreología clínica y microcirculación. 2015;63(1):35-43. Doi: 10.3233/CH-151978.
Vuong J, Qiu Y, La M, et al. Reference intervals of complete blood count constituents are highly correlated to waist circumference: should obese patients have their own "normal values?". Revista americana de hematología. 2014;89(7):671-7. Doi: 10.1002/ajh.23713.
Vaya A, Alis R, Hernandez-Mijares A, et al. La anchura de distribución de los hematíes no se relaciona con parámetros inflamatorios en pacientes con obesidad mórbida. Bioquímica clínica. 2014;47(6):464-6. Doi: 10.1016/j.clinbiochem.2014.01.020.
Wang YY, Lin SY, Liu PH, et al. Association between hematological parameters and metabolic syndrome components in a Chinese population. J Diabetes Complications. 2004;18(6):322-7. Doi: 10.1016/S1056-8727(04)00003-0.
Aguilar-Gómez FJ, Bueno-Lozano G, Leis R, et al. Síndrome metabólico antes de la pubertad: ¿Mito o realidad? Curr Opin Endocr Metab Res. 2020;14:97-103. Doi: https://doi.org/10.1016/j.coemr.2020.06.006.
Hardin AP, Hackell JM, Committee On P, et al. Límite de edad de la pediatría. Pediatrics. 2017;140(3). Doi: 10.1542/peds.2017-2151.
Vinciguerra F, Tumminia A, Baratta R, et al. Prevalence and Clinical Characteristics of Children and Adolescents with Metabolically Healthy Obesity: Role of Insulin Sensitivity. Life (Basilea). 2020;10(8). Doi: 10.3390/life10080127.
Damanhoury S, Newton AS, Rashid M, et al. Definición de obesidad metabólicamente saludable en niños: una revisión de alcance. Obes Rev. 2018;19(11):1476-91. Doi: 10.1111/obr.12721.
Cohen J. Statistical power analysis for the behavioral sciences. Hillsdale, NJ: Lawrence Erlbaum; 1988.
Barazzoni R, Gortan Cappellari G, Semolic A, et al. The association between hematological parameters and insulin resistance is modified by body mass index - results from the North-East Italy MoMa population study. PLoS One. 2014;9(7):e101590. Doi: 10.1371/journal.pone.0101590.
Damanhoury S, Morrison KM, Mian R, et al. Metabolically healthy obesity in children enrolled in the CANadian Pediatric Weight management Registry (CANPWR): An exploratory secondary analysis of baseline data. Clin Obes. 2021:e12490. Doi: 10.1111/cob.12490.
Vaya A, Alis R, Hernandez-Mijares A, et al. Reply to "The association of red blood cell distribution width and morbid obesity" by Aydin et al. Clinical biochemistry. 2014;47(13-14):1350. Doi: 10.1016/j.clinbiochem.2014.07.006.
Abdel-Moneim A, Zanaty MI, El-Sayed A, et al. Relation Between Oxidative Stress and Hematologic Abnormalities in Children With Type 1 Diabetes. Can J Diabetes. 2020;44(3):222-8. Doi: 10.1016/j.jcjd.2019.07.153.
Syauqy A, Hsu CY, Rau HH, et al. Asociación de patrones dietéticos, medidas antropométricas y parámetros metabólicos con la proteína C reactiva y la relación neutrófilos-linfocitos en adultos de mediana edad y mayores con síndrome metabólico en Taiwán: un estudio transversal. Nutr J. 2018;17(1):106. Doi: 10.1186/s12937-018-0417-z.
Bahadir A, Baltaci D, Turker Y, et al. Is the neutrophil-to-lymphocyte ratio indicative of inflammatory state in patients with obesity and metabolic syndrome? Anatol J Cardiol. 2015;15(10):816-22. Doi: 10.5152/akd.2014.5787.
Anik A, Celik E, Anik A. The Relation of Complete Blood Count Parameters with Metabolic and Clinical Parameters in Overweight and Obese Children. J Pediatr Res. 2021;8(2):161-70. Doi: 10.4274/jpr.galenos.2020.74824.
Türkkan E, Dag NÇ, Arabaci Ç, et al. Evaluation of Inflammatory Hematological Ratios (NLR, PLR, MLR and Monocyte/HDL-Cholesterol Ratio) in Obese Adolescents. Iberoam J Med. 2022;4(1):11-7. Doi: http://dx.doi.org/10.53986/ibjm.2022.0002.
Santos C, Picoito J, Teixeira AL, et al. Platelet to Lymphocyte Ratio and Homeostasis Model Assessment of Insulin Resistance in Pediatric Obesity and Overweight. Rev Port Endocrinol Diabetes Metab. 2017;12(2):177-82. Doi: https://dx.doi.org/10.1016/j.rpedm.2016.10.041.
Erdal E, Inanir M. Platelet-to-lymphocyte ratio (PLR) and Plateletcrit (PCT) in young patients with morbid obesity. Rev Assoc Med Bras (1992). 2019;65(9):1182-7. Doi: 10.1590/1806-9282.65.9.1182.
Akboga MK, Canpolat U, Yuksel M, et al. Platelet to lymphocyte ratio as a novel indicator of inflammation is correlated with the severity of metabolic syndrome: A single center large-scale study. Platelets. 2016;27(2):178-83. Doi: 10.3109/09537104.2015.1064518.
Pizano-Zarate ML, Horta-Baas G, Nunez-Hernandez JA, et al. Prevalencia y características del fenotipo obeso metabólicamente sano en niños y adolescentes de un estado mexicano. Endocrinol Diabetes Nutr (Engl Ed). 2020;67(10):625-35. Doi: 10.1016/j.endinu.2020.03.015.
Marin-Echeverri C, Aristizabal JC, Gallego-Lopera N, et al. Cardiometabolic risk factors in preschool children with abdominal obesity from Medellin, Colombia. J Pediatr Endocrinol Metab. 2018;31(11):1179-89. Doi: 10.1515/jpem-2018-0140.
Shashaj B, Bedogni G, Graziani MP, et al. Origin of cardiovascular risk in overweight preschool children: a cohort study of cardiometabolic risk factors at the onset of obesity. JAMA Pediatr. 2014;168(10):917-24. Doi: 10.1001/jamapediatrics.2014.900.
Guzzetti C, Ibba A, Casula L, et al. Cardiovascular Risk Factors in Children and Adolescents With Obesity: Sex-Related Differences and Effect of Puberty. Front Endocrinol (Lausana). 2019;10:591. Doi: 10.3389/fendo.2019.00591.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Revista de la Facultad de Medicina Humana

This work is licensed under a Creative Commons Attribution 4.0 International License.