Assessment of Mycobacterium Tuberculosis drug-resistance patterns in a public hospital of Lima, Peru during 2022
Evaluación de los patrones de farmacorresistencia de Mycobacterium Tuberculosis en un hospital público de Lima, Perú durante 2022
DOI:
https://doi.org/10.25176/RFMH.v23i3.5815Keywords:
Tuberculosis, Mycobacterium tuberculosis, Drug Resistance, InfectionsAbstract
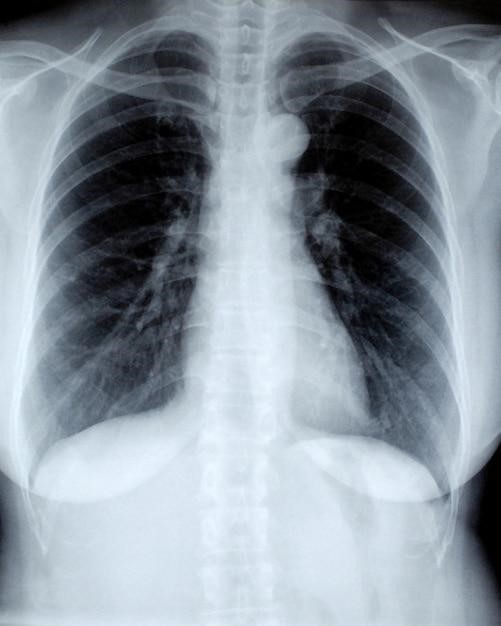
Background. Tuberculosis is a public health problem considered to be the world's leading cause of death from an infectious disease among adults. Diagnosis is often challenging and is based on clinical, epidemiological, radiological, bacteriological, histological and biochemical findings. Timely diagnosis, identification of the susceptibility profile and follow-up compliance is important to enable more effective treatment and avoid severe forms of the disease.
Aim. Describe the resistance patterns of Mycobacterium tuberculosis identified in the period of the year 2022 at Hospital María Auxiliadora.
Material and Methods. This is an observational, cross-sectional study of patients diagnosed with tuberculosis throughout the year 2022 in the Tuberculosis Center of Excellence (TB COE), division of the respiratory medicine department at the Hospital Maria Auxiliadora, Lima, Peru. Data was collected from the medical records which was then included for the statistical analysis. The clinical and demographic characteristics were described by absolute frequencies and percentages. Chi-square test and Fisher's exact test were used to evaluate the association between the sensitivity profile of tuberculosis and the independent variables. A p-value < 0.05 was considered as statistically significant.
Results. A total of 261 medical records were included in the present study. The most frequent age group was 17-59 years old, the majority were male (62.1%) and 15.7% were relapses, as established on national technical standard. Of the total, 89.7% were sensitive to first line drugs; 6.1% of the patients were multidrug-resistant (MDR), and 0.8% presented extensively drug-resistance (XDR); likewise, 0.8% and 2.7% presented resistance for rifampicin only and resistance for isoniazid only respectively. HIV infection was found at 14.2%. The most common form of tuberculosis was pulmonary (49%) followed by pleural tuberculosis (21.8%).
Conclusion. Tuberculosis is a worldwide condition whose drug-resistance patterns continue evolving. However, in our hospital, a southern Peru reference Center, most TB patients are still sensitive to first line drugs. Only a small amount of MDR and XDR patients were found. Moreover, the most common clinical presentation was pulmonary followed by pleural tuberculosis.
Downloads
References
Fukunaga R, Glaziou P, Harris JB, Date A, Floyd K, Kasaeva T. Epidemiology of Tuberculosis and Progress Toward Meeting Global Targets - Worldwide, 2019. 2021;70(12).
Visca D, Ong CWM, Tiberi S, Centis R, D'Ambrosio L, Chen B, et al. Tuberculosis and COVID-19 interaction: A review of biological, clinical and public health effects. Pulmonology [Internet]. 2021 Mar [citado 2023 Apr 28];27(2):151-65. Disponible en: https://linkinghub.elsevier.com/retrieve/pii/S2531043721000040
Ranzani OT, Pescarini JM, Martinez L, Garcia-Basteiro AL. Increasing tuberculosis burden in Latin America: an alarming trend for global control efforts. BMJ Glob Health [Internet]. 2021 Mar [citado 2023 Apr 28];6(3):e005639. Disponible en: https://gh.bmj.com/lookup/doi/10.1136/bmjgh-2021-005639
Walter KS, Martinez L, Arakaki-Sanchez D, Sequera VG, Estigarribia Sanabria G, Cohen T, et al. The escalating tuberculosis crisis in central and South American prisons. The Lancet [Internet]. 2021 abr [citado 2023 abr 28];397(10284):1591-6. Disponible en: https://linkinghub.elsevier.com/retrieve/pii/S0140673620325782
OMS. WHO global list of high burden countries for tuberculosis (TB), TB/HIV and multidrug/rifampicin-resistant TB (MDR/RR-TB), 2021-2025 [Internet]. 2021. Disponible en: https://cdn.who.int/media/docs/default-source/hq-tuberculosis/who_globalhbcliststb_2021-2025_backgrounddocument.pdf?sfvrsn=f6b854c2_9
OMS. Informe mundial sobre la tuberculosis 2022 [Internet]. 2022. Disponible en: https://www.who.int/publications/i/item/9789240061729
Rumende CM. Risk Factors for Multidrug-resistant Tuberculosis. Indones J Intern Med [Internet]. 2018;50. Disponible en: https://www.actamedindones.org/index.php/ijim/article/view/785/296
Hameed S, Ahmad SR, Rahman MA ur, Nazir H, Ullah I. Drug resistance profile of Mycobacterium tuberculosis and predictors associated with the development of drug resistance. Revista de resistencia antimicrobiana global [Internet]. 2019 Sep [citado 2023 Apr 28];18:155-9. Disponible en: https://linkinghub.elsevier.com/retrieve/pii/S2213716519300785
Goossens SN, Sampson SL, Van Rie A. Mechanisms of Drug-Induced Tolerance in Mycobacterium tuberculosis. Clin Microbiol Rev [Internet]. 2020 dic 16 [citado 2023 abr 28];34(1):e00141-20. Disponible en: https://journals.asm.org/doi/10.1128/CMR.00141-20
Liu Z, Klümper U, Liu Y, Yang Y, Wei Q, Lin JG, et al. Metagenomic and metatranscriptomic analyses reveal activity and hosts of antibiotic resistance genes in activated sludge. Medio ambiente internacional [Internet]. 2019 Aug [citado 2023 Apr 28];129:208-20. Disponible en: https://linkinghub.elsevier.com/retrieve/pii/S0160412019307603
OMS. Global Health Expediture Database (GHED) [Internet]. 2022. Disponible en: https://apps.who.int/nha/database
Ahmad M, Khan AU. Global economic impact of antibiotic resistance: A review. Revista de resistencia antimicrobiana global [Internet]. 2019 Dec [citado 2023 Apr 28];19:313-6. Disponible en: https://linkinghub.elsevier.com/retrieve/pii/S2213716519301341
Lohiya A, Suliankatchi Abdulkader R, Rath RS, Jacob O, Chinnakali P, Goel AD, et al. Prevalence and patterns of drug resistant pulmonary tuberculosis in India-A systematic review and meta-analysis. Journal of Global Antimicrobial Resistance [Internet]. 2020 Sep [citado 2023 Apr 28];22:308-16. Disponible en: https://linkinghub.elsevier.com/retrieve/pii/S2213716520300722
Ahmad S, Mokaddas E, Al-Mutairi NM. Prevalence of tuberculosis and multidrug resistant tuberculosis in the Middle East Region. Revisión experta de terapia antiinfecciosa [Internet]. 2018 Sep 2 [citado 2023 Apr 28];16(9):709-21. Available from: https://www.tandfonline.com/doi/full/10.1080/14787210.2018.1519393
Tengan FM, Figueiredo GM, Leite OH, Nunes AK, Manchiero C, Dantas BP, et al. Prevalence of multidrug-resistant tuberculosis in Latin America and the Caribbean: a systematic review and meta-analysis. Trop Med Int Health [Internet]. 2020 Sep [citado 2023 Apr 28];25(9):1065-78. Disponible en: https://onlinelibrary.wiley.com/doi/10.1111/tmi.13453
Furin J, Cox H, Pai M. Tuberculosis. The Lancet [Internet]. 2019 Apr [citado 2023 Apr 28];393(10181):1642-56. Disponible en: https://linkinghub.elsevier.com/retrieve/pii/S0140673619303083
Wang DM, Li Q feng, Zhu M, Xu YH, Liao Y. Clinical characteristics, common sites and drug resistance profile in culture-confirmed extrapulmonary TB/HIV co-infection patients, Southwest China. Journal of Global Antimicrobial Resistance [Internet]. 2022 [citado 2023 Apr 16];28:1-7. Disponible en: https://linkinghub.elsevier.com/retrieve/pii/S2213716521002721
Bonin CR, Fochat RC, Leite ICG, Pereira TV, Fajardo M de O, Pinto CPG, et al. Análisis de la resistencia a los medicamentos antituberculosos y aspectos sociodemográficos y clínicos de pacientes ingresados en un hospital de referencia. Einstein (São Paulo) [Internet]. 2019 Oct 22 [citado 2023 Apr 16];18:eAO4620. Disponible en: https://journal.einstein.br/article/analysis-of-anti-tuberculosis-drug-resistance-and-sociodemographic-and-clinical-aspects-of-patients-admitted-in-a-referral-hospital/
Thummar PD, Rupani MP. Prevalence and predictors of hazardous alcohol use among tuberculosis patients: The need for a policy on joint tuberculosis-alcohol collaborative activities in India. Alcohol [Internet]. 2020 Aug [citado 2023 Apr 20];86:113-9. Disponible en: https://linkinghub.elsevier.com/retrieve/pii/S074183292030197X
Wigger GW, Bouton TC, Jacobson KR, Auld SC, Yeligar SM, Staitieh BS. The Impact of Alcohol Use Disorder on Tuberculosis: A Review of the Epidemiology and Potential Immunologic Mechanisms. Front Immunol [Internet]. 2022 Mar 31 [citado 2023 Apr 16];13:864817. Disponible en: https://www.frontiersin.org/articles/10.3389/fimmu.2022.864817/full
de Vargas KR, Freitas AA, Azeredo ACV, Silva DR. Prevalencia de tabaquismo y efectos sobre los resultados del tratamiento en pacientes con tuberculosis. Rev Assoc Med Bras [Internet]. 2021 Mar [citado 2023 Abr 20];67(3):406-10. Disponible en: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0104-42302021000400406&tlng=en
Song W mei, Li S jin, Liu J yue, Fu Q, Xu T ting, Tao NN, et al. Impact of alcohol drinking and tobacco smoking on the drug-resistance of newly diagnosed tuberculosis: a retrospective cohort study in Shandong, China, during 2004-2020. BMJ Open [Internet]. 2022 Jul [citado 2023 Apr 16];12(7):e059149. Disponible en: https://bmjopen.bmj.com/lookup/doi/10.1136/bmjopen-2021-059149
Ugarte-Gil CA. Tuberculosis: Un enfoque de Derechos Humanos. 2009; Disponible en: http://www.scielo.org.pe/pdf/amp/v26n1/a12v26n1.pdf
Sultana ZZ, Hoque FU, Beyene J, Akhlak-Ul-Islam Md, Khan MHR, Ahmed S, et al. HIV infection and multidrug resistant tuberculosis: a systematic review and meta-analysis. BMC Infect Dis [Internet]. 2021 dic [citado 2023 abr 28];21(1):51. Disponible en: https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-020-05749-2
Jeon CY, Murray MB. Diabetes Mellitus Increases the Risk of Active Tuberculosis: A Systematic Review of 13 Observational Studies. Williams B, editor. PLoS Med [Internet]. 2008 Jul 15 [citado 2023 Apr 28];5(7):e152. Disponible en: https://dx.plos.org/10.1371/journal.pmed.0050152
Salindri AD, Kipiani M, Kempker RR, Gandhi NR, Darchia L, Tukvadze N, et al. Diabetes Reduces the Rate of Sputum Culture Conversion in Patients With Newly Diagnosed Multidrug-Resistant Tuberculosis. Foro abierto de enfermedades infecciosas [Internet]. 2016 May 1 [citado 2023 Apr 28];3(3):ofw126. Disponible en: https://academic.oup.com/ofid/article/doi/10.1093/ofid/ofw126/2593268
Hamada Y, Getahun H, Tadesse BT, Ford N. HIV-associated tuberculosis. Int J STD AIDS [Internet]. 2021 Aug [citado 2023 Apr 28];32(9):780-90. Available from: http://journals.sagepub.com/doi/10.1177/0956462421992257
op LG, Department of Obstetrics and Gynecology, Alessandrescu-Rusescu National Institute for Mother and Child Health, Bucarest, Rumanía, * Corresponding Author: Lucian Pop, MD, Departamento de Obstetricia y Ginecología, Instituto Nacional Alessandrescu-Rusescu de Salud Materno-Infantil, Bucarest, Rumanía. Teléfono: +40741044720 Correo electrónico: popluciangh@icloud.com, Bacalbasa N, Departamento de Obstetricia y Ginecología, Instituto Nacional Alessandrescu-Rusescu de Salud Maternoinfantil, Bucarest, Rumanía, Centro de Excelencia en Medicina Traslacional, Instituto Clínico Fundeni, Bucarest, Rumanía, et al. Tuberculosis in pregnancy. JMedLife [Internet]. 2021 Mar [citado 2023 Apr 28];14(2):165-9. Disponible en: https://medandlife.org/wp-content/uploads/6.-jml-2021-0001.pdf
Hussein MM, Mooij JM, Roujouleh H. Tuberculosis and Chronic Renal Disease: TB AND CHRONIC RENAL DISEASE. Seminars in Dialysis [Internet]. 2003 Jan 20 [citado 2023 Apr 28];16(1):38-44. Available from: http://doi.wiley.com/10.1046/j.1525-139X.2003.03010.x
Luczynski P, Poulin P, Romanowski K, Johnston JC. Tuberculosis and risk of cancer: A systematic review and meta-analysis. Duell EJ, editor. PLoS ONE [Internet]. 2022 Dec 30 [citado 2023 Apr 28];17(12):e0278661. Disponible en: https://dx.plos.org/10.1371/journal.pone.0278661
Chiang SS, Brooks MB, Jenkins HE, Rubenstein D, Seddon JA, van de Water BJ, et al. Concordance of Drug-resistance Profiles Between Persons With Drug-resistant Tuberculosis and Their Household Contacts: A Systematic Review and Meta-analysis. Enfermedades Infecciosas Clínicas [Internet]. 2021 Jul 15 [citado 2023 Apr 28];73(2):250-63. Disponible en: https://academic.oup.com/cid/article/73/2/250/5843623
Bayona J, Chavez-Pachas AM, Palacios E, Llaro K, Sapag R, Becerra MC. La investigación de contactos como medio de detección y tratamiento oportuno de personas con tuberculosis infecciosa multirresistente.
Parr JB, Mitnick CD, Atwood SS, Chalco K, Bayona J, Becerra MC. Concordance of Resistance Profiles in Households of Patients With Multidrug-Resistant Tuberculosis. Enfermedades Infecciosas Clínicas [Internet]. 2014 Feb 1 [citado 2023 Apr 28];58(3):392-5. Disponible en: https://academic.oup.com/cid/article-lookup/doi/10.1093/cid/cit709
Velen K, Shingde R, Ho J, Fox G. The effectiveness of contact investigation among contacts of tuberculosis patients: a systematic review and meta-analysis. European Respiratory Journal [Internet]. 2021;58. Disponible en: https://erj.ersjournals.com/content/58/6/2100266
Osei E, Oppong S, Der J. Trends of tuberculosis case detection, mortality and co-infection with HIV in Ghana: A retrospective cohort study. Spigelman M, editor. PLoS ONE [Internet]. 2020 Jun 24 [citado 2023 Apr 28];15(6):e0234878. Disponible en: https://dx.plos.org/10.1371/journal.pone.0234878
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Revista de la Facultad de Medicina Humana

This work is licensed under a Creative Commons Attribution 4.0 International License.



































