SOLITARY FIBROUS TUMOR OF THE BRAIN: A CASE REPORT
TUMOR FIBROSO SOLITARIO CEREBRAL: A PROPÓSITO DE UN CASO
Keywords:
Solitary Fibrous Tumors, Brain Neoplasms, Central Nervous System NeoplasmsAbstract
Introduction: Solitary fibrous tumors (SFTs) are rare mesenchymal neoplasms that, although typically develop in the visceral pleura, occasionally occur in the intracranial cavity. Furthermore, they are characterized by high rates of metastasis and recurrence.
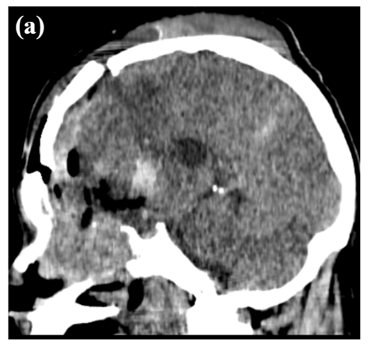
Case Report: We present the case of a 59-year-old male patient with a 3-month history of headache and bradyphrenia. Computed tomography revealed a neoformative tumor infiltrating the nasal cavity, ethmoid sinuses, and anterior cranial fossa, involving the left frontal lobe. The patient underwent two exploratory craniectomies, during which diagnoses suggestive of high-grade glial neoplasia and SFT were made. For precise diagnosis, immunohistochemistry was performed, which was consistent with solitary fibrous tumor. The case is analyzed, focusing particularly on histopathological aspects, the unusual location of this tumor, and its variable clinical manifestations.
Downloads
References
Sun LJ, Dong J, Gao F, Chen DM, Li K, Liu J, et al. Intracranial solitary fibrous tumor: Report of two cases. Medicine (Baltimore). 2019;98(17):e15327. doi: https://doi.org/10.1097/md.0000000000015327
Lee JH, Jeon SH, Park CK, Park SH, Yoon HI, Chang JH, et al. The Role of Postoperative Radiotherapy in Intracranial Solitary Fibrous Tumor/Hemangiopericytoma: A Multi-institutional Retrospective Study (KROG 18-11). Cancer Res Treat Off J Korean Cancer Assoc. 2022;54(1):65-74. doi: https://doi.org/10.4143/crt.2021.142
El-Abtah ME, Murayi R, Ejikeme T, Ahorukomeye P, Petitt JC, Soni P, et al. A Single-Center Retrospective Analysis of Intracranial and Spinal Solitary Fibrous Tumor/Hemangiopericytoma Clinical Outcomes: Sex Association With Aggressiveness. World Neurosurg. 2023;169:e190-6. doi: https://doi.org/10.1016/j.wneu.2022.10.092
Sahoo N, Mohapatra D, Panigrahi S, Lenka A, Das P, Mohapatra SS. Intracranial Solitary Fibrous Tumor/Hemangiopericytoma: A Clinicoradiological Poorly Recognized Entity- An Institutional Experience. Turk Neurosurg. 2020. doi: http://dx.doi.org/10.5137/1019-5149.JTN.31204-20.2
Gunasekaran A, Santos JM, Vandergrift WA. Supraorbital Craniotomy for Sellar Solitary Fibrous Tumor: Operative Technique and Literature Review. World Neurosurg. 2020;141:395-401. doi: https://doi.org/10.1016/j.wneu.2020.06.108
Singh N, Collingwood R, Eich ML, Robinson A, Varambally S, Al Diffalha S, et al. NAB2-STAT6 Gene Fusions to Evaluate Primary/Metastasis of Hemangiopericytoma/Solitary Fibrous Tumors. Am J Clin Pathol. 2021; 156(5):906-912. doi: https://doi.org/10.1093/ajcp/aqab045
Lu C, Alex D, Benayed R, Rosenblum MK, Hameed MR. Solitary Fibrous Tumor with Neuroendocrine and Squamous Dedifferentiation: A Potential Diagnostic Pitfall. Hum Pathol. 2018;77:175. doi: https://doi.org/10.1016%2Fj.humpath.2017.12.024
Louis DN, Perry A, Reifenberger G, von Deimling A, Figarella-Branger D, Cavenee WK, et al. The 2016 World Health Organization Classification of Tumors of the Central Nervous System: a summary. Acta Neuropathol. 2016;131(6):803-820. doi: https://doi.org/10.1007/s00401-016-1545-1
Chmielecki J, Crago AM, Rosenberg M, O’Connor R, Walker SR, Ambrogio L, et al. Whole-exome sequencing identifies a recurrent NAB2-STAT6 fusion in solitary fibrous tumors. Nat Genet. 2013;45(2):131-2. doi: https://doi.org/10.1038/ng.2522
Macagno N, Vogels R, Appay R, Colin C, Mokhtari K, Consortium FCS, et al. Grading of meningeal solitary fibrous tumors/hemangiopericytomas: analysis of the prognostic value of the Marseille Grading System in a cohort of 132 patients. Brain Pathol. 2019;29(1):18-27. doi: https://doi.org/10.1111/bpa.12613
Gubian A, Ganau M, Cebula H, Todeschi J, Scibilia A, Noel G, et al. Intracranial Solitary Fibrous Tumors: A Heterogeneous Entity with an Uncertain Clinical Behavior. World Neurosurg. 2019;126:e48-56. doi: https://doi.org/10.1016/j.wneu.2019.01.142
Fargen KM, Opalach KJ, Wakefield D, Jacob RP, Yachnis AT, Lister JR. The central nervous system solitary fibrous tumor: A review of clinical, imaging and pathologic findings among all reported cases from 1996 to 2010. Clin Neurol Neurosurg. 2011;113(9):703-10. doi: https://doi.org/10.1016/j.wneu.2019.01.142
Towner JE, Johnson MD, Li YM. Intraventricular Hemangiopericytoma: A Case Report and Literature Review. World Neurosurg. 2016;89:728.e5-728.e10. doi: https://doi.org/10.1016/j.wneu.2016.01.056
Bi WL, Santagata S. Skull Base Tumors: Neuropathology and Clinical Implications. Neurosurgery. 2022;90(3):243. doi: https://doi.org/10.1093/neuros/nyab209
He W, Xiao X, Li X, Guo Y, Guo L, Liu X, et al. Whole-tumor histogram analysis of apparent diffusion coefficient in differentiating intracranial solitary fibrous tumor/hemangiopericytoma from angiomatous meningioma. Eur J Radiol. 2019;112:186-91. doi: https://doi.org/10.1016/j.ejrad.2019.01.023
Xiao D, Shi J, Zhou M, Yan L, Zhao Z, Hu T, et al. Tumor volume and the dural tail sign enable the differentiation of intracranial solitary fibrous tumor/hemangiopericytoma from high-grade meningioma. Clin Neurol Neurosurg. 2021;207:106769. doi: https://doi.org/10.1016/j.clineuro.2021.106769
Hayenga HN, Bishop AJ, Wardak Z, Sen C, Mickey B. Intraspinal Dissemination and Local Recurrence of an Intracranial Hemangiopericytoma. World Neurosurg. 2019;123:68-75. doi: https://doi.org/10.1016/j.wneu.2018.11.173
Mesny E, Lesueur P. Radiotherapy for rare primary brain tumors. Cancer Radiother 2023;27:599–607.doi: https://doi.org/10.1016/j.canrad.2023.06.008
Reames DL, Mohila CA, Sheehan JP. Treatment of intracranial solitary fibrous tumors with gamma knife radiosurgery: Report of two cases and review of literature. Neurosurgery 2011;69:E1023–8. doi: https://doi.org/10.1227/neu.0b013e318223b7e6
Hendrickson Rahmlow T, Kolagatla S, Mattingly K, Grube J, Ganti SS, Moka N. Liver Metastasis From Intracranial Hemangiopericytoma 8 Years After Initial Resection: Case Report. J Investig Med High Impact Case Rep. 2022. doi: https://doi.org/10.1177/2324709622113224
Demicco EG, Wagner MJ, Maki RG, Gupta V, Iofin I, Lazar AJ, et al. Risk assessment in solitary fibrous tumors: validation and refinement of a risk stratification model. Mod Pathol. 2017;30(10):1433-42. doi: https://doi.org/10.1038/modpathol.2017.54
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Revista de la Facultad de Medicina Humana

This work is licensed under a Creative Commons Attribution 4.0 International License.