Pulmonary Aspergillosis, an approach to clinical and radiological manifestations. Report of three cases
Manifestaciones clínicas y radiológicas de la Aspergilosis Pulmonar: Informe de tres casos
DOI:
https://doi.org/10.25176/RFMH.v24i2.6098Keywords:
Aspergillosis Pulmonary, Aspergillus, Immunocompromised Host, Voriconazole, Respiratory Tract InfectionsAbstract
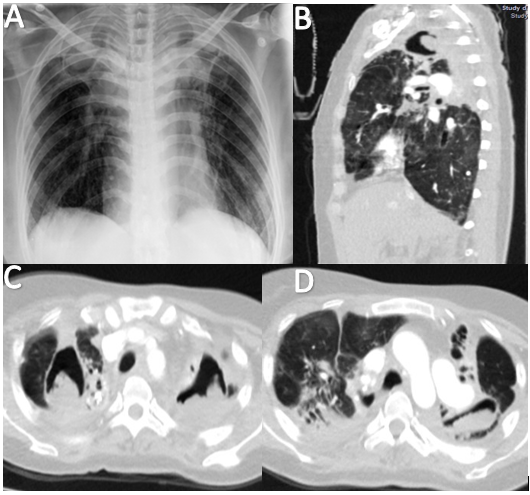
Pulmonary aspergillosis, caused by the opportunistic fungus Aspergillus, primarily affects immunocompromised individuals. This report presents three cases: An 18-year-old female with acute leukemia developed respiratory distress and bilateral "tree-in-bud" patterns on CT. Despite voriconazole treatment, she succumbed to respiratory failure. A 58-year-old female with diabetes and COPD had dyspnea and hemoptysis. Imaging revealed a cavitated lesion, confirming aspergilloma. Surgery was considered due to active hemoptysis. A 41-year-old female with a history of tuberculosis presented with fever and respiratory symptoms. CT showed cavitated lesions and bronchiectasis, confirming chronic aspergillosis. She responded well to voriconazole. These cases highlight the variability in pulmonary aspergillosis and underscore the importance of timely diagnosis and treatment to improve patient outcomes.
Downloads
References
Raper KB, Fennell DI, editors. The genus Aspergillus. Huntington: Robert E. Krieger Pub.; 1973.
Greenberger PA. Allergic bronchopulmonary aspergillosis. J Allergy Clin Immunol. 2002 Nov;110(5):685-92. doi:10.1067/mai.2002.130179
Lortholary O, Ascioglu S, Moreau P, Herbrecht R, Marinus A, Casassus P, et al. Invasive aspergillosis as an opportunistic infection in nonallografted patients with multiple myeloma: a European Organization for Research and Treatment of Cancer/ Invasive Fungal Infections Cooperative Group and the Intergroupe Français du Myélome. Clin Infect Dis. 2000;30(1):41–6. doi:10.1086/313592
Kaiser L, Huguenin T, Lew PD, Chapuis B, Pittet D. Invasive aspergillosis. Clinical features of 35 proven cases at a single institution. Medicine (Baltimore). 1998;77(3):188–94. doi:10.1097/00005792-199805000-00004
Donnelly JP, Chen SC, Kauffman CA, et al. Revision and update of the consensus definitions of invasive fungal disease from the European Organization for Research and Treatment of Cancer and the Mycoses Study Group Education and Research Consortium. Clin Infect Dis. 2020;71(6):1367-76. doi:10.1093/cid/ciz1008
Mercier T, Castagnola E, Marr KA, Wheat LJ, Verweij PE, Maertens JA. Defining galactomannan positivity in the updated EORTC/MSGERC consensus definitions of invasive fungal diseases. Clin Infect Dis. 2021 Mar 12;72(Suppl 2). doi:10.1093/cid/ciaa1786
Koehler P, Bassetti M, Chakrabarti A, Chen SCA, et al. Defining and managing COVID-19-associated pulmonary aspergillosis: the 2020 ECMM/ISHAM consensus criteria for research and clinical guidance. Lancet Infect Dis. 2021;21(6). doi:10.1016/S1473-3099(20)30847-1
McNeil MM, Nash SL, Hajjeh RA, Phelan MA, Conn LA, Plikaytis BD, et al. Trends in mortality due to invasive mycotic diseases in the United States, 1980-1997. Clin Infect Dis. 2001;33(5):641–7. doi:10.1086/322606
Groll AH, Shah PM, Mentzel C, Schneider M, Just-Nuebling G, Huebner K. Trends in the postmortem epidemiology of invasive fungal infections at a university hospital. J Infect. 1996;33(1):23–32. doi:10.1016/s0163-4453(96)92700-0
De Pauw B, Walsh TJ, Donnelly JP, Stevens DA, Edwards JE, Calandra T, et al. Revised definitions of invasive fungal disease from the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) Consensus Group. Clin Infect Dis. 2008;46(12):1813-21. doi:10.1086/588660
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Revista de la Facultad de Medicina Humana

This work is licensed under a Creative Commons Attribution 4.0 International License.