Factors associated with non-attendance at prenatal care in the first and second trimesters of pregnancy in a tertiary-level hospital in Lima, Peru, 2023
Factores asociados a la inasistencia al control prenatal en el primer y segundo trimestre del embarazo en un hospital de tercer nivel de Lima, Perú, 2023
Keywords:
prenatal care, social determinant, pregnancy, trimester.Abstract
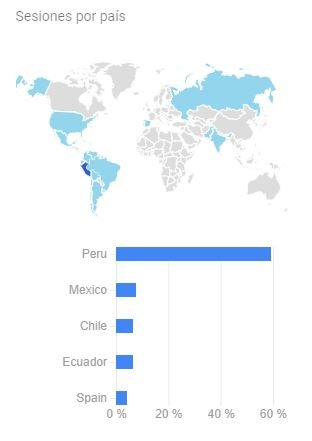
Objective: To compare the factors associated with inadequate prenatal care in the first and second trimesters of pregnancy in women attending the outpatient clinic of the National Maternal Perinatal Institute, a referral hospital in Lima, Peru.
Methodology:
A retrospective analytical cross-sectional study was designed with pregnant women attended at the National Maternal Perinatal Institute in Lima, Peru. The study included 256 pregnant women with more than 26 weeks and 6 days of gestation. Demographic factors, gynecological history, social aspects, and institutional factors related to prenatal care attendance were collected through a questionnaire. Inadequate prenatal care was defined as fewer than 1 visit in the first trimester and fewer than 2 in the second. The strength of association was estimated using a Poisson regression model with a 95% confidence interval and a significance p-value of 0.05.
Results: Multivariate analysis revealed that in the first trimester, single women and those with primary and secondary education had a higher risk of inadequate attendance, as did those attended by midwives and those living far from the hospital. Women with high-risk pregnancies had a lower risk. In the second trimester, the higher risk persisted for single women and those with lower education, but women born in provinces had a lower risk, while those with three or more children had a higher risk of inadequate attendance.
Conclusions: These findings highlight key differences between trimesters in the factors associated with inadequate prenatal attendance.
Keywords: Risk, prenatal care, education, pregnancy, trimester.
Downloads
References
La OMS señala que las embarazadas deben poder tener acceso a una atención adecuada en el momento adecuado [Internet]. [citado 4 de julio de 2024]. Disponible en: https://www.who.int/es/news/item/07-11-2016-pregnant-women-must-be-able-to-access-the-right-care-at-the-right-time-says-who
Huang A, Wu K, Zhao W, Hu H, Yang Q, Chen D. Attendance at prenatal care and adverse birth outcomes in China: A follow-up study based on Maternal and Newborn’s Health Monitoring System. Midwifery. febrero de 2018;57:26-31.
Handler A, Rankin K, Rosenberg D, Sinha K. Extent of documented adherence to recommended prenatal care content: provider site differences and effect on outcomes among low-income women. Matern Child Health J. febrero de 2012;16(2):393-405.
Doku DT, Neupane S. Survival analysis of the association between antenatal care attendance and neonatal mortality in 57 low- and middle-income countries. Int J Epidemiol. 1 de octubre de 2017;46(5):1668-77.
Yan J. The Effects of Prenatal Care Utilization on Maternal Health and Health Behaviors. Health Econ. agosto de 2017;26(8):1001-18.
Nuamah GB, Agyei-Baffour P, Mensah KA, Boateng D, Quansah DY, Dobin D, et al. Access and utilization of maternal healthcare in a rural district in the forest belt of Ghana. BMC Pregnancy Childbirth. 7 de enero de 2019;19(1):6.
Holcomb DS, Pengetnze Y, Steele A, Karam A, Spong C, Nelson DB. Geographic barriers to prenatal care access and their consequences. Am J Obstet Gynecol MFM. septiembre de 2021;3(5):100442.
Guliani H, Sepehri A, Serieux J. Determinants of prenatal care use: evidence from 32 low-income countries across Asia, Sub-Saharan Africa and Latin America. Health Policy Plan. 1 de agosto de 2014;29(5):589-602.
Kotlar B, Gerson E, Petrillo S, Langer A, Tiemeier H. The impact of the COVID-19 pandemic on maternal and perinatal health: a scoping review. Reprod Health. 18 de enero de 2021;18(1):10.
Esopo K, Derby L, Haushofer J. Interventions to improve adherence to antenatal and postnatal care regimens among pregnant women in sub-Saharan Africa: a systematic review. BMC Pregnancy Childbirth. 24 de mayo de 2020;20(1):316.
Groskaufmanis L, Brunner Huber LR, Vick T. Group Prenatal Visits: Maternal and Neonatal Health Outcomes. J Midwifery Womens Health. 8 de agosto de 2018;
Wilson M, Patterson K, Nkalubo J, Lwasa S, Namanya D, Twesigomwe S, et al. Assessing the determinants of antenatal care adherence for Indigenous and non-Indigenous women in southwestern Uganda. Midwifery. noviembre de 2019;78:16-24.
WHO recommendations on antenatal care for a positive pregnancy experience [Internet]. [citado 14 de junio de 2024]. Disponible en: https://www.who.int/publications/i/item/9789241549912
Recomendaciones para una maternidad saludable [Internet]. 2024 [citado 4 de julio de 2024]. Disponible en: https://www.gob.pe/33919-recomendaciones-para-una-maternidad-saludable
Perú: Encuesta Demográfica y de Salud Familiar, Endes 2023 [Internet]. [citado 4 de julio de 2024]. Disponible en: https://www.gob.pe/institucion/inei/informes-publicaciones/5601739-peru-encuesta-demografica-y-de-salud-familiar-endes-2023
González-Cowes VL, Landini FP. [Adherence to prenatal care in the north of Argentina from a social interface perspective]. Cienc Saude Coletiva. agosto de 2018;23(8):2741-50.
Dioses Fernández DL, Corzo Sosa CA, Zarate García JJ, Vizcarra Gonzales VA, Zapata Maza NG, Arredondo-Nontol M, et al. Adherence to prenatal care in the sociocultural context of developing countries: a narrative review. Horiz Méd Lima [Internet]. octubre de 2023 [citado 2 de julio de 2024];23(4). Disponible en: http://www.scielo.org.pe/scielo.php?script=sci_abstract&pid=S1727-558X2023000400013&lng=en&nrm=iso&tlng=en
Wolf ER, Donahue E, Sabo RT, Nelson BB, Krist AH. Barriers to Attendance of Prenatal and Well-Child Visits. Acad Pediatr. agosto de 2021;21(6):955-60.
Ribeiro ERO, Guimarães AMDN, Bettiol H, Lima DDF, Almeida MLD, de Souza L, et al. Risk factors for inadequate prenatal care use in the metropolitan area of Aracaju, Northeast Brazil. BMC Pregnancy Childbirth. 22 de julio de 2009;9:31.
Kidie AA, Asmamaw DB, Belachew TB, Fetene SM, Baykeda TA, Endawkie A, et al. Socioeconomic inequality in timing of ANC visit among pregnant women in Ethiopia, 2019. Front Public Health [Internet]. 14 de marzo de 2024 [citado 3 de julio de 2024];12. Disponible en: https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2024.1243433/full
Evans NM, Sheu JJ. Validating a path model of adherence to prenatal care recommendations among pregnant women. Patient Educ Couns. julio de 2019;102(7):1350-6.
Puthussery S, Tseng PC, Sharma E, Harden A, Griffiths M, Bamfo J, et al. Disparities in the timing of antenatal care initiation and associated factors in an ethnically dense maternal cohort with high levels of area deprivation. BMC Pregnancy Childbirth. 19 de septiembre de 2022;22(1):713.

Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Revista de la Facultad de Medicina Humana

This work is licensed under a Creative Commons Attribution 4.0 International License.