Hallazgos microscópicos del tejido pulmonar y los músculos respiratorios en la Enfermedad Pulmonar Obstructiva Crónica (EPOC)
Microscopic findings of lung tissue and respiratory muscles in Chronic Obstructive Pulmonary Disease (COPD)
DOI:
https://doi.org/10.25176/RFMH.v20i1.2447Palabras clave:
Enfermedad pulmonar obstructiva crónica, Músculo estriado, Antracosis, Tabaquismo, AutopsiaResumen
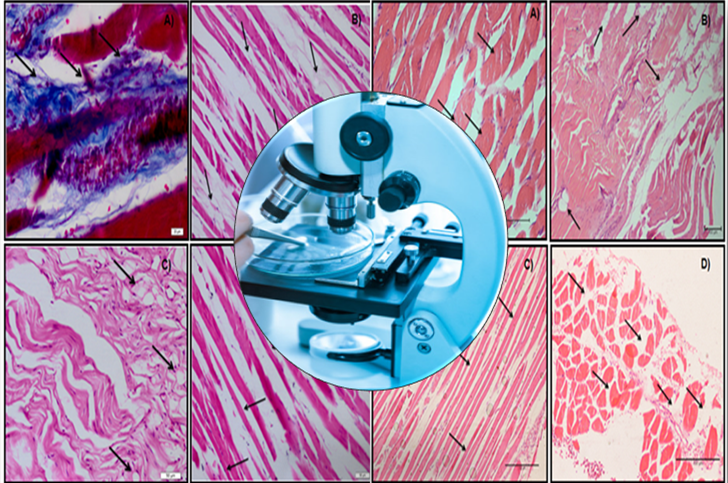
Introducción: En la enfermedad pulmonar obstructiva crónica (EPOC), el diafragma y los músculos respiratorios esternocleidomastoideos (ECOM) funcionan contra el aumento de las cargas mecánicas debido a la limitación del flujo de aire y los cambios en la conformación del tórax debido a la condición de hiperinflación pulmonar. Objetivo: Evaluar los cambios histopatológicos presentes en los pulmones y los músculos respiratorios (diafragma y ECOM) de los cadáveres con Diagnostico de EPOC. El Estudio: Este es un estudio ciego y descriptivo con análisis de imágenes histológicas de biopsia. El historial de tabaquismo asociado con la presencia de antracosis pulmonar, engrosamiento septal y bullas enfisematosas comprendió los criterios de inclusión del estudio. La muestra consistió en biopsias de pulmón, diafragma y ECOM. El estudio se realizó mediante análisis microscópico óptico de lâminas histológicas obtenidas de 36 cadáveres con EPOC. El diagnóstico histopatológico fue realizado por un patólogo que desconocía los objetivos del estudio. Hallazgos: En el diafragma, hubo la presencia de tejido adiposo interpuesto, atrofia muscular, eliminación de las fibras musculares y fibrosis. En el ECOM, también se evidenció la eliminación de las fibras musculares, la atrofia muscular, el tejido adiposo interpuesto, la hipertrofia muscular y el engrosamiento de los tendones. Conclusiones: Los cambios encontrados en las biopsias musculares de diafragma y ECOM de los cadáveres con EPOC se evidenciaron como un mecanismo de compensación y/o disfunción del sistema respiratorio debido a alteraciones biomecánicas promovidas por la enfermedad.
Descargas
Citas
2. MATHERS, C. D.; LONCAR, D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med, v. 3, n. 11, p. e442, Nov 2006. ISSN 1549-1676. Disponível em: < https://www.ncbi.nlm.nih.gov/pubmed/17132052 >.
3. DOURADO, V. Z. et al. Systemic manifestations in chronic obstructive pulmonary disease. J Bras Pneumol, v. 32, n. 2, p. 161-71, 2006 Mar-Apr 2006. ISSN 1806-3756. Disponível em: < https://www.ncbi.nlm.nih.gov/pubmed/17273586 >.
4. SNIDER, G. L. Clinical relevance summary: Collagen vs elastin in pathogenesis of emphysema; cellular origin of elastases; bronchiolitis vs emphysema as a cause of airflow obstruction. Chest, v. 117, n. 5 Suppl 1, p. 244S-6S, May 2000. ISSN 0012-3692. Disponível em: < https://www.ncbi.nlm.nih.gov/pubmed/10843929 >.
5. MENEZES, A. M. et al. Chronic obstructive pulmonary disease in five Latin American cities (the PLATINO study): a prevalence study. Lancet, v. 366, n. 9500, p. 1875-81, Nov 2005. ISSN 1474-547X. Disponível em: < https://www.ncbi.nlm.nih.gov/pubmed/16310554 >.
6. VOGELMEIER, C. F. et al. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Lung Disease 2017 Report. GOLD Executive Summary. Am J Respir Crit Care Med, v. 195, n. 5, p. 557-582, 03 2017. ISSN 1535-4970. Disponível em: < https://www.ncbi.nlm.nih.gov/pubmed/28128970 >.
7. HOGG, J. C.; SENIOR, R. M. Chronic obstructive pulmonary disease - part 2: pathology and biochemistry of emphysema. Thorax, v. 57, n. 9, p. 830-4, Sep 2002. ISSN 0040-6376. Disponível em: < https://www.ncbi.nlm.nih.gov/pubmed/12200530 >.
8. FINKELSTEIN, R. et al. Alveolar inflammation and its relation to emphysema in smokers. Am J Respir Crit Care Med, v. 152, n. 5 Pt 1, p. 1666-72, Nov 1995. ISSN 1073-449X. Disponível em: < https://www.ncbi.nlm.nih.gov/pubmed/7582312 >.
9. STRINGER, K. A. et al. Cigarette smoke extract-induced suppression of caspase-3-like activity impairs human neutrophil phagocytosis. Am J Physiol Lung Cell Mol Physiol, v. 292, n. 6, p. L1572-9, Jun 2007. ISSN 1040-0605. Disponível em: < https://www.ncbi.nlm.nih.gov/pubmed/17351060 >.
10. ABBOUD, R. T. et al. Relationship of alveolar macrophage plasminogen activator and elastase activities to lung function and CT evidence of emphysema. Chest, v. 113, n. 5, p. 1257-63, May 1998. ISSN 0012-3692. Disponível em: < https://www.ncbi.nlm.nih.gov/pubmed/9596303 >.
11. OROZCO-LEVI, M. Structure and function of the respiratory muscles in patients with COPD: impairment or adaptation? Eur Respir J Suppl, v. 46, p. 41s-51s, Nov 2003. ISSN 0904-1850. Disponível em: < https://www.ncbi.nlm.nih.gov/pubmed/14621106 >.
12. NEWELL, S. Z.; MCKENZIE, D. K.; GANDEVIA, S. C. Inspiratory and skeletal muscle strength and endurance and diaphragmatic activation in patients with chronic airflow limitation. Thorax, v. 44, n. 11, p. 903-12, Nov 1989. ISSN 0040-6376. Disponível em: < https://www.ncbi.nlm.nih.gov/pubmed/2595630 >.
13. SIMILOWSKI, T. et al. Contractile properties of the human diaphragm during chronic hyperinflation. N Engl J Med, v. 325, n. 13, p. 917-23, Sep 1991. ISSN 0028-4793. Disponível em: < https://www.ncbi.nlm.nih.gov/pubmed/1881417 >.
14. OTTENHEIJM, C. A.; HEUNKS, L. M.; DEKHUIJZEN, R. P. Diaphragm adaptations in patients with COPD. Respir Res, v. 9, p. 12, Jan 2008. ISSN 1465-993X. Disponível em: < https://www.ncbi.nlm.nih.gov/pubmed/18218129 >.
15. CARDOSO, D. M. et al. Effects of expiratory positive airway pressure on the electromyographic activity of accessory inspiratory muscles in COPD patients. J Bras Pneumol, v. 37, n. 1, p. 46-53, 2011 Jan-Feb 2011. ISSN 1806-3756. Disponível em: < https://www.ncbi.nlm.nih.gov/pubmed/21390431 >.
16. CANÇADO, J. E. et al. [Clinical repercussions of exposure to atmospheric pollution]. J Bras Pneumol, v. 32 Suppl 2, p. S5-11, 2006. ISSN 1806-3756. Disponível em: < https://www.ncbi.nlm.nih.gov/pubmed/17273599 >.
17. CHURG, A. et al. Chronic exposure to high levels of particulate air pollution and small airway remodeling. Environ Health Perspect, v. 111, n. 5, p. 714-8, May 2003. ISSN 0091-6765. Disponível em: < https://www.ncbi.nlm.nih.gov/pubmed/12727599 >.
18. GONZALEZ, M. et al. Images in thorax. Tension pneumothorax mimicking giant emphysematous bullae. Thorax, v. 65, n. 11, p. 1028, Nov 2010. ISSN 1468-3296. Disponível em: < https://www.ncbi.nlm.nih.gov/pubmed/20530117 >.
19. SCOTT, A. et al. Increased injury and intramuscular collagen of the diaphragm in COPD: autopsy observations. Eur Respir J, v. 27, n. 1, p. 51-9, Jan 2006. ISSN 0903-1936. Disponível em: < https://www.ncbi.nlm.nih.gov/pubmed/16387935 >.
20. CLANTON, T. L.; LEVINE, S. Respiratory muscle fiber remodeling in chronic hyperinflation: dysfunction or adaptation? J Appl Physiol (1985), v. 107, n. 1, p. 324-35, Jul 2009. ISSN 8750-7587. Disponível em: < https://www.ncbi.nlm.nih.gov/pubmed/19359619 >.
21. CONTE, M. et al. Differential expression of perilipin 2 and 5 in human skeletal muscle during aging and their association with atrophy-related genes. Biogerontology, v. 16, n. 3, p. 329-40, Jun 2015. ISSN 1573-6768. Disponível em: < https://www.ncbi.nlm.nih.gov/pubmed/25559404 >.
22. KADER, D. F.; WARDLAW, D.; SMITH, F. W. Correlation between the MRI changes in the lumbar multifidus muscles and leg pain. Clin Radiol, v. 55, n. 2, p. 145-9, Feb 2000. ISSN 0009-9260. Disponível em: < https://www.ncbi.nlm.nih.gov/pubmed/10657162 >.
23. ALEXOPOULOU, C. et al. Vascular-specific growth factor mRNA levels in the human diaphragm. Respiration, v. 72, n. 6, p. 636-41, 2005 Nov-Dec 2005. ISSN 0025-7931. Disponível em: < https://www.ncbi.nlm.nih.gov/pubmed/16355005 >.
24. ZHU, E. et al. Diaphragm muscle fiber injury after inspiratory resistive breathing. Am J Respir Crit Care Med, v. 155, n. 3, p. 1110-6, Mar 1997. ISSN 1073-449X. Disponível em: < https://www.ncbi.nlm.nih.gov/pubmed/9116995 >.
25. CHARGÉ, S. B.; RUDNICKI, M. A. Cellular and molecular regulation of muscle regeneration. Physiol Rev, v. 84, n. 1, p. 209-38, Jan 2004. ISSN 0031-9333. Disponível em: < https://www.ncbi.nlm.nih.gov/pubmed/14715915 >.
26. FACTOR, D.; DALE, B. Current concepts of rotator cuff tendinopathy. Int J Sports Phys Ther, v. 9, n. 2, p. 274-88, Apr 2014. ISSN 2159-2896. Disponível em: < https://www.ncbi.nlm.nih.gov/pubmed/24790788 >.
27. WHITTOM, F. et al. Histochemical and morphological characteristics of the vastus lateralis muscle in patients with chronic obstructive pulmonary disease. Med Sci Sports Exerc, v. 30, n. 10, p. 1467-74, Oct 1998. ISSN 0195-9131. Disponível em: < https://www.ncbi.nlm.nih.gov/pubmed/9789845 >.
28. SATTA, A. et al. Fibre types in skeletal muscles of chronic obstructive pulmonary disease patients related to respiratory function and exercise tolerance. Eur Respir J, v. 10, n. 12, p. 2853-60, Dec 1997. ISSN 0903-1936. Disponível em: < https://www.ncbi.nlm.nih.gov/pubmed/9493673 >.
29. HUDSON, A. L.; GANDEVIA, S. C.; BUTLER, J. E. The effect of lung volume on the co-ordinated recruitment of scalene and sternomastoid muscles in humans. J Physiol, v. 584, n. Pt 1, p. 261-70, Oct 2007. ISSN 0022-3751. Disponível em: < https://www.ncbi.nlm.nih.gov/pubmed/17690147 >.
30. ROSENBERG, I. H. Sarcopenia: origins and clinical relevance. Clin Geriatr Med, v. 27, n. 3, p. 337-9, Aug 2011. ISSN 1879-8853. Disponível em: < https://www.ncbi.nlm.nih.gov/pubmed/21824550 >.
Descargas
Publicado
Cómo citar
Número
Sección
Licencia
Derechos de autor 2019 Revista de la Facultad de Medicina Humana

Esta obra está bajo una licencia internacional Creative Commons Atribución 4.0.




































