Report of case of systemic al amyloidosis in a 65-year-old man with chronic diarrhea and hemolacria
Reporte de un caso de amiloidosis sistémica al en un varón de 65 años con diarrea crónica y hemolacria
DOI:
https://doi.org/10.25176/RFMH.v24i2.6534Keywords:
Immunoglobulin Light-chain Amyloidosis, Diarrhea, Eye HemorrhageAbstract
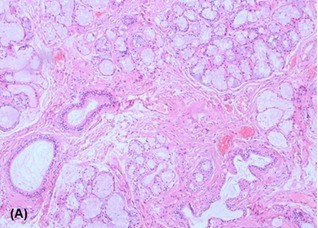
The case of a 65-year-old male with chronic diarrhea, periorbital ecchymosis, and hemolacria is described. Laboratory studies, biopsy, and immunohistochemical analysis were performed to confirm the diagnosis. The dependent variable was the confirmed diagnosis of AL amyloidosis, while the independent variables included clinical symptoms and diagnostic test results. Descriptive techniques were used to analyze the clinical and laboratory data. The patient presented with chronic diarrhea unresponsive to conventional treatment, periorbital ecchymosis, and hemolacria. Diagnostic studies revealed amyloid deposits in the tissues. Immunohistochemical analysis confirmed systemic light chain AL amyloidosis. Specific treatment was initiated, partially improving the symptoms and stabilizing the patient's condition. Systemic AL amyloidosis requires a high index of clinical suspicion for timely diagnosis. The combination of diagnostic studies and early treatment can improve the prognosis of these patients.
Downloads
References
Kumar N, Zhang NJ, Cherepanov D, Romanus D, Hughes M, Faller DV. Global epidemiology of amyloid light-chain amyloidosis. Orphanet J Rare Dis. 2022;17(1):278. doi:10.1186/s13023-022-02414-6
Baker KR. Light Chain Amyloidosis: Epidemiology, Staging, and Prognostication. Methodist Debakey Cardiovasc J. 18(2):27–35. doi:10.14797/mdcvj.1070
Elsayed M, Usher S, Habib MH, Ahmed N, Ali J, Begemann M, et al. Current Updates on the Management of AL Amyloidosis. J Hematol. 2021;10(4):147–61. doi:10.14740/jh866
Picken MM. The Pathology of Amyloidosis in Classification: A Review. Acta Haematol. 2020;143(4):322–34. doi:10.1159/000506696
Bal S, Landau H. AL amyloidosis: untangling new therapies. Hematology Am Soc Hematol Educ Program. 2021;2021(1):682–8. doi:10.1182/hematology.2021000305
Zanwar S, Gertz MA, Muchtar E. Immunoglobulin Light Chain Amyloidosis: Diagnosis and Risk Assessment. J Natl Compr Canc Netw. 2023;21(1):83-90. doi:10.6004/jnccn.2022.7077
Gertz MA, Dispenzieri A. Reconocimiento, pronóstico y tratamiento de la amiloidosis sistémica: una revisión sistemática. JAMA. 2020;324(1):79–89. doi:10.1001/jama.2020.5493
McCausland KL, White MK, Guthrie SD, et al. Light Chain (AL) Amyloidosis: The Journey to Diagnosis. Patient. 2018;11(3):207–216. doi:10.1007/s40271-017-0273-5
Stelmach-Gołdyś A, Zaborek-Łyczba M, Łyczba J, Garus B, Pasiarski M, Mertowska P, et al. Physiology, Diagnosis and Treatment of Cardiac Light Chain Amyloidosis. J Clin Med. 2022;11(4):911. doi:10.3390/jcm11040911
Dahiya DS, Kichloo A, Singh J, Albosta M, Wani F. Gastrointestinal amyloidosis: A focused review. World J Gastrointest Endosc. 2021;13(1):1-12. doi:10.4253/wjge.v13.i1.1
Nicol M, Siguret V, Vergaro G, Aimo A, Emdin M, Dillinger JG, et al. Thromboembolism and bleeding in systemic amyloidosis: a review. ESC Heart Failure. 2022;9(1):11–20. doi:10.1002/ehf2.13701
Thompson CA, Kyle R, Gertz M, Heit J, Pruthi R, Pardanani A. Systemic AL amyloidosis with acquired factor X deficiency: a study of perioperative bleeding risk and treatment outcomes in 60 patients. Am J Hematol. 2010;85(3):171–173. doi:10.1002/ajh.21603
Di Nunzio D, Recupero A, de Gregorio C, Zito C, Carerj S, Di Bella G. Echocardiographic findings in cardiac amyloidosis: inside two-dimensional, Doppler, and strain imaging. Curr Cardiol Rep. 2019;21(2):7. doi:10.1007/s11886-019-1094-z
Li T, Huang X, Cheng S, et al. Utility of abdominal skin plus subcutaneous fat and rectal mucosal biopsy in the diagnosis of AL amyloidosis with renal involvement. PLoS ONE. 2017;12(9). doi:10.1371/journal.pone.0185078
Ikura H, Endo J, Kitakata H, Moriyama H, Sano M, Fukuda K. Molecular mechanism of pathogenesis and treatment strategies for AL amyloidosis. Int J Mol Sci. 2022;23(11):6336. doi:10.3390/ijms23116336
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Revista de la Facultad de Medicina Humana

This work is licensed under a Creative Commons Attribution 4.0 International License.